All published articles of this journal are available on ScienceDirect.
Friction or Frictionless: What is the Most Effective Method for Retracting Anterior Teeth?
Abstract
Objective
To evaluate the effectiveness of the friction-based (sliding mechanism with elastomeric chains) and frictionless (T-loop) methods for retracting anterior teeth in Angle Class I malocclusion.
Methods
This clinical intervention study examined the duration of maxillary incisor retraction from August 2022 to August 2024 in 42 adult patients who had completed canine retraction. The process involved resolving horizontal and vertical discrepancies, establishing a Class I relationship between the canines, and altering the overbite (the interproximal space between the lateral incisors and canines) until an ideal overbite index of 2 mm was achieved. Cone beam computed tomography (CBCT) was conducted before and after retraction to evaluate alveolar changes and speed.
Result
The maxillary central incisors advanced 1.2 mm more in the sliding mechanism cohort than in the loop mechanism cohort (0.18 mm) (p < 0.001). The angle between the central incisor axis and the palatal plane decreased by 12.57° with sliding mechanics, which was significantly greater than the 9.65° decrease observed with the loop mechanism (p = 0.014). After retraction, the location of maxillary tooth roots changed, with the length of incisor roots decreasing by 1 mm and 0.81 mm in the central incisors and 0.67 mm and 0.61 mm in the lateral incisors, respectively (p > 0,05).
Conclusion
Following treatment, frictionless (T-loop) procedures generally provided superior control over the torque and extrusion of the incisors during retraction and were more efficient. However, root resorption rates were comparable between the frictionless and friction (sliding mechanism with elastomeric chains) groups.
Clinical Trial Registration
It is registered in the ClinicalTrials.gov with ClinicalTrials.gov ID: NCT06928896.
1. INTRODUCTION
The objective of malocclusion therapy is to achieve a harmonious, attractive, and stable functional occlusion. The ongoing evolution of archwire and bracket systems has enhanced biomechanical frameworks in the treatment process [1-3]. Professionals often debate the longest phase of orthodontic therapy: the retraction of incisors after tooth extraction. The retraction of the four incisors in the two-stage retraction procedure after premolar extraction is executed using two methods: the sliding mechanism (friction) and the loop mechanism (frictionless) methods [4, 5]. While friction mechanics are simple and widely used, they can cause unwanted tipping or rotation of the anterior teeth. By contrast, frictionless mechanics provide superior control over the movement of the anterior teeth. However, small mistakes in loop design can lead to significant differences in tooth movement, and some patients may find the loops uncomfortable [5]. The existing literature on the effects of friction versus frictionless mechanics on speed, tooth root length, and changes in axis is limited. This underscores the need for well-designed studies to draw definitive conclusions and provide valuable insights into the effectiveness of different mechanical approaches on alveolar bone changes. The knowledge gained from such studies would enable orthodontists to choose the most appropriate treatment mechanics, ultimately enhancing patient satisfaction and compliance throughout the treatment process. Prioritizing this research is essential for advancing orthodontic care and improving overall patient outcomes. Therefore, this study evaluated the effectiveness of the friction-based (sliding mechanism with elastomeric chains) and frictionless (T-loop) methods for retracting anterior teeth in Angle Class I malocclusion.
2. MATERIALS AND METHODS
2.1. Study Participants
2.1.1. Inclusion Criteria
Age ≥16 years, Angle Class I malocclusion on one or both sides, no previous orthodontic treatment, indications for fixed appliances and premolar extraction to create space during treatment, and consent to participate in the study.
2.1.2. Exclusion Criteria
History of craniofacial traumas, anomalies, congenital disabilities, or systemic diseases related to osteogenic metabolism (e.g., diabetes mellitus, kidney diseases, and osseous diseases); use of anticoagulant drugs that affect bone metabolism (e.g., heparin, warfarin, NSAIDs, cyclosporine, glucocorticoids, medroxyprogesterone acetate, etc.); the presence of mini-screws; and history of hook failure.
