All published articles of this journal are available on ScienceDirect.
Facial Scar Management with Dermabrasion with or without Hyaluronic Acid: A Randomized Controlled Trial
Abstract
Objective
This study evaluated the effectiveness of combining dermabrasion with hyaluronic acid injection for the treatment of postoperative facial scars in a single session.
Materials and Methods
This study was conducted at Tishreen University Hospital's Department of Oral and Maxillofacial Surgery. A total of 20 patients with postoperative facial scars were randomly divided into two groups of 10. The first group received treatment with dermabrasion alone, while the second group underwent dermabrasion combined with hyaluronic acid injection into the deep reticular dermis. The healing progress was monitored, and outcomes were assessed using the Patient and Observer Scar Assessment Scale (POSAS) at follow-up intervals of 10 days, 1 month, and 6 months.
Results
Our study demonstrated progressive improvement in all assessed variables across follow-up periods. The Patient and Observer Scar Assessment Scale scores showed a significant decrease, with the most pronounced improvement observed in the group receiving dermabrasion combined with hyaluronic acid injection.
Conclusion
In conclusion, our study illustrates that combining dermabrasion with hyaluronic acid injection effectively manages facial scars in a single session, reducing the need for multiple visits. This approach presents a promising solution for efficiently addressing facial scars.
Clinical Trial Registration Number
This research is registered at the Research Registry under the identifying number researchregistry10813.
1. INTRODUCTION
When the skin experiences injury or surgical trauma, it often leads to scarring. It is estimated that over 100 million individuals develop scars each year, primarily as a result of surgical interventions [1]. Scars can pose challenges that affect daily activities and social interactions, prompting researchers to investigate various treatments for effective scar management [2]. The scar treatment market in the United States is estimated to be between $6 billion and $12 billion annually, while the global wound care market is projected to reach $15 billion to $22 billion by the end of 2024 [3].
Wounds typically heal within three weeks; however, this rapid healing process can result in scarring, particularly with deeper wounds. Large scars not only affect aesthetics but can also cause discomfort, including pain, itching, and hardness, among other symptoms [4]. Scars are alterations in the structure and appearance of skin tissues resulting from various injuries. The prevalence of scarring ranges from 40% to 70%, particularly among burn victims, post-surgical patients, and individuals who have experienced trauma. Scars can manifest in different forms, including flat, elongated, sunken, or raised, and may appear distinct from the surrounding skin. They may also exhibit symptoms, such as inflammation, erythema, dryness, and itching. Hypertrophic and keloid scars, in particular, can affect both aesthetic appearance and physiological function, contributing to anxiety and depression and ultimately impacting the quality of life for those affected [5].
Scar treatment can be a lengthy, demanding, and costly process. A variety of methods have been developed to prevent or address scars, including lasers, radiotherapy, compression, intratissue injections, surgical excision, gene therapies, and epigenetic therapies [6]. Many of these approaches necessitate multiple sessions supervised by medical professionals to achieve optimal results, making them both time-consuming and financially burdensome for patients. While topical medications are readily accessible, easy to use, and affordable, they often yield unsatisfactory results; thus, traditional treatments remain the preferred option for most patients with scars [7].
Dermabrasion is a cosmetic procedure that involves carefully scraping the skin down to the papillary dermis and superficial reticular dermis to improve the appearance of scars. The papillary dermis typically exhibits pinpoint hemorrhages, while the superficial reticular dermis shows parallel white lines [8-11]. Dermabrasion is a commonly used mechanical skin rejuvenation technique that involves systematically removing damaged or unsightly skin layers to the appropriate depth, thereby promoting the regeneration of fresh, healthy, and aesthetically improved skin. This technique provides the surgeon with precise control over the depth of the treatment, allowing for the removal of skin layers from the epidermis down to the papillary or reticular dermis, tailored to the severity and depth of the initial deformity. Dermabrasion intentionally creates a new wound in the skin to stimulate the resurfacing process. The effectiveness of this method relies on the body’s subsequent healing mechanisms. The facial skin is characterized by a dense vascular network, which ensures a continuous supply of oxygenated blood to freshly wounded areas, delivering essential nutrients to support the energy needs of actively dividing cells during their proliferation [9-12].
