All published articles of this journal are available on ScienceDirect.
The Impact of Surface Treatments and 3D Printing Machines on the Biaxial Flexural Strength of 3D-Printed Composite Resins
Abstract
Introduction
The use of 3D-printed composite resins, such as BEGO TriniQ, is increasing in restorative dentistry due to their aesthetic and functional potential. However, the biaxial flexural strength of these materials—and the influence of surface treatments and printing machines—requires further investigation to determine their suitability for high-stress clinical applications.
Materials and Methods
Eighty BEGO TriniQ composite resin specimens were 3D-printed, with 40 produced using the Asiga MAX UV and 40 using the SprintRay Pro printer. Specimens (14 mm diameter, 2 mm thickness) were divided into four treatment groups: control (no treatment), sandblasting, hydrofluoric acid etching, and a combination of both. Biaxial flexural strength was tested using a universal testing machine, and results were analyzed using two-way ANOVA.
Results
Flexural strength ranged from 103.29 MPa to 113.60 MPa. Although Asiga MAX UV printed specimens showed slightly higher values than SprintRay Pro, the differences were not statistically significant (p > 0.05). Surface treatments also did not significantly affect flexural strength, and no interaction was observed between surface treatment and printer type.
Discussion
The findings indicate that neither surface treatments nor the type of 3D printing machine significantly influenced the biaxial flexural strength of BEGO TriniQ resin. This aligns with prior research suggesting that surface treatments may enhance surface characteristics but do not substantially improve mechanical performance in 3D-printed composites. The results emphasize the need for alternative reinforcement strategies to enhance mechanical properties for clinical applications in high-stress areas.
Conclusion
Surface treatments and 3D printing machines did not significantly impact the biaxial flexural strength of BEGO TriniQ. The material appears suitable for low-stress applications, but further material enhancements are needed to optimize its performance in demanding clinical conditions.
1. INTRODUCTION
The evolution of 3D-printed composite resins has brought significant advancements in fixed dental restorations, offering highly customizable and efficient solutions for both temporary and permanent applications [1]. For temporary restorations, 3D printing enables the rapid production of crowns, bridges, and veneers, providing patients with functional and aesthetically pleasing restorations while awaiting their permanent solutions [2, 3]. This digital workflow not only enhances accuracy but also reduces chairside time, leading to improved patient outcomes and higher satisfaction [4].
Recent advancements in resin materials have expanded the use of 3D-printed composites to permanent restorations. These high-performance materials exhibit enhanced wear resistance, fracture toughness, and biocompatibility, making them suitable for long-term use [2, 3, 5]. Nevertheless, even with recent advancements, 3D-printed composite resins typically exhibit inferior mechanical strength compared to conventional dental materials [4], along with other challenges, such as long-term durability, wear resistance, and marginal adaptation due to resin shrinkage, particularly in high-stress areas. Addressing these issues is crucial for their broader use in permanent, load-bearing restorations [6, 3].
Nonetheless, the aesthetic versatility, cost-effectiveness, and precision of 3D printing make 3D-printed composite resins viable options for selected permanent restorations, particularly when combined with techniques designed to enhance their mechanical strength [7]. Since 3D-printed composite resins generally possess lower mechanical strength compared to traditional dental materials like zirconia and lithium disilicate, their use is limited in high-stress areas of the mouth [6]. For instance, 3D-printed resins typically have flexural strengths between 76 and 143 MPa, which often confines their use to temporary or non-load-bearing permanent restorations [8, 9].
In contrast, zirconia offers much higher biaxial flexural strength, ranging from 900 to 1200 MPa, making it the material of choice for high-load-bearing restorations, such as molar crowns and bridges, due to its exceptional durability and fracture resistance [10, 11]. Lithium disilicate ceramics (e.g., E-max) provide a balance between aesthetics and strength, with flexural strengths between 350 and 450 MPa, making them particularly suitable for anterior restorations [12]. Other ceramics, like alumina (450-600 MPa) and feldspathic ceramics (60-120 MPa), vary in strength and translucency, and their clinical applications are largely determined by the need for either aesthetics or mechanical durability [13, 14].
To address the inherent limitations of 3D-printed composite resins, researchers are actively exploring methods to enhance their mechanical properties. Surface treatments, such as sandblasting and acid etching, are widely employed to improve the flexural strength of dental materials [15]. Sandblasting creates surface roughness and induces compressive stresses that help prevent crack propagation, while acid etching chemically alters the surface by removing weak layers, resulting in a more uniform and robust structure [15]. These treatments may hold promise for enhancing the mechanical performance of 3D-printed resins, potentially making them more suitable for permanent, load-bearing restorations [16]. The clinical adoption of 3D-printed composite resins can significantly improve patient outcomes. Faster production times reduce the number of necessary clinic visits, and the precision of digital workflows ensures better-fitting restorations with fewer adjustments. Combined with the aesthetic flexibility of 3D-printed materials, these factors can enhance patient satisfaction and long-term success [4].