2.2. Study Methods
This interventional trial enrolled 42 patients, dividing them into two groups: in group 1, the friction (sliding mechanism with elastomeric chains) method was used, and in group 2, the frictionless (T-loop) method was used. Cone beam computed tomography (CBCT) was conducted before and after retraction to evaluate alveolar changes and speed.
This was a single-blind study; the statistician was blinded to the data’s origin and grouping. The coinvestigator who performed the measurements was also blinded to group allocation. The principal investigator and patients could not be blinded. The same orthodontist provided the orthodontic treatment.
The sample size of 42 participants was determined using a formula for calculating sample size in clinical trial research comparing average values between two groups (including a control group) and a previous study by Tawfik (2022) [6]. The Ethics Committee in Biological Research (Approval number: 22.063.HV–ĐHYDCT) approved this study. It is registered in the ClinicalTrials.gov with ClinicalTrials.gov ID: NCT06928896. The present article was prepared according to the CONSORT guidelines (Fig. 1).
2.3. Study Procedure
2.3.1. Step 1
The following data were collected: general information, clinical examination, classification of facial symmetry while facing forward, profile, state of the temporomandibular joint, relationships between the first molar teeth, and canine relationship. Patients with bilateral type I angle malocclusion were selected. The PAR(W) index was calculated using the model cast as a measurement. Subsequently, the patients’ model casts, standardized intraoral and extraoral photographs, panoramic films, and cephalometric films were used to make the second selection. A patient’s upper first premolar was removed if orthodontic treatment was indicated. All cephalometric films that met the study’s requirements were analyzed using the customized software WebCeph. Before beginning orthodontic therapy, the bleeding time, clotting time, and platelet count were tested in the patients who met the inclusion criteria. Before participating in the study, patients signed a permission form and received information about the study’s goals and methods.
2.3.2. Step 2
The TransbondTM XT Light Cure Adhesive and the Victory Series Metal Bracket System (MBT 0.022 slot, 3M Unitek®, USA) were employed. This study used a two-step space closure method for tooth extraction, in which the canine is moved backward to obtain a Class I canine relationship, and the relationship between the molars is changed if necessary. Subsequently, CTCB was performed before the procedure of retracting the four incisors. At this stage, the patient’s group allocation was determined randomly. IZC mini-screws (8 x 1.6 mm, 3M UnitekTAD, St. Paul, Minn.) were used in both groups (Figs. 2-4).
In group 1 (sliding mechanism: using elastomeric chains combined with mini-screws), 3M elastomeric chains were used to retract the four maxillary incisors toward the mini-screws with 160 g of force.
In group 2 (loop mechanism), the T-loop was measured and bent using TMA wire (0.016 × 0.022 inches, 3M, USA) to conform to the patient’s arch. The loop was positioned distal to the lateral incisor to initiate the force and modify the loop. Weingart forceps were utilized to retract the archwire posterior to the first premolar, expanding the loop
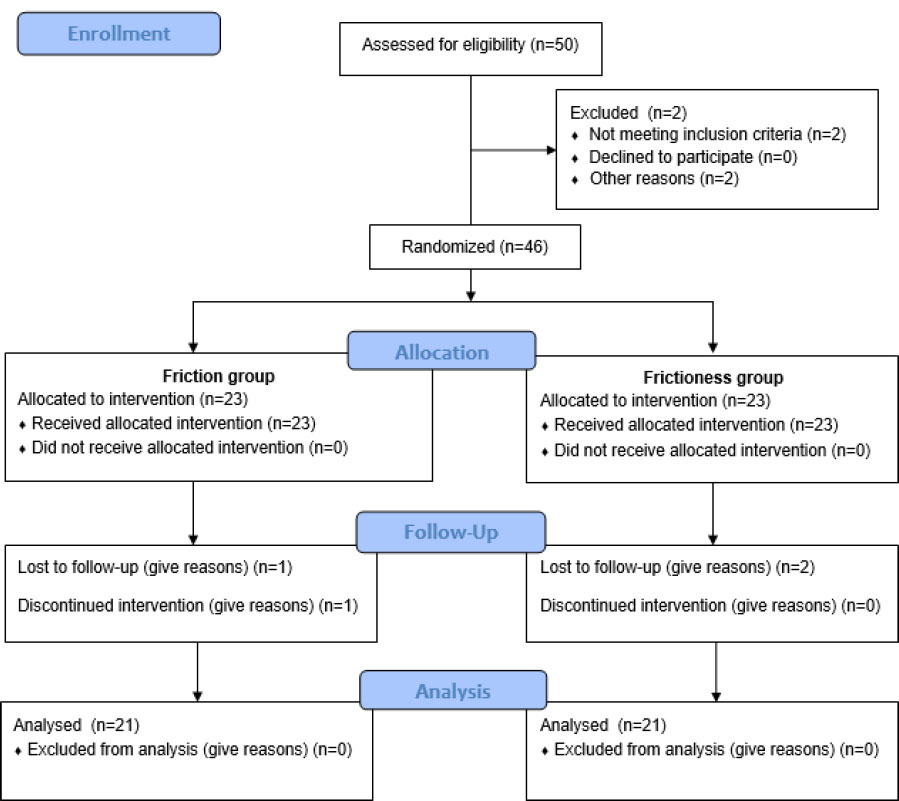
Consort flow chart.
