All published articles of this journal are available on ScienceDirect.
Effect of Social Habits on the Clinical Performance of CAD/CAM Ceramic Prosthesis Fabricated from Different Ceramic Materials: 12-month Follow-up
Abstract
Background
Aesthetic restorations are fabricated using CAD/CAM technologies utilizing zirconia and lithium disilicate. These materials have shown promising results in terms of clinical performance, but the effects of social habits remain unknown. Therefore, this study aimed to investigate the impact of social habits (khat or smokeless tobacco) on the clinical performance of prostheses constructed from different CAD/CAM prosthetic materials (multilayer zirconia or lithium disilicate) by using the United States Public Health Service (USPHS).
Methods
in 2022–2023, sixth-year dental students evaluated 87 multilayer zirconia and lithium disilicate CAD/CAM restorations with modified USPHS criteria and under the direct observation of supervisors. The clinical performance was evaluated at 6 and 12 months of follow-up. The patient’s data included age, CAD/CAM material type, khat chewing, absence of smoking, arch type, side of the face, and tooth position. The statistical significance was set at p ≤ 0.05.
Results
Most of the case scores were clinically excellent (alpha) for both CAD/CAM materials at different recall intervals, but few scores were clinically acceptable (bravo) according to the USPHS criteria within the 12-month period; no charlie or delta value was recorded. The ANOVA and McNemar tests showed no significant differences in USPHS and parameter scores in both follow-up intervals. The color parameters recorded a p-value of 0.063 in the 12-month recall assessments, while marginal adaptation showed a p-value of 0.375 at the final study recall. Patient satisfaction, based on visual analog scale parameters, was very high
Conclusion
The overall USPHS scores were almost excellent in all parameters, and the clinical performance of crowns showed statistically significant differences in social habits in terms of color and retention.
1. INTRODUCTION
In the replacement of a destructive tooth structure with a dental restoration, the main goal of prosthetic rehabilitation is to achieve aesthetic and functional restoration. Over the years, this goal has been accomplished with the use of CAD/CAM restorative materials that provide excellent aesthetic and biomechanical properties [1]. Considerable advancements in dental technology have allowed for the adoption of CAD/CAM systems in modern clinics, streamlining digital workflows effectively and rapidly [2-4].
In recent decades, zirconia and lithium disilicate has been increasingly used in fixed dental prostheses [5]. Zirconia is considered stronger than lithium disilicate and offers superior physical properties; however, lithium disilicate has better aesthetic and optical properties than zirconia [6, 7]. As such, both materials offer reliable solutions and high survival rates for single-crown restorations [1]. First-generation zirconia is primarily used for frameworks covered with veneering ceramic because of its high opacity [8, 9]. Monolithic zirconia has emerged as a cost-effective solution, ensuring production efficiency [10].
Zirconia shows good optical properties without changes in its chemical makeup, featuring increased yttria content and a high cubic phase, which enhances translucency and aging resistance. However, this material has low flexural strength and fracture toughness; thus, it should be carefully used under high-stress conditions [11]. Prostheses made of lithium disilicate ceramic exhibit several notable advantages. First, its translucency mimics the natural appearance of teeth, making it ideal for tooth-colored restorations [12, 13]. It is a good alternative for dental restorations [14], and bonding with freshly cut dentin results in an excellent adhesive connection [15].
Traditional methods and materials are gradually being phased out because novel technologies have maintained success and are compatible with tissues [16]. The CAD/CAM technology can be used in fabricating zirconia and lithium disilicate restorations; only one visit is required, and no provisional phase is required [17]. It reduces human error and improves the marginal and internal fit by offering customized 3D images for different preparation designs [18].
At present, lithium disilicate glass-ceramic and multilayer zirconia are the predominant materials employed in the fabrication of restorations. Compared with other ceramic types, zirconia exhibits superior toughness and fracture resistance, but lithium disilicate ceramics offer satisfactory aesthetics and color variability [19, 20]. Lithium disilicate strengthens the bond between resin cement and dental tissues. Moreover, zirconia restorations are an effective and efficient solution for severely damaged teeth [1, 19, 21]. Monolithic zirconia resolves persistent issues, such as bone-white opacity and porcelain veneer fracture. It has a high flexural strength (600–800 MPa) [22]. Both materials have elevated survival rates when used in fabricating a single crown in either layered or monolithic forms [23].