Digital Light Processing (DLP) and Stereolithography (SLA) are advanced 3D printing technologies that transform liquid resin into precise objects through photopolymerization. DLP cures entire layers simultaneously using a digital projector, offering faster production suited for intricate and large-scale designs. In contrast, SLA employs a laser to solidify individual points on each layer, delivering superior precision and smooth surfaces. Unlike traditional subtractive methods like milling, which removes material, these additive techniques build objects layer by layer, reducing waste. Their ability to create complex geometries and facilitate rapid prototyping makes them essential in dentistry for producing customized prosthetics, restorations, and innovative biomaterials [17-19].
The choice of a 3D printing machine also plays a crucial role in determining the mechanical properties of printed materials. Differences in light intensity settings, layer thickness control, and curing processes across different printers can significantly influence the final strength of the printed materials. In this study, two popular 3D printers, Asiga and SprintRay, are evaluated for their impact on the biaxial flexural strength of BEGO TriniQ resin. Asiga’s DLP technology allows for precise control over the printing parameters, which could result in smoother surfaces and stronger material properties. In contrast, SprintRay, while also based on DLP technology, differs in printing speed and light exposure settings, potentially influencing the curing process and layer bonding. By investigating the combined effects of different surface treatments and 3D printing machines on the biaxial flexural strength of 3D-printed resins, this study aims to provide insights into optimizing these materials for broader clinical applications.
2. MATERIALS AND METHODS
This study aimed to evaluate the effects of different surface treatments and 3D printing machines on the biaxial flexural strength of 3D-printed composite resins. A total of 80 composite resin specimens were fabricated using two different 3D printing machines, and the specimens were divided into 8 groups of 10 each based on the surface treatments applied. The biaxial flexural strength was measured to assess the mechanical performance of each group.
The composite resin material used in this study was BEGO TriniQ resin (Lot 601398, BEGO, Bremen, Germany), which is compatible with both 3D printers employed in the study (Fig. 1). The two 3D printers used were the Asiga MAX UV (Asiga, Alexandria, Australia) and the SprintRay Pro (SprintRay, Los Angeles, USA), both utilizing digital light processing (DLP) technology. Table 1 provides detailed specifications for the Asiga MAX UV and SprintRay Pro printers, highlighting key parameters that may influence the biaxial flexural strength of the fabricated specimens [20, 21].

BEGO triniQ resin used in the study.
| Specification | Asiga MAX UV | SprintRay Pro |
| Printing Resolution | 50 µm | 55 µm |
| Layer Thickness | 50 µm | 55 µm |
| Curing Wavelength | 385 nm | 405 nm |
| Printing Orientation | Horizontal | Horizontal |
| Software Used | Asiga Composer | Ray Ware |
| Build Volume | 119 X 67 X 75 mm | 190 X 120 X 210 mm |
| Printing Speed | Adjustable, up to 80 mm/hour | Adjustable, up to 100 mm/hour |
| Light Source | UV LED | LED-based |
Specimens were designed with a circular diameter of 14 mm and a thickness of 2 mm. The ASIGA composer software was used for designing the specimen files for the Asiga MAX UV printer, while the SprintRay Pro software was used for the SprintRay Pro printer. All designs were standardized across groups to ensure uniformity. The 3D printing process was performed using BEGO TriniQ resin, which was loaded into each printer’s resin tank. Printing parameters were set according to the manufacturer's recommendations, with a layer thickness optimized for high precision and detail. After printing, the specimens were carefully removed from the build platform using a metal scraper, and excess uncured resin was cleaned by submerging the specimens in 99% isopropyl alcohol for approximately 5 minutes, with gentle agitation to ensure thorough cleaning. Once cleaned, the specimens were post-cured in a nitrogen atmosphere using a curing chamber (Gas N2 4500) to optimize polymerization and improve mechanical properties. The curing process lasted for a specific duration, with the specimens rotated to ensure even UV light exposure. This procedure was applied consistently to both the Asiga MAX UV and SprintRay Pro printed specimens (Figs. 2 and 3).
The surface treatments involved sandblasting and hydrofluoric acid etching. Sandblasting was conducted using 50 µm aluminum oxide particles (Renfert, Germany) at a controlled pressure of 2.5 bar and a distance of 10 mm. Hydrofluoric acid etching was performed using 9.6% hydrofluoric acid etch gel (Pulpdent Porcelain Etch Gel, Lot 161115, Pulpdent, Watertown, MA, USA). The discs in the acid etching group were treated for 60 seconds, followed by thorough rinsing with water and air drying.
The specimens were then assigned to 8 groups of 10 specimens each: Group 1 (Asiga MAX UV, control): No surface treatment, Group 2 (Asiga MAX UV): Sandblasting with 50 µm aluminum oxide particles at 2.5 bar pressure and 10 mm distance, Group 3 (Asiga MAX UV): Hydrofluoric acid etching for 60 seconds, followed by rinsing and drying, Group 4 (Asiga MAX UV): Combination of sandblasting and hydrofluoric acid etching, Group 5 (SprintRay Pro, control): No surface treatment, Group 6 (SprintRay Pro): Sandblasting under the same conditions as Group 2, Group 7 (SprintRay Pro): Hydrofluoric acid etching for 60 seconds, followed by rinsing and drying, and Group 8 (SprintRay Pro): Combination of sandblasting and hydrofluoric acid etching.