by about 4 mm (150 g) and securing the tail to initiate activation. The loop force was adjusted to fully close space at each subsequent visit. To enhance anchoring, the mini-screw was placed identically on both sides of the arch (the screw positioning resembled that of group 1). Subsequently, the upper first molar was secured to the mini-screws using a 0.012-inch diameter ligature wire.
After the retraction of four incisors, post-retraction CBCT scans were obtained, and the retraction of the four upper incisors was analyzed (overbite achieved 2 mm, Class I canine relationship). CBCT images were generated in DICOM format and imported into Ondemand3Ddental software (Cybermed, Korea, version 1.0.11.1007) for data measurement. The teeth were identified using axial navigation guidance from the multi-planar reconstruction (axial, sagittal, and coronal) of the CBCT, following the measurement method in Le’s study [7], while ensuring that radiation exposure was kept as low as reasonably achievable (ALARA Guidelines) [8].
2.4. Statistical Analysis
SPSS 22.0 software was used to process the study’s indicators and analyze the data. Paired samples t-tests were used to compare two-time points within a single group; independent samples t-tests were used to compare the results of canine movement using elastomeric chains and NiTi closed-coil springs. A 95% level of significance was used to analyze the variables on radiographs.
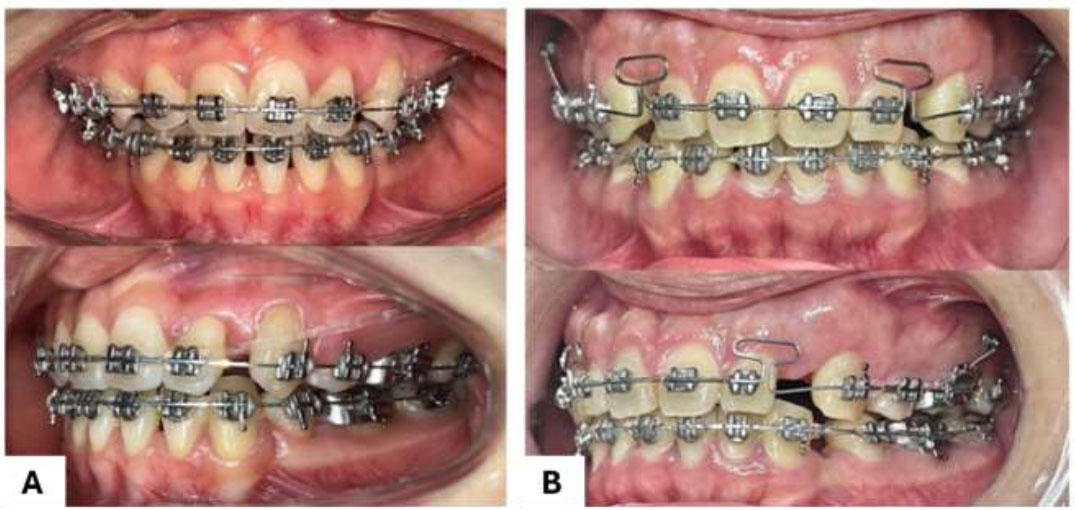
Use of the (A) friction (sliding mechanism with elastomeric chains) and (B) frictionless (T-loop) methods for retracting anterior teeth in Angle Class I malocclusion.