This study aimed to evaluate the efficacy of combining the dermabrasion technique with hyaluronic acid injections for the treatment of atrophic scars resulting from facial surgical procedures within a single clinical session.
2. MATERIALS AND METHODS
2.1. Sample
This randomized trial comprised 10 patients from the Department of Oral and Maxillofacial Surgery at Tishreen University Hospital (Fig. 1). Patients were chosen to have either two postoperative scars in the maxillofacial region or a single large scar divided into two equal parts. This research followed the ethical guidelines of the Declaration of Helsinki for human research and obtained approval from the Ethics Committee of Tishreen University with Number 107 on 17th Dec, 2020. This research is registered at the Research Registry under the identifying number researchregistry10813.
2.2. Study Design
During this randomized controlled clinical study, the sample was divided into two groups:
- The first group (study group) was comprised of 10 scars, which were treated with dermabrasion alongside intradermal hyaluronic acid injections.
- The second group (control group) was comprised of 10 scars, which were treated with dermabrasion alone.
2.2.1. Inclusion Criteria
The inclusion criteria were as follows:
- Patients aged between 18-50 years.
- Patients with a facial postoperative scar present for at least 6 weeks.
- Patients without allergies to hyaluronic acid.
- Patients without contraindications for peeling due to blood disorders.
- Patients with Fitzpatrick skin type III or IV, which is prevalent in the Middle East.
2.2.2. Exclusion Criteria
The exclusion criteria were as follows:
- Patients with photosensitivity or excessive sun exposure.
- Patients with conditions that impede the healing process, such as diabetes, immune disorders, hepatitis, thyroid issues, coagulation disorders, or leukemia.
- Patients receiving radiation therapy for oncological conditions.
- Patients on prolonged corticosteroid or anticoagulant treatment.
- Patients with skin conditions like psoriasis, vitiligo, skin infections, rashes, or skin cancer.
- Patients who have undergone treatment with botulinum toxin or fillers within the past four to six months.
2.3. Intervention
The scar surface and its surrounding area were cleaned and sterilized using a surface disinfectant (Hexamidine, Alasi, Syria) (Fig. 2). The procedure was carried out under local anesthesia, which was administered through infiltration into the dermis surrounding the scar and directly into the scar itself. Diamond burs, attached to a straight handpiece operating at a speed of 25,000-35,000 rpm, were utilized for the dermabrasion procedure (Fig. 3). The scar was held between the thumb and index finger (Fig. 3) to help control the dermabrasion process. Dermabrasion was performed with copious irrigation using a saline solution to prevent skin burns. The skin was abraded following the Bradley and Park method, with the handpiece moved parallel to the bur to prevent debris buildup and dead tissue accumulation, maintaining a 45-degree angle to the scar surface. The dermabrasion depth was controlled until punctate bleeding, signifying penetration into the papillary dermis, was achieved (Fig. 4). Subsequently, based on the group allocation (control or experimental), either the abrasion alone was deemed adequate or hyaluronic acid was injected into the deep reticular dermis at a rate of 1cc per cm2 of the scar (Fig. 5). The area was then gently cleansed using sterile gauze soaked in saline until bleeding ceased. Finally, a dressing comprising sterile gauze with a topical antibiotic (Fucine, Ibn Hayyan, Syria) was applied and left on for 24 hours.