Biaxial flexural strength testing was conducted using an Instron universal testing machine (model 5566A) equipped with a 1-kN load cell. The testing procedure followed ISO 6872:2015 standards, employing a ball-on-three-ball configuration. Three equally spaced ball bearings (120 degrees apart) supported the specimens to ensure uniform stress distribution and minimize localized stress concentrations. The load was applied at the center using a piston until specimen failure occurred.
Biaxial flexural strength testing was conducted using an Instron universal testing machine (model 5566A) equipped with a 1-kN load cell. The testing procedure adhered to ASTM Standard C1499-20, commonly utilized to evaluate biaxial flexural strength in advanced ceramics. A controlled and steady load was applied at a crosshead speed of 0.5 mm/min. Specimens were centrally supported on a circular fixture with three equally spaced ball bearings to ensure uniform stress distribution and minimize localized stress concentrations. The load was applied at the center of the specimens using a piston until failure occurred. The biaxial flexural strength (σ) was calculated using the following formula: Biaxial flexural strength =-0.2387 P (X-Y)/d2, where P is the load at fracture (N), d is the specimen thickness (mm), and X and Y are constants based on the geometry of the specimen: X = (1 + v) ln(r2/r3) [2] + (1 - v)/22 and Y = (1 + v)[1 + ln(r1/r3) [2] + (1 - v)(r1/r3) [2] (Fig. 4).
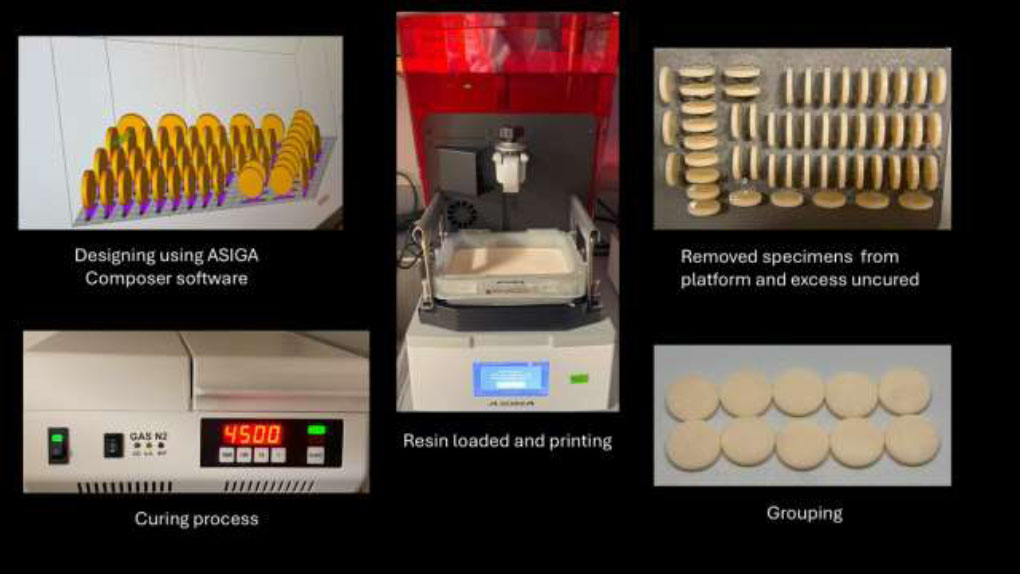
Steps in specimen fabrication using asiga printer.
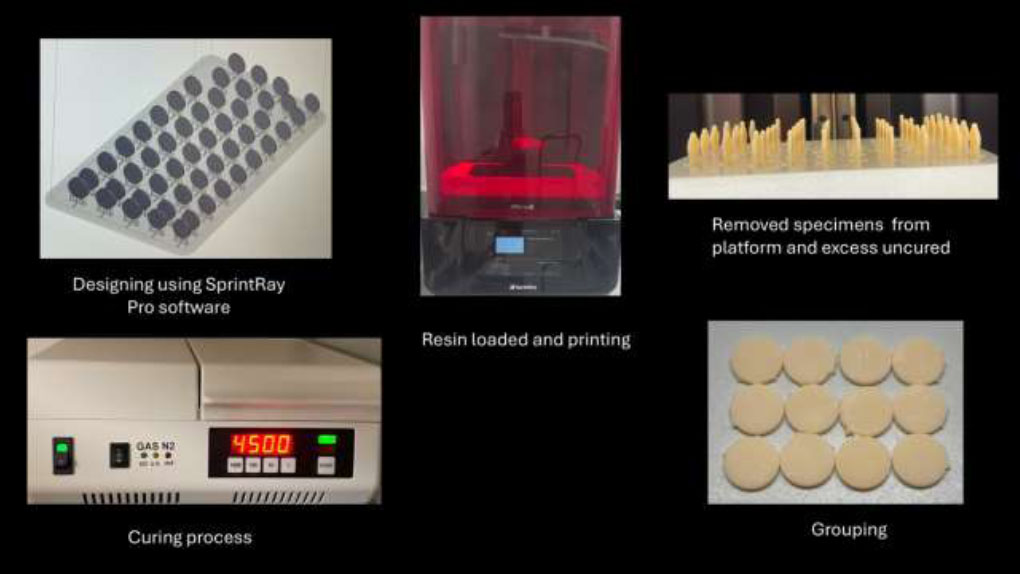
Steps in specimen fabrication using sprintray printer.