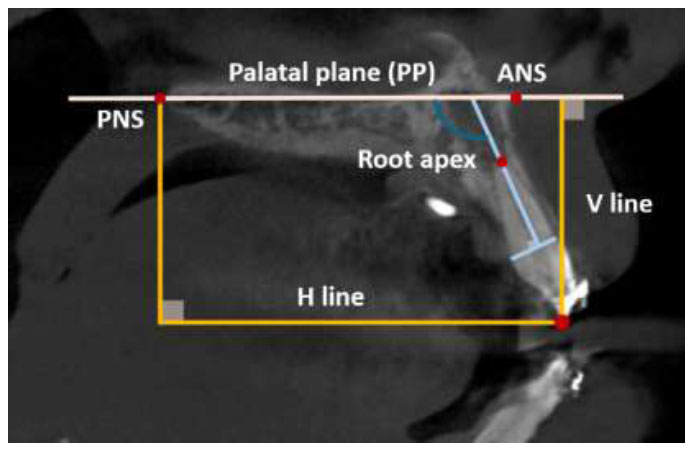
Study variables measured on CBCT. The palatal plane (PP) represents the magnetic connection between the PNS (posterior nasal spine) and the ANS (anterior nasal spine). V: a vertical reference line perpendicular to the ANS-PNS line; H: a vertical reference line parallel to the ANS-PNS line.
| Group | Treatment Time of Retraction | Speed of Retraction | ||
|---|---|---|---|---|
| Mean ± SD | p | Mean ± SD | p | |
| Group 1 | 6.43 ± 1.03 | 0.233* | 0.63 ± 0.09 | 0.001** |
| Group 2 | 6.0 ± 1.22 | 0.85 ± 0.24 | ||
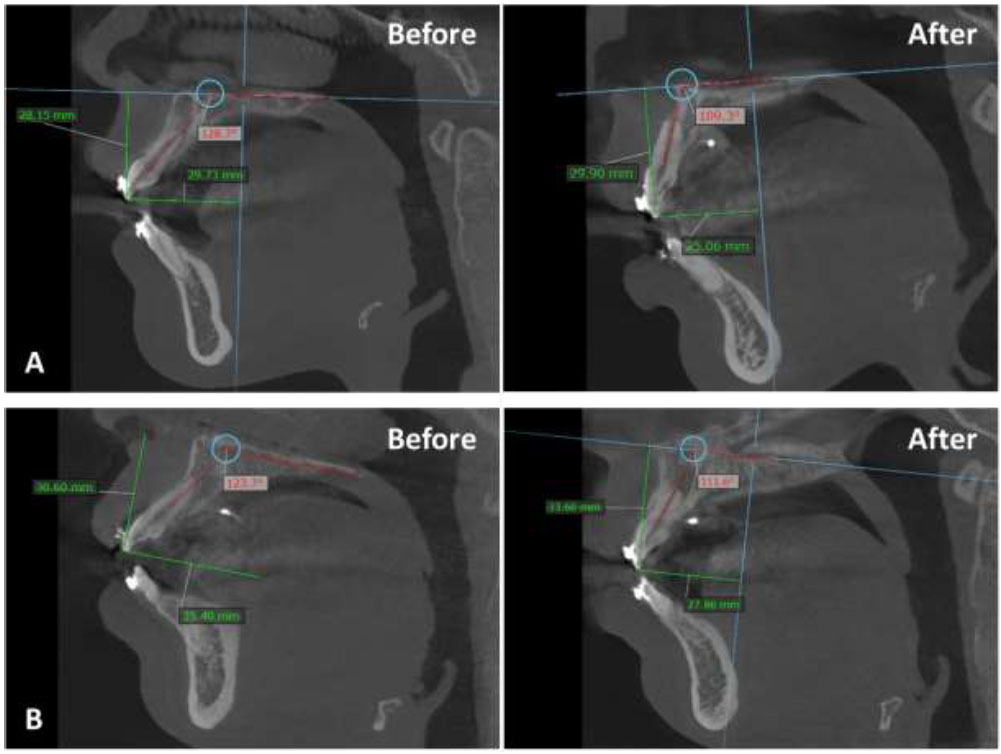
CBCT before and after treatment for both groups: (A) friction group, (B) frictionless group.