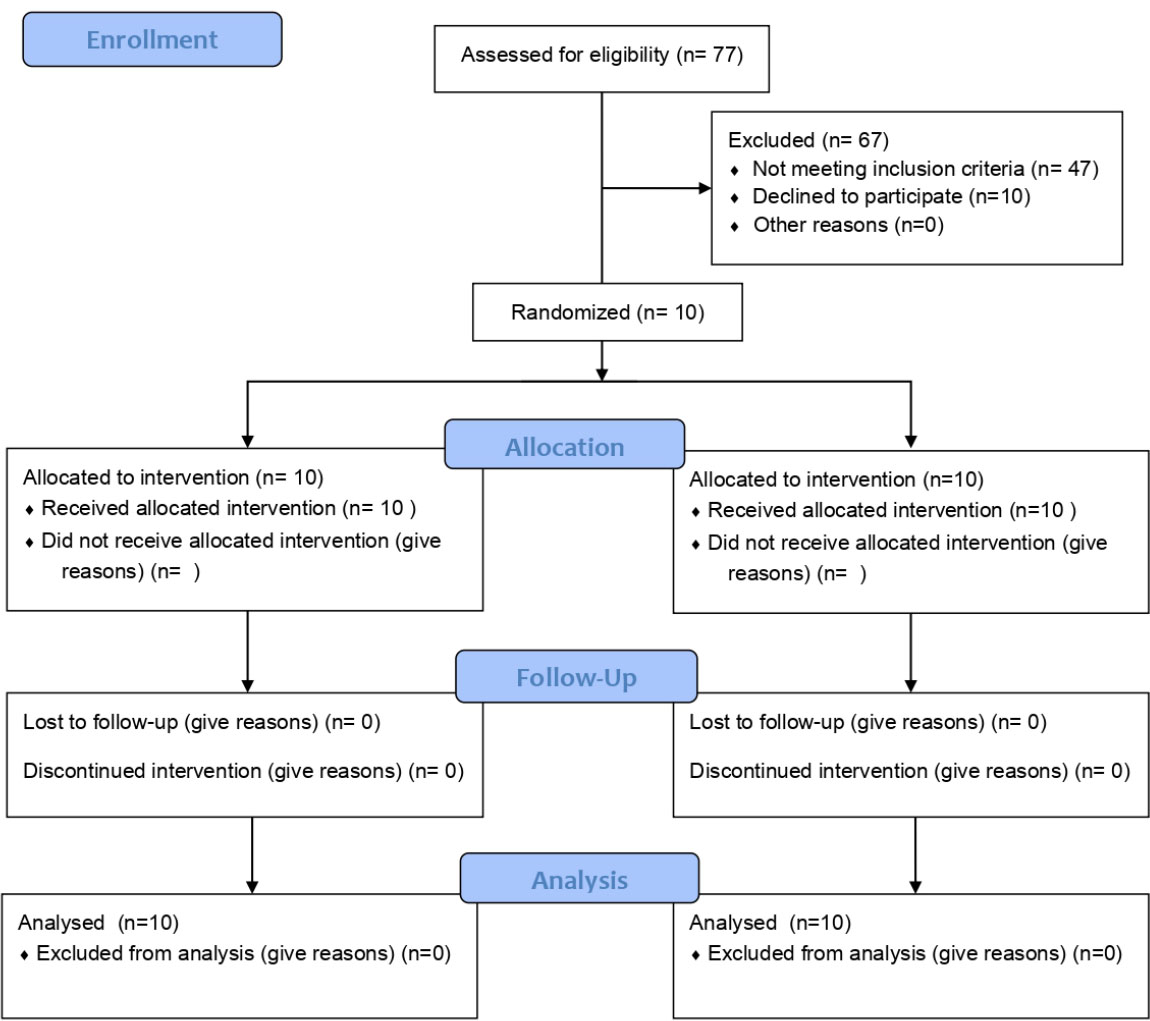
CONSORT flow diagram.

Two atrophic scars on the cheek and under the left eye.
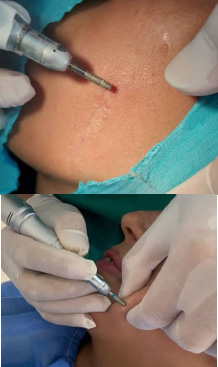
Dermabrasion with saline cooling on both scars.

The treated scar right after the dermabrasion displays punctate bleeding, which indicates the necessary depth of dermabrasion.

Hyaluronic acid injections into the dermis.
2.4. Post-operative Care and Follow-up
Patients were advised to follow the following instructions:
- Change the dressing every 24 hours for the initial 3 days.
- Maintain cleanliness by washing the area regularly with water and surface disinfectants, followed by applying a light ointment for 10 days.
- Refrain from using cosmetics for at least a week.
- Avoid sun exposure and apply sunscreen for a week.
- Apply a skin ointment (MMT Scar, American Health Care, Syria) twice daily starting a week after treatment for an additional week.