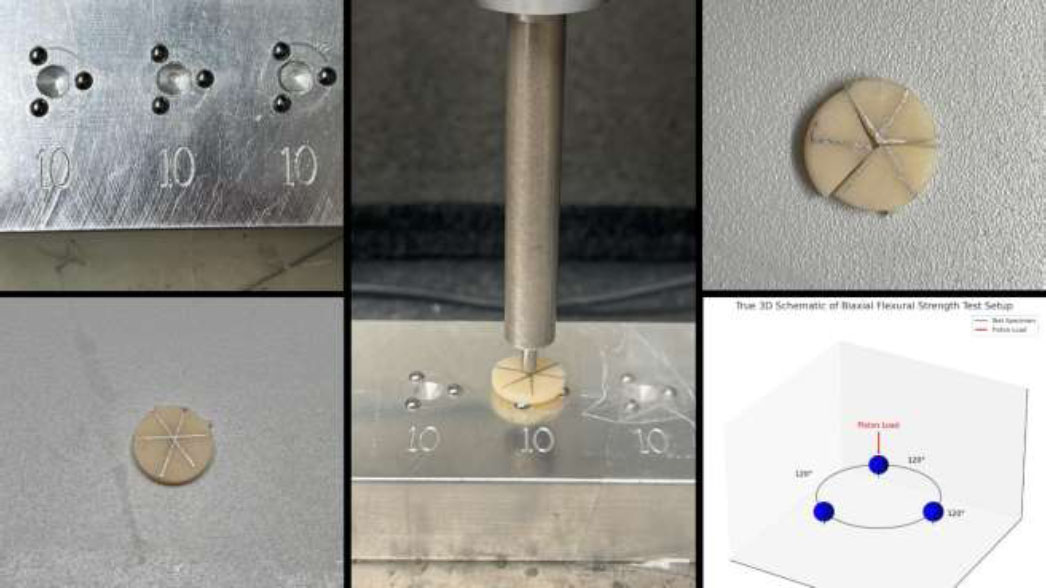
Specimen stages before, during, and after biaxial flexural strength testing using the instron universal testing machine.
The biaxial flexural strength test was conducted because it effectively replicates the multi-directional forces that dental materials experience in the oral cavity, offering a realistic evaluation of mechanical performance. Compared to uniaxial testing, this method reduces the influence of stress concentrations at the edges and provides a more uniform stress distribution across the specimen. It also allows for the use of small, standardized samples, making it well-suited for testing 3D-printed materials. This approach ensures accurate and practical insights into the material’s strength and reliability, supporting its optimization for dental applications involving high-stress conditions [22, 23].
The statistical analysis was performed using SPSS software (trial version, IBM, USA). A 2-way ANOVA followed by Tukey's post hoc test was carried out to compare the biaxial flexural strength between the groups. A significance level of p < 0.05 was considered statistically significant.
3. RESULTS
This study evaluated the impact of different surface treatments and 3D printing machines on the biaxial flexural strength of BEGO TriniQ composite resin. A total of 80 specimens were tested, with each group containing 10 specimens divided between two 3D printing machines: Asiga MAX UV and SprintRay Pro. The surface treatments applied included no surface treatment, sandblasting, hydrofluoric acid etching, and a combination of sandblasting and hydrofluoric acid etching.
The biaxial flexural strength of the specimens ranged from 103.29 MPa to 113.60 MPa, depending on the combination of the 3D printing machine and surface treatment. For the Asiga MAX UV printer, biaxial flexural strength was 112.00 ± 15.36 MPa for no surface treatment, 113.60 ± 14.32 MPa for sandblasting, 109.58 ± 23.41 MPa for hydrofluoric acid etching, and 103.98 ± 9.36 MPa for the combination of sandblasting and hydrofluoric acid etching. For the SprintRay Pro printer, it was 103.29 ± 16.13 MPa for no surface treatment, 104.03 ± 20.97 MPa for sandblasting, 110.41 ± 17.54 MPa for hydrofluoric acid etching, and 112.00 ± 15.36 MPa for the combination of sandblasting and hydrofluoric acid etching.
Analysis of the force-displacement curves (bending deformation curves) revealed the material's behavior under loading conditions. Initially, all specimens exhibited elastic deformation, represented by a linear increase in force. This was followed by localized plastic deformation and brittle failure, as indicated by a sudden drop in force after the peak. The fully supported bottom surface concentrated stress at the loading point, leading to variability in maximum load capacity (188–395 N) and displacement at failure (0.6–0.9 mm), reflecting differences in material strength and ductility (Fig. 5).