However, several social habits may affect dental aesthetics, including smoking with electronic or conventional cigarettes. Tar and other combustion byproducts included in conventional cigarette smoke cause the discoloration and staining of dental restorations [24-26]. Furthermore, e-cigarettes cause aesthetic problems despite being marketed as safe alternatives to conventional cigarettes. Nicotine, which can interact with dental material components, causes staining, and modifies restorative clarity, may be present in the aerosol released by e-cigarette devices [27]. Moreover, chewing khat and smokeless tobacco considerably alters the color of glazed or polished CAD/CAM zirconia or conventional ceramics [28, 29], as well as the crowns made from lithium disilicate glass ceramics [30].
The Ryge criteria or the United States Public Health Service (USPHS) criteria are commonly used in the assessment of restorations since the 1970s. Jack Cvar and Gunnar Ryge examined restorations based on biological functions, aesthetic qualities, and overall functionality, employing a classification system in which alpha indicates excellent restorations, bravo denotes acceptable ones, and charlie or delta represents clinically unacceptable restorations, regardless of whether the restorations can be repaired [23, 31, 32]. Although these criteria were established more than 40 years ago, they continue to be important. They have been adjusted periodically to correspond with advancements in dental materials and methods [23].
Khat is a green leaf that naturally stimulates the central nervous system and is chewed by around 5 million people worldwide, predominantly in Yemen and southern Saudi Arabia [33]. In recent years, global tobacco demand has surged. The World Health Organization estimates that the population of smokeless tobacco users currently surpasses 1.3 billion individuals [28]. Research typically assessed ceramic discs by immersing them in staining solutions, subjecting the samples to discoloration from both sides [28, 34].
The visual analog scale (VAS) is a reliable tool for measuring subjective experiences and perceptions. It is commonly employed in surveys, questionnaires, and clinical settings. It is used to evaluate patient satisfaction and validate research findings, functioning as an effective communication tool between clinicians and patients [35]. Previous clinical studies have shown promising results regarding the clinical efficacy of CAD/CAM ceramic prostheses fabricated from lithium disilicate or zirconia [32, 36-38], but the effects of social habits (khat or smokeless tobacco) remain unclear.
2. PARTICIPANTS AND METHODS
2.1. Study Design
This study was designed to investigate the effect of social habits (Khat or smokeless tobacco) on the clinical performance of prostheses constructed from different CAD/CAM prosthetic materials (multilayer zirconia or lithium disilicate) and cemented in different (anterior or posterior) tooth areas of dental arches placed in a faculty training setting with the USPHS. All cemented prostheses were operated by sixth-year male students at the College of Dentistry, Jazan University, in the 2022–2023 academic year. The study's null hypothesis stated that no statistically significant differences in USPHS parameters would be observed concerning types of social habits, restorative materials, tooth positions, and arch types at the recall intervals.
A retrospective study was conducted on clinical performance, gathering data from patients who had received CAD/CAM prostheses made by sixth-year dental students from the Comprehensive Care Course from 2022 to 2023. The procedures were directly monitored by supervisors. This clinical study adhered to the standards of the World Medical Association's Declaration of Helsinki and received approval from the ethics committee of the College of Dentistry, University Jazan (# CODJU-2317F; June 12, 2023). The study was conducted at the Prosthetic Dental Science Department and dental intern clinics within the same institution. In addition, informed consent forms were signed by the participants.
2.2. Inclusive and Exclusive Criteria
Patients who received CAD/CAM ceramic single-crown multilayer zirconia and lithium disilicate for the maxillary and mandibular arches in the anterior (incisors or canines) and posterior (premolars or molars) teeth were included. The procedures were conducted by sixth-year male students under supervision. The patient records included phone numbers. Other inclusion criteria were vital pulp or successful endodontic treatment without apical periodontitis, absence of internal or external root resorption, and normal occlusion connection. The measurements were performed during the same daytime hours (10 am–2 pm). CAD/CAM prostheses were cemented for at least 12 months. A positive RCT indicated the absence of apical periodontitis, no internal or external root resorption, and the presence of posterior vertical stops. The exclusion criteria were parafunctional habits and periapical pathosis. Crowns made from the specified materials were excluded.
2.3. Teeth Preparation, Impression, Construction of CAD/CAM Restoration and Cementation
All clinical and laboratory procedures were conducted in accordance with the manufacturer’s guidelines and relevant textbooks [39, 40]. Protocols for ceramic tooth preparations, impression techniques, laboratory procedures for the construction of multiyear zirconia and lithium disilicate ceramic CAD/CAM prostheses, and cementation type and technique were based on the manufacturers’ instructions. Fig. (1) illustrates a clinical case, with Fig. (1A) depicting a male patient with multilayer CAD/CAM before tooth preparation, during tooth preparation, and after the cementation of separated crowns for the maxillary teeth extending from the right to the left second premolars. Fig. (1B) displays a case at the initial stage, during the application of the retraction cord and preceding the final impression, and after cementation with lithium disilicate CAD/CAM ceramic crowns on the maxillary three anterior teeth.