2.5. Clinical Analysis
The scars were assessed using the Patient and Observer Scar Assessment Scale (POSAS). An evaluation was carried out by both the patient and three external observers from the residents of the department of Oral and Maxillofacial Surgery at Tishreen University Hospital. The observers were unbiased in the patients' assessment, as they were unaware of the treatment method employed. Follow-ups were scheduled at 10-day, 1-month, and 6-month intervals post-intervention to monitor progress over time (Figs. 6-7).
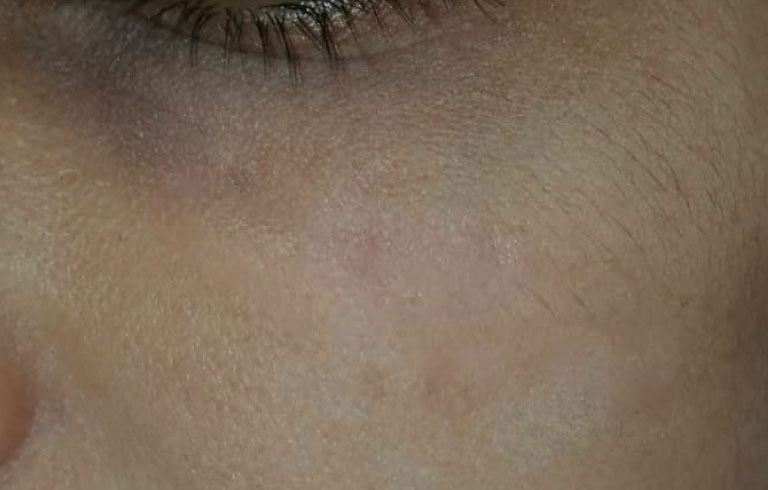
Follow up after 6 months (dermabrasion with hyaluronic acid injections).

Follow up after 6 months (dermabrasion without hyaluronic acid injections).
The Patient and Observer Scar Assessment Scale (POSAS) comprises two parts: a patient-specific scale and an observer-specific scale, each with 6 items. In both scales, every item is rated on a scale of 1 to 10, with 10 representing the most severe scar characteristics and 1 indicating healthy skin (normal pigmentation, absence of itching, etc.). The overall score for both the patient-specific and observer-specific scales was obtained by summing the scores for all six items, resulting in a total score between 6 and 60. To simplify interpretation, the total score was then divided by 6 to yield a final index score ranging from 1 to 10. The summed total represents the comprehensive score for the Scar Status Assessment Scale for both the patient and the observer.
2.6. Statistical Analysis
The statistical analysis was conducted using SPSS version 22 software (SPSS Inc., IL, USA). Descriptive statistics, such as mean and standard deviations, were employed. Mean comparisons were carried out using the Friedman test. The significance level set for the analysis was 5% (α=0.05).
3. RESULTS
3.1. Sample Description
The study sample comprised 10 patients, consisting of 4 males and 6 females, who met the specified inclusion criteria between 2021 and 2024. The age range of the patients spanned from 22 to 36 years, with a mean age of 28.30±4.2 years.
In our analysis of gender distribution, we found no statistically significant differences between the two research groups. Notably, both groups were predominantly composed of female participants, indicating a consistent representation of gender across the study. This might suggest that the findings of our research are applicable to a similar demographic, although further studies could explore gender-specific responses to the interventions employed (Table 1).
3.2. Clinical Analysis and Statistical Comparison
3.2.1. Patient Scar Assessment Scale
We noted a decline in the mean scores of the Patient Scar Assessment Scale across the entire study cohort during the follow-up periods in both treatment groups. Statistical analysis revealed significant differences, with the most substantial reduction observed in the dermabrasion group treated with hyaluronic acid injection (Table 2).