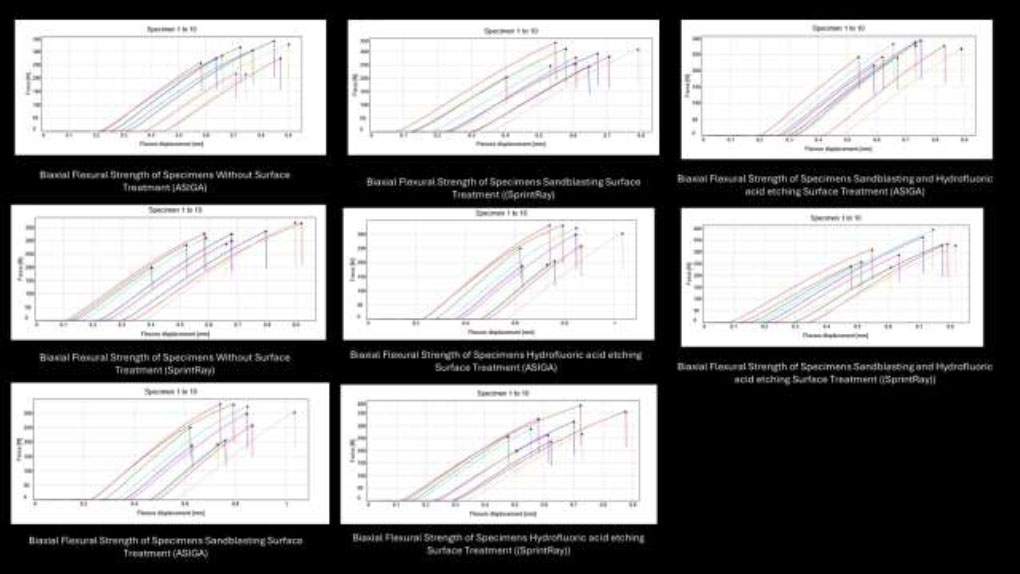
Force-displacement curves illustrating biaxial flexural behavior of specimens under different surface treatments.
The bar graph (Fig. 6) compares the biaxial flexural strength across surface treatments for both 3D printers. It depicted that the Asiga MAX UV consistently produced slightly higher flexural strength values than the SprintRay Pro, with the highest strength observed in the sandblasting group (113.60 MPa). Conversely, SprintRay Pro achieved its highest strength with the combination of sandblasting and hydrofluoric acid etching (112.00 MPa), illustrating the subtle differences in performance between the two printers under different treatment conditions.
A two-way ANOVA was carried out to assess the impact of 3D printing machines and surface treatments on biaxial flexural strength. The results indicated that the type of 3D printing machine did not have a statistically significant effect on biaxial flexural strength, with an F-value of 0.384 and a p-value of 0.538 (F(1, 72) = 0.384, p = 0.538). This suggests that there were no meaningful differences in flexural strength between specimens printed using the Asiga MAX UV and SprintRay Pro machines. Similarly, surface treatments did not significantly affect biaxial flexural strength (F(3, 72) = 0.075, p = 0.973). The differences observed across the four surface treatments (no surface treatment, sandblasting, hydrofluoric acid etching, and their combination) were minimal and not statistically significant, as reflected by the low F-value and high p-value. Furthermore, no significant interaction was found between the type of 3D printing machine and surface treatment (F(3, 72) = 1.208, p = 0.313). This indicates that the effect of surface treatments on biaxial flexural strength was not influenced by the choice of 3D printer and vice versa. The interaction plot illustrates the relationship between surface treatments and biaxial flexural strength across both 3D printing machines. The parallel lines in the plot indicate no significant interaction between the type of 3D printer and surface treatments, confirming that these two factors acted independently in this study (Fig. 7).
Post-hoc Tukey’s tests were conducted to compare the different surface treatment groups, and the results indicated no statistically significant differences in biaxial flexural strength between any of the surface treatments. The mean differences between the groups ranged from -2.00 MPa to 2.34 MPa, with all significance (Sig.) values above 0.05, confirming the lack of statistical significance. The pairwise comparisons showed that the mean difference between hydrofluoric acid etching and no surface treatment was 2.35 MPa, with a 95% confidence interval ranging from -11.82 MPa to 16.51 MPa (Sig. = 0.972). The mean difference between hydrofluoric acid etching and sandblasting was 1.18 MPa, with a confidence interval ranging from -12.98 MPa to 15.34 MPa (Sig. = 0.996). Additionally, the mean difference between hydrofluoric acid etching and the combination of sandblasting plus hydrofluoric acid etching was 2.00 MPa, with a confidence interval ranging from -12.16 MPa to 16.16 MPa (Sig. = 0.982) (Fig. 7).
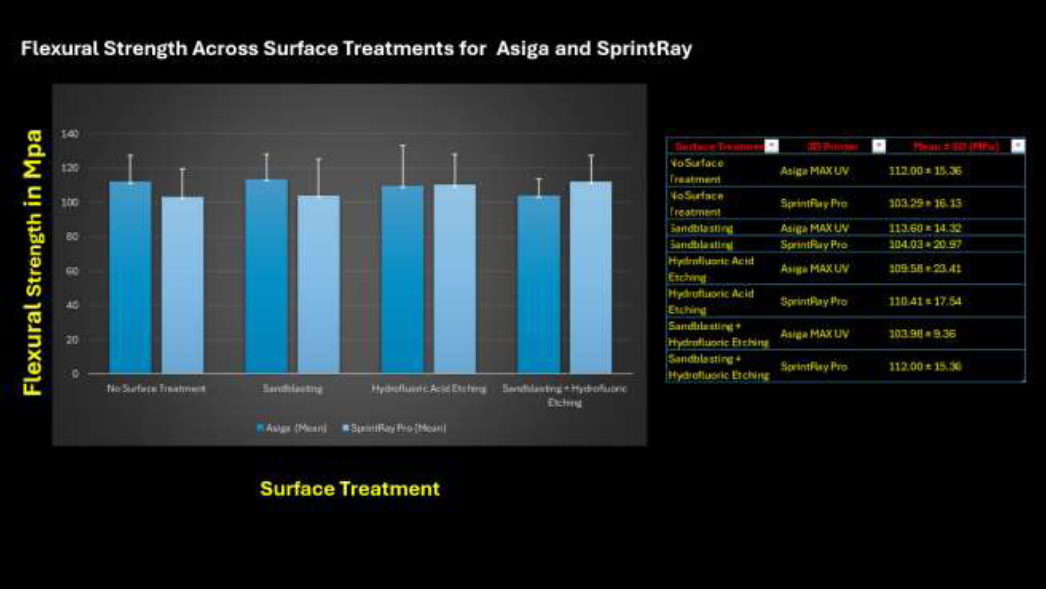
Bar graph comparing the biaxial flexural strength of bego TriniQ composite resin across surface treatments for both 3D printers (asiga MAX UV and sprintray pro).