2.4. Patient Grouping and Assessment
The patients were contacted through mobile phones or WhatsApp for clinical examination and data collection. Charting was performed by the dentists who constructed and cemented the restorations. Examinations were performed by using a dental mirror, sharp explorer, and periodontal probe. The radiographs were obtained only when needed. Calibration for examiners was performed using the USPHS criteria with slight modification. Additional and necessary data were collected from the CS-R4 program (CSR4 plus Practice Management Software version 4, Carestream Dental LLC, Atlanta, GA, USA), and the date of cementation was verified.
2.5. Data Collections
A clinical examination was conducted, and charting sheets were utilized for each participant. Each sheet consisted of a brief explanation of the purpose of the study and the method of data collection, along with two sets of questions and the participants’ demographic information. The participants’ characteristics included patient age, type of material used for crown CAD/CAM ceramic material construction (multilayer zirconia or lithium disilicate ceramic), khat chewing (yes or no), smokeless tobacco use (yes or no), arch type (maxillary or mandibular) or side of the face (right or left), and tooth position (anterior or posterior).

A- Case with multilayer zirconia, B- Case with lithium disilicate.
The first group of questions consisted of the clinical examination criteria and USPHS for clinical case screening with modifications. Seven items were considered (i.e., anatomic form, marginal adaptation, integrity of restoration, color match, secondary caries, and retention) for scoring, as shown in Table 1 [31, 41, 42]. In this system, alpha signifies clinically excellent restoration, bravo denotes clinically acceptable restoration, and charlie or delta represents clinically unacceptable restoration or failure of the procedure, regardless of reparability. All parameters were evaluated at baseline (1-week post-cementation) and at 6 and 12 months after cementation.
The second group of questions evaluated and recognized the overall participants’ degree of satisfaction with color, morphology, and margins using the VAS. Satisfaction was assessed using the following categories: very satisfied, satisfied, fairly satisfied, and not satisfied [35, 43-45]. The clinical performance of cemented CAD/CAM restorations was evaluated and monitored for USPHS and VAS at baseline (week from cementation) and 6 and 12 months after cementation. The data were collected and recorded by two evaluators, who then assessed the reliability and accuracy of the obtained results.
2.6. Reliability and Intraclass Correlation Coefficient Test
The kappa value for the examined parameters was 0.91 (>0.8). During the clinical assessment, the examiner evaluated restorations using the MUSPHS criteria. All measurements were subjected to intra-examiner reliability with intraclass correlation coefficient values [46].
2.7. Data Analysis
Data from the applicants were summarized in an Excel spreadsheet. The outcomes of the descriptive statistical analysis were reported as mean, frequency, percentages, and standard deviation (SD) with Statistical Package for Social Science software version 28.0 (Chicago, IL, USA). The comparisons and associations among various CAD/CAM materials used, khat chewing, arch, and tooth type were evaluated using the ANOVA and the McNemar test, followed by Bonferroni’s post hoc test. Statistical significance was set at p ≤ 0.05.
3. RESULTS
The mean age of 11 patients was 22.43 ± 6.92 years. Only two participants were khat chewers, and three used smokeless tobacco. A total of 87 CAD/CAM restorations were assessed. Fig. (2) shows the contributors’ characteristics. Most of the participants had multilayer zirconia CAD/CAM restorations (72; 82.8%), did not engage in khat chewing (75; 86.2%), and did not use smokeless tobacco (72; 82.7%). The maxillary cemented crowns totaled 63 (72.4%), with a slightly higher incidence on the left side (45; 51.7%). The prevalence of anterior CAD/CAM prostheses was greater than that of posterior prostheses (60; 69.1%), and preapical X-rays were applied to only nine prostheses (10.3%).