3. RESULTS
The speed of the retraction of the four upper incisors was significantly faster in the frictionless (T-loop) group (group 2) than in the friction (sliding mechanism with elastomeric chains) group (group 1) (Table 1).
Following the retraction, the position of the maxillary central incisors was altered, with a significant reduction in the distance between the incisor cusp tip and the V line (U1-V) in both groups. Additionally, the angle between the incisors and the palatal plane (U1-PP) decreased to the standard value in both groups (p < 0.001). The maxillary central incisors tended to protrude after treatment (p < 0.001) in the sliding mechanism group (group 1). The change in the incisors’ vertical position in the loop mechanism group (group 2) was not statistically significant (Table 2). After treatment, the positioning of the maxillary lateral incisors changed, with a notable retraction of the lateral incisors and a substantial reduction in the U2-V distance across all mechanisms. In addition, the angle between the incisors and the palatal plane (U2-PP) significantly decreased in both groups (p < 0.001). No notable alteration occurred in the vertical direction (U2-H) in either group (Table 2).
| Measurements | Group 1 | Group 2 | |||||
|---|---|---|---|---|---|---|---|
| Before | After | p | Before | After | p | ||
| Central Incisor | U1-V (mm) | 29.29 ± 2.70 | 25.17 ± 2.85 | <0.001* | 31.62 ± 2.84 | 26.38 ± 2.37 | <0.001* |
| U1-H (mm) | 28.88 ± 1.90 | 30.08 ± 1.88 | <0.001* | 27.35 ± 3.55 | 27.53 ± 3.52 | 0.417* | |
| U1-PP (°) | 120.67 ± 5.81 | 108.10 ± 3.23 | <0.001* | 121.63 ± 4.19 | 111.99 ± 3.84 | <.,001** | |
| Lateral Incisor | U2-V (mm) | 27.90 ± 1.26 | 24.08 ± 1.30 | <0.001* | 28.56 ± 3.01 | 23.67 ± 2.41 | <0.001* |
| U2-H (mm) | 28.81 ± 1.20 | 29.17 ± 1.52 | <0.219* | 27.22 ± 3.15 | 27.31 ± 3.20 | 0.501* | |
| U2-PP (°) | 118.98 ± 4.95 | 108.34 ± 4.40 | <0.001* | 118.84 ± 5.32 | 109.49 ± 5.00 | <0.001* | |
| Measurements | Group 1 | Group 2 | p | |
|---|---|---|---|---|
| Change | Change | |||
| Central Incisor | U1-V (mm) decreased | 4.12 ± 1.18 | 5.24 ± 2.35 | 0.125* |
| U1-H (mm) increased | 1.20 ± 0.51 | 0.18 ± 1.02 | <0.001** | |
| U1-PP (°) decreased | 12.57 ± 4.69 | 9.65 ± 2.03 | 0.014** | |
| Lateral Incisor | U2-V (mm) decreased | 3.82 ± 0.78 | 4.89 ± 1.92 | 0.134* |
| U2-H (mm) increased | 0.36 ± 1.30 | 0.09 ± 0.61 | 0.057* | |
| U2-PP (°) decreased | 10.64 ± 4.79 | 9.35 ± 5.46 | 0.420** | |
| Tooth Type | Group 1 | Group 2 | p |
|---|---|---|---|
| Change | Change | ||
| Central Incisor | 1.00 ± 0.41 | 0.81 ± 0.47 | 0.173* |
| Lateral Incisor | 0.67 ± 0.32 | 0.61 ± 0.29 | 0.518* |
Regarding post-retraction tooth extrusion, the maxillary central incisors extruded an average of 1.2 mm more in the sliding mechanism group (group 1) than in the loop mechanism group (group 2) (0.18 mm) (p < 0.001). With the sliding mechanism, the angle between the central incisor axis and the palatal plane decreased by 12.57°, which was greater than the 9.65° decrease observed with the loop mechanism (Table 3).