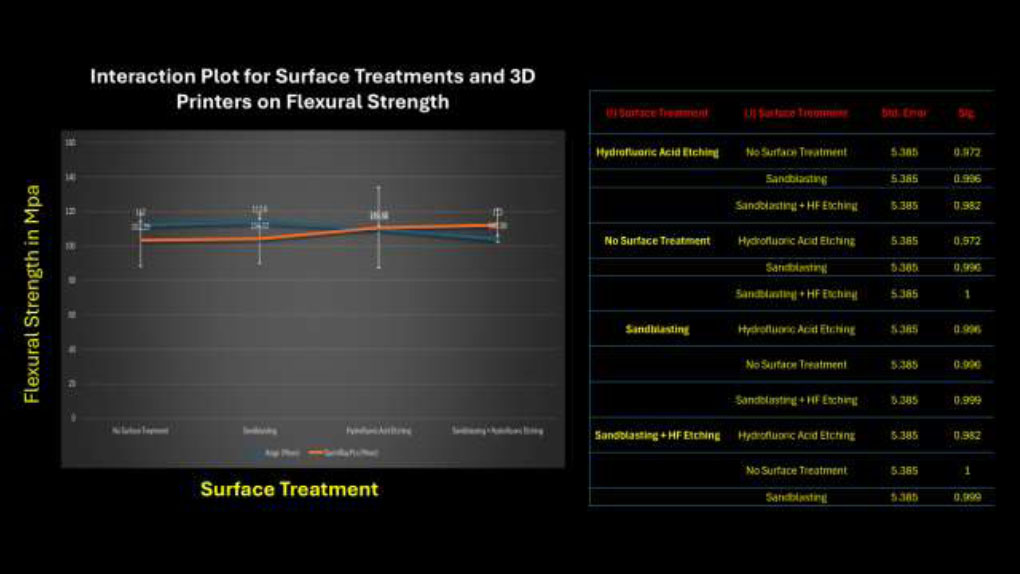
Interaction plot of surface treatments and 3D printing machines on biaxial flexural strength.
Pairwise comparisons of surface treatments using post-hoc tukey’s test for biaxial flexural strength of BEGO triniQ composite resin.
Comparisons between sandblasting and no surface treatment revealed a mean difference of -1.17 MPa, with a confidence interval from -15.33 MPa to 12.99 MPa (Sig. = 0.972). The mean difference between sandblasting plus hydrofluoric acid etching and no surface treatment was 0.35 MPa, with a confidence interval ranging from -13.82 MPa to 14.51 MPa (Sig. = 0.996). Furthermore, the mean difference between sandblasting and sandblasting plus hydrofluoric acid etching was 0.82 MPa, with a confidence interval ranging from -13.34 MPa to 14.99 MPa (Sig. = 1.000). Lastly, the mean difference between sandblasting plus hydrofluoric acid etching and hydrofluoric acid etching was -2.00 MPa, with a confidence interval ranging from -16.16 MPa to 12.16 MPa (Sig. = 0.996), and the mean difference between sandblasting and hydrofluoric acid etching was -1.17 MPa, with a confidence interval ranging from -12.99 MPa to 15.33 MPa (Sig. = 0.996). The overlap of all confidence intervals, along with the non-significant Sig. values (all above 0.05), confirmed that none of the pairwise comparisons were statistically significant (Fig. 7).
The interaction plot represents these pairwise comparisons, highlighting that the overlapping confidence intervals and small mean differences between surface treatment groups emphasize the lack of significant variation in biaxial flexural strength. The plot further confirms that surface treatments did not significantly impact biaxial flexural strength in this study (Fig. 8).
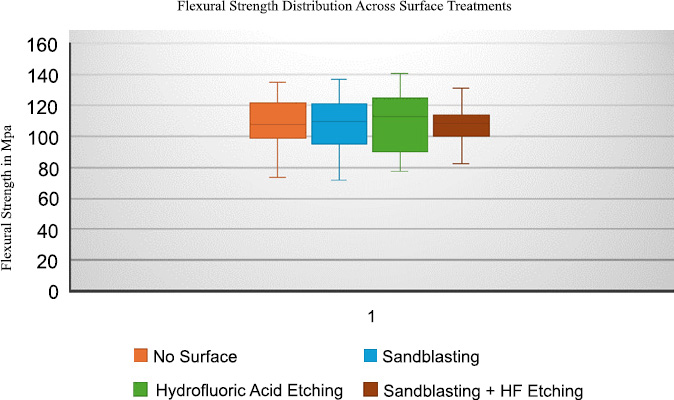
The homogeneous subset analysis revealed that all surface treatments could be grouped into a single subset, further confirming that none of the treatments resulted in significantly different biaxial flexural strengths. The mean biaxial flexural strengths across the groups showed minimal variation, ranging from 107.65 MPa to 109.99 MPa, indicating a narrow distribution.