| - | Dermabrasion with HA | Dermabrasion Only | Total | p-value |
|---|---|---|---|---|
| Male | 2 | 2 | 4 | 1 |
| Female | 3 | 3 | 6 |
| Periods | ||
|---|---|---|
| Dermabrasion with HA | Dermabrasion Only | |
| Baseline | 5.61 ± 0.5 | 5.55 ± 0.3 |
| 10 days | 4.68 ± 0.61 | 5.73 ± 0.7 |
| 1 month | 2.75 ± 0.7 | 3.4 ± 0.8 |
| 6 months | 1.9 ± 0.1 | 2.06 ± 0.2 |
| p-value | 0.0001 | 0.0001 |
3.2.2. Observer Scar Assessment Scale
We identified a reduction in the mean scores of the Observer Scar Assessment Scale for the entire study population across the follow-up periods in both treatment groups. Statistically significant variances were observed, with the most significant decrease noted in the dermabrasion group receiving hyaluronic acid injections (Table 3).
| Periods | ||
|---|---|---|
| Dermabrasion with HA | Dermabrasion Only | |
| Baseline | 5.76 ± 0.7 | 5.83 ± 0.6 |
| 10 days | 4.53 ± 0.4 | 5.95 ± 0.7 |
| 1 month | 3.78 ± 0.5 | 4.15 ± 0.8 |
| 6 months | 1.75 ± 0.2 | 1.93 ± 0.3 |
| p-value | 0.0001 | 0.0001 |
4. DISCUSSION
Combination therapy has gained popularity for treating facial scarring due to the recognition that no single treatment is universally ideal for all patients in achieving desired outcomes. Opting for combination therapy is often deemed most effective in meeting patients' individual needs and expectations, leading to quicker and more efficient results. The management of these scars can be intricate, with prominent combination therapies involving the utilization of triamcinolone in conjunction with 5-fluorouracil. Research indicates that this combined approach is notably more effective compared to individual injections of each substance alone [13-16].
The efficacy of dermabrasion with or without intradermal hyaluronic acid injection in treating facial scars was investigated in a study involving 10 patients with a total of 20 scars from the Maxillofacial Surgery Department at Tishreen University Hospital in Latakia. The patients met the specified inclusion criteria between 2021 and 2024, with each scar serving as an individual study case. The intervention involved treating the scars in a single session, followed by a study with monitoring at intervals of 10 days (since complete skin resurfacing typically takes 8-10 days), then at one month, and finally at six months. The specific time intervals in our study aimed to allow sufficient time for the dermis to remodel adequately, a process that demands additional time, and also to enable melanocytes to adjust the color of the scar, thereby facilitating the acquisition of more dependable results [17-20]. Subsequently, we followed up on the outcomes of our study using the Patient and Observer Scar Assessment Scale (POSAS), which assesses all scar parameters [21]. Patient satisfaction and external observers' assessments of the scars were measured without disclosing the treatment type administered to the scars and without the researcher's involvement in the result evaluation. This impartial approach is a reliable and practical method, yielding more authentic results that enhance the credibility of the study.
Our study revealed the values of each studied variable during the respective follow-up periods in both groups: the dermabrasion group alone and the dermabrasion group with hyaluronic acid injection. These variables include pain, itching, skin color, hardness, thickness, appearance, overall scar assessment, and the general condition of the facial scar defect based on patient feedback [21]. Moreover, blood flow and pigmentation, flexibility, thickness, topography, surface area, overall assessment of dehydration, and the general condition of the facial scar defect as per the observer's evaluation showed progressive improvement throughout the follow-up periods in the research sample. The efficacy of this combined treatment technique in reshaping the treated scars synergistically is attributed to the fact that combined treatments are more effective than single treatments. Scars frequently necessitate volume restoration, tension relief, and/or tissue movement, all of which can be achieved through combined methods [22, 23]. Moreover, the safety of performing combined treatments, coupled with the synergy between different methods, plays a pivotal role in attaining optimal results [22-24].
Throughout our study, we observed a notable decrease in the average values of both the patient's and observer's assessment index for the entire study group during the follow-up periods in both treatment groups, showing statistically significant differences. The most substantial decrease was observed in the dermabrasion group with hyaluronic acid injections, reaching a significant percentage during the follow-up periods. The results converged towards the end of the follow-up, while statistically significant differences persisted in favor of the dermabrasion group with hyaluronic acid injections. These variations can be attributed to hyaluronic acid's capacity to dissolve the collagen fibers of the scar and enhance its diverse properties. The injected acid at the base of these scars also diminishes their recurrence following surgical excision. Furthermore, the acid serves as a crucial agent in reshaping these scars by binding to its specific cellular receptors, thereby initiating repair processes and safeguarding the structural integrity of the extracellular matrix [25-27].