After retraction, the location of the maxillary tooth roots changed. The length of the incisor roots decreased by 1 mm and 0.81 mm in the central incisors and by 0.67 mm and 0.61 mm in the lateral incisors in the sliding mechanism and loop mechanism groups, respectively. Root length alteration did not differ significantly between the two groups (Table 4).
4. DISCUSSION
Due to the three-dimensional nature of cephalometric radiographs, overlapping anatomical structures can hinder the accurate identification of changes in the maxillofacial region [9, 10]. The introduction of CBCT has enhanced the precision of imaging and identification of craniofacial features. Several studies assessing alveolar bone morphology using CBCT images have used the tooth axis as a reference line [11-13]. This approach may lack accuracy in assessing alveolar bone alterations after anterior tooth retraction because the reference sites on the bone also shift with changes in the tooth axis.
This study established a coordinate system based on the palatal bone to evaluate changes in alveolar bone morphology and the position of the posterior teeth involved in the retraction of the four maxillary incisors. The palatal bone remains unchanged during treatment. This reference system is close to the survey area, reducing unwanted changes compared to distant structures and minimizing measurement errors [14, 15]. This study investigated three-dimensional images, unlike studies based on lateral cephalometric films. High-definition CBCT images show the buccal and lingual alveolar bones and teeth without image overlap, which improves measurement accuracy [16-18]. However, CBCT provides detailed three-dimensional pictures of the head, face, and airways. Ethical concerns regarding ionizing radiation exposure must be considered, especially in children. Children's heightened sensitivity to radiation increases their risk of long-term adverse effects, including cancer. The ALARA (as low as reasonably achievable) requires that the potential diagnostic and therapeutic benefits be sufficient to justify the use of ionizing radiation. To ensure compliance with the ALARA principle, several strategies must be implemented. First, the use of CBCT must have a strong clinical justification (i.e., the data obtained from this imaging must be vital for accurate diagnosis and effective treatment planning) [18]. It is essential to optimize radiation dose reduction while maintaining high-quality diagnostic images. Second, the field of view (FOV) must be optimized. This process involves strictly limiting the FOV to the relevant areas, which should only include the skull and facial structures pertinent to the clinical study. Finally, low-dose protocols must be implemented. These techniques optimize exposure parameters by reducing tube current and shortening exposure time while ensuring diagnostic image quality [19].
CBCT has several advantages, such as providing three-dimensional visualization of cranial structures and enhancing physicians’ assessment of airways. However, alternative imaging modalities should be considered whenever possible. Although lateral cephalograms can only produce two-dimensional images, they are a low-radiation option for assessing the bones and soft tissues for the first time [20]. Panoramic radiographs provide a general overview of the dentition but have limited utility in assessing airway dimensions [20, 21]. Magnetic resonance imaging (MRI) is better for observing soft tissues and obtaining three-dimensional information without using ionizing radiation. However, it is expensive, can be difficult to access, and may not be feasible for people with claustrophobia or metal implants [22]. Therefore, the judicious selection of imaging modality should be based on a careful risk-benefit assessment, considering the patient’s age, clinical indication, and the specific information required for diagnosis and treatment planning.
Closing the premolar extraction space with the two-stage technique results in less posterior anchorage loss than closing the space with the one-stage technique [23]. In this study, the anchorage was reinforced with mini-screws for both retraction mechanics. Direct and indirect skeletal anchorage was implemented in the friction and frictionless groups, respectively, during anterior segment retraction. The posterior segments were equally restricted from mesial movement in both groups through direct ligation between the mini-screws and the retracted canines. However, the use of these screws is accompanied by a range of potential complications that can arise at various stages: during placement, throughout the treatment process, and following their removal.