In conclusion, neither the type of 3D printing machine (Asiga MAX UV or SprintRay Pro) nor the surface treatment (no surface treatment, sandblasting, hydrofluoric acid etching, or a combination of sandblasting and hydrofluoric acid etching) had a significant effect on the biaxial flexural strength of BEGO TriniQ composite resin. These findings suggest that under the conditions tested, neither the 3D printing machine nor the surface treatment is a critical factor in enhancing the biaxial flexural strength of this material.
4. DISCUSSION
The goal of this study was to investigate the effects of surface treatments and 3D printing machines on the biaxial flexural strength of BEGO TriniQ composite resins. By evaluating four surface treatments (no surface treatment, sandblasting, hydrofluoric acid etching, and a combination of sandblasting and hydrofluoric acid etching) and two 3D printers (Asiga MAX UV and SprintRay Pro), this study aimed to determine whether these factors significantly influence the mechanical properties of 3D-printed composite resins.
The surface treatments investigated in this study, namely sandblasting, hydrofluoric acid etching, and their combination, are widely used in dentistry to modify surface characteristics and enhance the mechanical performance of restorative materials. Sandblasting introduces surface roughness and compressive stresses, which can resist crack propagation and improve strength. Similarly, hydrofluoric acid etching chemically alters the surface, creating irregularities that may contribute to enhanced mechanical properties. When used together, these treatments are often expected to synergistically improve biaxial flexural strength. While such methods have shown significant effects on materials like zirconia by enhancing durability through surface modifications, their impact on the mechanical properties of 3D-printed composite resins, such as BEGO TriniQ, remains largely unexplored [16, 24].
The findings of this study indicate that surface treatments, including sandblasting and hydrofluoric acid etching, did not significantly enhance the biaxial flexural strength of BEGO TriniQ resin. This outcome aligns with previous studies, which demonstrated that while surface treatments improved surface roughness and flexural strength in repaired 3D-printed denture bases, the treated materials did not achieve the strength levels of intact groups. This suggests that although surface treatments can modify surface properties and improve adhesion, their effect on mechanical properties, such as flexural strength, remains limited. It has been observed that the intrinsic mechanical limitations of 3D-printed materials, particularly in terms of flexural strength, were not substantially overcome by surface treatments alone [25, 8].
The lack of significant improvement in biaxial flexural strength with surface treatments, as observed in this study, might be attributed to the intrinsic properties of BEGO TriniQ resin. This material’s polymer matrix, with a lower filler content compared to milled composites, contributes to its mechanical limitations. The absence of significant statistical differences aligns with prior studies indicating that 3D-printed materials generally exhibit lower strength compared to milled counterparts. Additionally, the differences in light polymerization during the printing process may result in incomplete cross-linking, which reduces the ability of surface treatments to enhance mechanical strength [8, 26-28].
Since no direct studies exist on the biaxial flexural strength of 3D-printed resins for fixed restorations, our results can be compared with findings from studies on 3D-printed denture bases. Asli et al. (2021) examined the effects of different surface treatments on repaired 3D-printed denture bases and found that, while surface treatments significantly improved surface roughness and flexural strength, the treated materials did not achieve the strength of intact specimens. Bur grinding yielded the highest flexural strength among the treatments. However, similar to our study, their results highlight the limited ability of surface treatments to enhance the mechanical strength of 3D-printed materials for high-stress applications. This comparison emphasizes the need for further research into alternative methods, beyond surface treatments, to improve the mechanical properties of 3D-printed resins for both fixed restorations and denture base applications [25].
This study examined whether the choice of a 3D printing machine, Asiga MAX UV or SprintRay Pro, had any significant impact on the biaxial flexural strength of BEGO TriniQ composite resin. Although slight differences in strength values were observed between the machines, the variations were not statistically significant. These findings align with the conclusions of a study by Saini et al. (2024), who noted that while different 3D printing technologies like DLP and SLA can introduce minor variations in mechanical properties, these differences are often not clinically relevant [8]. Saini et al. (2024) also pointed out that DLP technology, used in both Asiga MAX UV and SprintRay Pro, is favored for its precision and speed in dental applications, which may account for the comparable results observed in this study. The absence of a significant difference suggests that either printer can be used for producing BEGO TriniQ resin without compromising its biaxial flexural strength, making them both suitable for low-load or provisional restorations. The differences in printing resolution, layer thickness, and curing wavelengths between the Asiga MAX UV and SprintRay Pro printers might account for variations in the biaxial flexural strength of the specimens. Although the statistical analysis did not reveal significant differences, these parameters could affect the homogeneity and polymerization of the resin, warranting further investigation [8].