During the initial follow-up periods (10 days and one month), we observed distinctive statistically significant differences favoring the dermabrasion group with hyaluronic acid injection, irrespective of the scar type. Subsequently, the results began to converge towards the end of the follow-up period, yet the differences persisted between the two groups. This observation can be attributed to the study's objective of treating the scar in a single session, where hyaluronic acid was administered only during the initial session. Consequently, the peak concentration of the acid was achieved during this first period. Furthermore, this phenomenon can be elucidated by the acid's penetration into all phases of the healing process at elevated levels post-dermabrasion. This accelerated the healing process post-dermabrasion, promoting visible re-epithelialization. Consequently, it aided in averting dermabrasion-related complications, such as infections and their potential impact on scar remodeling and the ultimate scar appearance [28]. This finding aligns with the study conducted by Surowitz et al. in 2011 [10], demonstrating that any treatment approach that expedites the healing process following dermabrasion yields long-term enhancements in treated scars. Additionally, the acid's capacity to moisturize the scar and regulate fibrous cell proliferation contributes to softening and maintaining moisture in the scar tissue, thereby expediting the healing process.
In our study, we did not observe any adverse side effects, such as pigmentation issues, atrophy, or subsequent infections. Our findings align with the study conducted by Urdiales-Gálvez in 2019 [29], highlighting the safety and enhanced patient satisfaction associated with hyaluronic acid injections in diverse facial treatments.
The findings of our randomized controlled trial provide valuable insights into the efficacy of dermabrasion, with and without the adjunctive use of hyaluronic acid, for facial scar management. The results suggest that both treatment modalities offer significant improvements in scar appearance, which could guide clinicians in selecting appropriate treatment options for patients. The study contributes to the existing literature by highlighting the potential benefits of hyaluronic acid in enhancing the outcomes of dermabrasion, paving the way for further research in this area.
Moreover, the implications of this study extend to understanding patient preferences and expectations regarding scar treatment. As patients increasingly seek effective and minimally invasive options, our findings may help inform shared decision-making processes between patients and healthcare providers. Future studies with larger sample sizes could further elucidate the long-term benefits and possible adverse effects associated with these treatments.
This study has several limitations that should be acknowledged. First, the relatively small sample size may limit the generalizability of our findings. While our randomized controlled design enhances internal validity, the small cohort size may reduce the statistical power to detect subtle differences between treatment groups. Future research with larger populations is needed to validate our results and provide a more comprehensive understanding of treatment efficacy.
Additionally, the follow-up period in our study was limited, which restricted our ability to assess the long-term outcomes of dermabrasion and hyaluronic acid treatment. Future studies should consider extended follow-up durations to evaluate the sustainability of treatment effects over time.
Lastly, while we aimed to control for confounding variables, individual patient characteristics and variations in scar types may influence treatment outcomes. A more diverse sample population and stratification by scar characteristics could enhance the robustness of future investigations.
CONCLUSION
Based on the parameters of our study, it can be concluded that the dermabrasion technique proves to be an effective and commendable method for addressing surgical scars, yielding satisfactory outcomes and favorable final appearances. Hyaluronic acid demonstrates a remarkable capability in expediting the healing process and enhancing the visibility of treated scars. The significance of integrating dermabrasion with hyaluronic acid injections at the scar base is to enhance the ultimate aesthetics of scars, even with a single-session application. This approach boosts patient satisfaction by eliminating the need for multiple visits and reducing the associated financial burden.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: M.N.A.: Contributed to the conceptualization, methodology, data curation, and investigation; A.K.: Proposed the methodology, carried out the investigation, and performed supervision; Z.A.: Involved in the conceptualization and writing of the manuscript.
All authors reviewed the results and approved the final version of the manuscript.
ABBREVIATION
| POSAS | = Patient and Observer Scar Assessment Scale |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Ethics Committee of Tishreen University, Syria, with Number 107 on 17th December 2020.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patients for publication of this study.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article will be available from the corresponding author [Z.A] upon reasonable request.
ACKNOWLEDGEMENTS
Declared none.