During the placement phase, practitioners may encounter several issues. For instance, a screw may fracture, hindering the planned treatment and complicating subsequent removal or adjustment. Additionally, the adjacent anatomical structures may inadvertently be damaged [24]. For example, damage to the nerve roots can lead to numbness or pain, and damage to the sinuses may cause sinusitis or discomfort. Furthermore, infections can develop at the insertion site, increasing the risk of postoperative complications and potentially necessitating further surgical intervention. Additional concerns arise once the mini-screws are in place and treatment is underway. One of the most common complications is screw loosening, which can jeopardize the entire treatment plan by reducing the effectiveness of anchorage. Soft tissue irritation is another issue, often resulting from friction between the screw and the surrounding tissues, leading to discomfort and possibly contributing to localized inflammation. An additional concern is bone resorption around the screw; the bone may begin to break down, potentially compromising the stability of the mini-screw and affecting overall treatment outcomes. Post-treatment complications may also arise, including lingering pain and discomfort as the body adapts to the absence of the screws. This can be attributed to the body’s healing response and the residual effects of irritation or injury that occurred during treatment [25].
4.1. The Treatment Time and the Speed of the Retraction
Various factors affect the duration of retraction, not just the rate of tooth movement. Other critical elements include space-closing mechanics and the level of patient cooperation. Anne’s study focused on the biochemical analysis of specific chemical mediators in gingival sac fluid, demonstrating that the concentration of these mediators is greater in younger individuals than in adults. This suggests that the initial rate of tooth movement is typically faster in younger patients [26]. Conversely, adults are more likely to require early appliance removal and show greater compliance with treatment protocols.
In the current study, the friction group demonstrated an average retraction period of 6.43 months, and the frictionless group showed a comparable duration of 6 months. These durations exceed those reported by Eksriwong et al., who reported an average retraction time of 4.2 months. This difference may be attributed to the shorter retraction distance used in Eksriwong’s study [27].
In addition, the frictionless group exhibited a retraction speed of 0.85 mm per month, notably higher than the retraction speed of 0.63 mm per month in the friction group. This difference may stem from the characteristics of the impact forces involved. With the friction method, the force generated by the loop is continuous; with the sliding mechanism utilizing chain elastics, the impact force is intermittent. This intermittent force application can lead to a gradual reduction in effectiveness over time and may slow the tooth retraction process.
Elastomeric chains experience significant force loss; within the first 24 hours, these materials can lose approximately 50% to 70% of their initial force, with only 30% to 40% of the original force remaining after 3 weeks [28].
Elastomeric chains are widely used in orthodontics because they are simple, easy to use, and low maintenance for patients. Because they are made from synthetic rubber, these chains are susceptible to deformation over time. The absorption of saliva can adversely affect the molecular structure of the elastics. Continuous elastics tend to deliver higher initial force and sustain that force for a longer duration than intermittent elastics. However, a significant limitation of these systems is the rapid biodegradation associated with force loss [28, 29].
4.2. Vertical Tooth Movement and Change in Angle between Tooth Axis and Palatal Plane
Both groups exhibited tooth extrusion following treatment. This extrusion may be attributed to alterations in the position of the incisal edge after the leveling and flattening stage of the dental arch, as well as the potential for tooth extrusion during the retraction process. The retraction force is applied below the center of resistance of the four maxillary incisors, resulting in a clockwise rotation around the center of resistance. This rotational movement can induce the protrusion of the incisors during retraction. These results align with the findings of Ruenpol et al. (2019), who also reported tooth extrusion when employing a sliding mechanism for the retraction of the incisors. The rotation of the incisors around the center of resistance leads to the outward movement of the teeth [30].
In addition, both groups exhibited a reduction in the angle between the incisor axis and the palatal plane (PP) after treatment (the U1-PP). This angle reduction was similar to that reported in Yodthong’s study (10.90) after the retraction of four incisors, which significantly improved the patient’s profile [13]. The incisors were repositioned to the standard value to stabilize the tooth axis after treatment.