When comparing the BEGO TriniQ resin used in this study to other 3D-printed resins, such as VarseoSmile Crown Plus (83.6 ± 18.5 MPa), BEGO TriniQ demonstrated higher biaxial flexural strength values, ranging from 103.29 MPa to 113.60 MPa. However, BEGO TriniQ’s strength remains considerably lower than that of milled materials, such as nanohybrid composite resins (NHC), which can reach up to 237.3 MPa, and polymer-infiltrated ceramic networks (PICN), which show flexural strengths around 140.3 MPa. The reduced strength of 3D-printed resins is often attributed to differences in inorganic filler content and the printing process [8]. VarseoSmile, though designed for fixed dental restorations, also exhibits lower flexural strength than milled composites, further indicating the limitations of 3D-printed resins for high-stress applications. Milled materials remain preferable due to their superior mechanical properties. This suggests that 3D-printed resins, like BEGO TriniQ, are more suitable for low-load, non-stress areas rather than high-stress restorations [8, 29, 30].
The systematic review and meta-analysis by Saini et al. (2024) observed similar trends in flexural strength across 3D-printed resins. While DLP and SLA technologies produce materials with sufficient strength for provisional use, they often underperform in applications requiring higher strength. For example, DLP-printed bis-acrylic resins demonstrated a flexural strength of 146.37 MPa, and SLA-printed resins achieved 116.08 MPa, both comparable to BEGO TriniQ. In contrast, Graphy resins showed significantly higher strengths at 329.3 MPa, and NextDent resins reached 177.8 MPa, demonstrating the variability across 3D-printed materials. This highlights the importance of material selection in clinical applications, particularly where higher mechanical performance is required [8].
From a clinical standpoint, this study suggests that surface treatment and 3D printing machines have a limited effect on the biaxial flexural strength of 3D-printed composite resins like BEGO TriniQ. While surface treatments, such as sandblasting and etching, may improve properties like bonding, they do not significantly enhance the intrinsic strength of these materials. To improve the strength of 3D-printed composite resins, other strategies are needed, such as increasing filler content, incorporating high-performance fillers like nanofillers, optimizing the polymer matrix, and using dual-cure resin systems to achieve complete polymerization. Additionally, ensuring optimal post-curing conditions is crucial for enhancing the mechanical properties of these materials. These advancements may provide new avenues to improve the clinical viability of 3D-printed composite resins for more demanding applications [6, 31-34].
However, at present, BEGO TriniQ and similar 3D-printed resins seem better suited for low-load applications, such as temporary restorations or non-load-bearing areas, where their strength limitations are less likely to affect long-term performance. For high-stress restorations requiring greater mechanical strength and durability, clinicians may need to rely on milled materials, which offer significantly higher flexural strength and long-term reliability. Careful material selection is essential when considering the demands of restorations subjected to heavy occlusal forces, as using less mechanically robust 3D-printed resins in these cases could compromise the restoration's durability and success [33].
In terms of standards, BEGO TriniQ composite resin, with flexural strength values ranging from 103.29 MPa to 113.60 MPa, meets the ISO 10477 requirement of 100 MPa for polymer-based anterior crowns, making it suitable for such applications. However, it falls short of the ISO 6872 requirements of 300 MPa for posterior crowns and 500 MPa for fixed partial dentures (FPDs), highlighting its limitation for high-stress areas. These findings emphasize the importance of selecting appropriate materials based on clinical application. While BEGO TriniQ aligns with ISO 10477 standards for polymer-based anterior crowns and temporary restorations, its current mechanical properties limit its applicability in posterior crowns or FPDs. For such high-stress restorations, milled materials remain the preferred choice due to their superior strength and long-term reliability [35, 36].
Future research should explore advanced resin formulations with higher filler content and dual-cure systems to improve the polymerization degree and mechanical properties of 3D-printed materials. Hybrid surface treatment strategies, such as combining mechanical abrasion with chemical coupling agents, could also be investigated to determine their efficacy in enhancing both surface roughness and adhesion strength. Furthermore, evaluating the long-term performance of these materials under thermal and environmental aging conditions would provide critical insights into their clinical durability and reliability.
CONCLUSION
This study found that neither surface treatments, such as sandblasting and hydrofluoric acid etching, nor the type of 3D printing machine (Asiga MAX UV or SprintRay Pro) significantly improved the biaxial flexural strength of BEGO TriniQ composite resin. Although BEGO TriniQ exhibited higher strength than some other 3D-printed resins, it remained weaker compared to milled materials like nanohybrid composites and polymer-infiltrated ceramics. These results indicate that 3D-printed resins, including BEGO TriniQ, are better suited for low-load, non-stress applications rather than high-stress restorations, underscoring the need for further material improvements to meet higher mechanical demands.
AUTHORS’ CONTRIBUTIONS
The author confirms sole responsibility for the following: study conception and design, data collection, analysis and interpretation of results, and manuscript preparation.
LIST OF ABBREVIATIONS
| DLP | = Digital Light Processing |
| SLA | = Stereolithography |
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of this article is available from the corresponding author [M.F] upon reasonable request.
ACKNOWLEDGEMENTS
The author would like to thank the Boston University Dental Biomaterials Laboratory for providing access to equipment and resources and Dr. Russell Giordano for his guidance during the research.