In our study, most participants in the treatment group had a favorable aesthetic outcome, eliminating the need for further correction. Thus, the active bending technique developed in this study lowered the four incisors by 1 mm, thereby effectively preventing extrusion. The findings indicate that the level of incisor extrusion was significantly reduced in the loop mechanism group compared with the sliding mechanism group. The configuration of the friction method, which applied a retraction force positioned below the center of resistance (CR), resulted in a clockwise rotation of the anterior teeth. This rotation caused the incisal edges to tilt linguinally while protruding slightly. Conversely, in the frictionless method, the design for the anterior teeth featured a T-loop in which the vertical component was 1 mm shorter than that of the posterior teeth. This design adjustment effectively minimized tooth protrusion. A significant benefit of wire bending in the frictionless method lies in its ability to facilitate adjustments to treatment outcomes. This ensures alignment with the established treatment plan. The friction method enables the modification of the retraction force’s location, either across the CR for bodily movement or above the CR for minimal protrusion force, depending on the requirements of the specific clinical application [23].
4.3. Anteroposterior Tooth Movement
This study presents the results of tooth retraction after treatment in both treatment groups regarding the improvement in the patient’s profile. Frictionless methods often provide superior control over the torque of the incisors during retraction; however, no statistically significant difference was found between the two groups (p > 0.05). Eksriwong et al. studied the retraction of four incisors using the loop mechanism using the same H-V reference system and recorded a retraction range of 2.1 mm to 5.6 mm from the tip of the incisor’s incisal edge to the V line [27].
4.4. Reduction in Root Length after Treatment
We observed that root length decreased following retraction using both treatment methods. The root resorption associated with the frictionless technique utilizing a TMA T-loop spring was comparable to that associated with the friction technique. This similarity may be attributed to the application of a continuous and gentle force, approximately 150 grams, which is within the recommended parameters. Similarly, a study by Bakhit et al. on 30 Egyptian female patients treated using the sliding mechanism or loop mechanism showed that the root length decreased using both treatment methods, but root resorption was not clinically significant [29].
5. LIMITATIONS
Further research is warranted to investigate the characteristics of individuals with Angle Class II and III malocclusion, along with a comparative analysis of all three classes. Such studies would provide a more comprehensive understanding of treatment strategies that can be implemented in clinical practice. This study was conducted immediately following the retraction of the four maxillary incisors, and thus, the alveolar bone remodeling was not completed. Therefore, extended monitoring of the treatment outcomes is necessary for a more accurate assessment of both the effectiveness of the treatment and the likelihood of recurrence, particularly with the use of sliding and loop mechanisms. Moreover, our study did not address potential anchorage loss despite employing temporary anchorage devices (TADs) to enhance stability. It is possible that this omission occurred because of the direct loading applied to the first permanent molars through the engagement of the beta arm of the T-loop. Conversely, in the friction group, the direct loading was appropriately directed to the mini-screws.
CONCLUSION
Overlapping anatomical structures have little effect on the three-dimensional visuals generated by CBCT, and the palatal bone remains unchanged during treatment. Therefore, CBCT can effectively assess the position of the posterior teeth that retract the four maxillary incisors. After treatment, frictionless (T-loop) methods often provide superior control over the torque and extrusion of the incisors during retraction and are faster; however, our results showed that root resorption was similar between the friction (sliding mechanism with elastomeric chains) and frictionless group.
AUTHORS’ CONTRIBUTIONS
L.N.L.: Study concept or design; K.P.V.L.: Conceptualization; T.T.D.: Methodology; T.T.L.: Study Concept or design.
LIST OF ABBREVIATIONS
| CBCT | = Cone beam computed tomography |
| TAD | = Temporary anchorage device |
| CR | = Center of resistance |
| MRI | = Magnetic Resonance Imaging |
| FOV | = Field of View |
| PNS | = Posterior Nasal Spine |
| PP | = Palatal Plane |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This research was approved by the ethics committee of the Can Tho University of Medicine and Pharmacy, Vitenam (approval number: 22.063.HV–ĐHYDCT).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article will be available from the corresponding author [L.N.L] upon reasonable request.
ACKNOWLEDGEMENTS
The authors are grateful for the facilities and support provided by the Faculty of Odonto and Stomatology, Can Tho University of Medicine and Pharmacy, Vitenam.