| Parameter | Rating | Restoration Condition |
| Anatomic form | Alpha | The restoration is continuous with the anatomy of the teeth |
| Bravo | Slightly over or under contoured restoration; slightly under contoured; contact slightly open (maybe self-correcting); locally reduced occlusal height | |
| Charlie/ Delta |
* Restoration is grossly over- or under contoured, with an exposed base or dentin; faulty contact, i.e., not self-correcting; reduced occlusal height; occlusion affected * Marginal overhang present; traumatic occlusion; damaged tooth, supporting bone or soft tissues |
|
| Marginal adaptation . |
Alpha | The restoration is continuous with current anatomic form, and the sharp explorer will not catch |
| Bravo | The sharp explorer does catch, but there are no observable crevices that the explorer will penetrate | |
| Charlie/ Delta |
There is a crevice at the margin, and there is an exposed enamel margin * The crevice at the margin is very apparent, and there is exposed dentine or lute. |
|
| Integrity of restoration | Alpha | Completely intact |
| Bravo | * Crack apparent on transillumination | |
| Charlie/ Delta |
* Fracture observable * Crown lost (state at which interface debond occurred) |
|
| Color match | Alpha | Excellent color match and shade between restoration and adjacent tooth, restoration almost invisible |
| Bravo | Slightly mismatching between the restoration and the adjacent tooth, which is in the normal range of tooth | |
| Charlie/ Delta |
Color, translucence, and/or shade *Obvious mismatch, beyond the normal range *Gross mismatch/aesthetically displeasing colour, shade, and/or translucence. |
|
| Secondary caries | Alpha | No apparent caries contiguous with the restoration margin |
| Bravo | *Caries is observable contiguous with the restoration margin | |
| Retention | Alpha | Complete retention of the restoration |
| Bravo | *Mobility present |
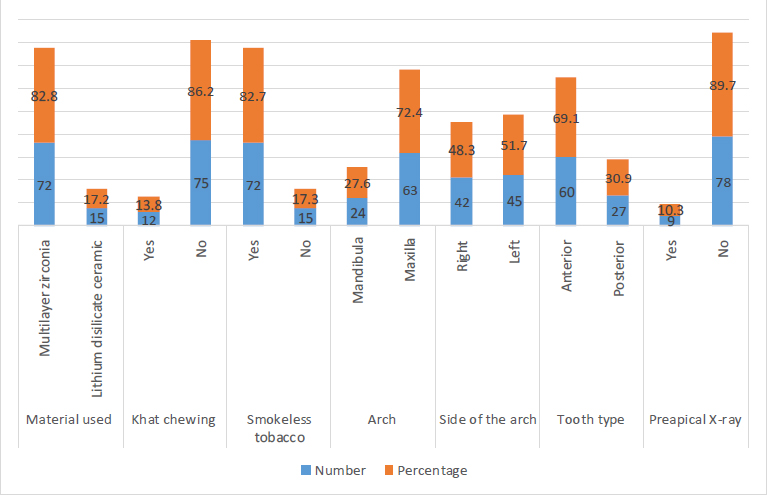
Participants characteristics.
Most of the case scores were clinically excellent (alpha) for both CAD/CAM materials at different recall intervals, but few scores were clinically acceptable (bravo) according to the USPHS criteria within the 12-month period. ANOVA and the McNemar test revealed no significant differences in USPHS and its parameter score in different follow-up intervals. The color parameters documented p of 0.063 in the 12-month recall assessments, whereas marginal adaptation verified p of 0.375 at the end of the study recall (Table 2).
| Time | Alpha | Bravo | Charlie/Delta | p-value* |
|---|---|---|---|---|
| Anatomical form | ||||
| Baseline | 81 (93.1) | 6 (6.9) | 0 (0) | - |
| 6 Months | 81 (93.1) | 6 (6.9) | 0 (0) | 1 |
| 12 Months | 78 (89.7) | 9 (10.3) | 0 (0) | 1 |
| Marginal adaptation | ||||
| Baseline | 78 (89.7) | 9 (11.3) | 0 (0) | - |
| 6 Months | 72 (82.8) | 15 (17.2) | 0 (0) | 0.625 |
| 12 Months | 69 (79.3) | 18 (20.7) | 0 (0) | 0.375 |
| Restoration integrity | ||||
| Baseline | 87 (100) | 0 (0) | 0 (0) | - |
| 6 Months | 87 (100) | 0 (0) | 0 (0) | NC |
| 12 Months | 84 (96.6) | 3 (3.4) | 0 (0) | NC |
| Color match | ||||
| Baseline | 57 (65.5) | 30 (34.5) | 0 (0) | - |
| 6 Months | 45 (51.7) | 42 (48.3) | 0 (0) | 0.125 |
| 12 Months | 42 (48.3) | 45 (51.7) | 0 (0) | 0.063 |
| Secondary caries | ||||
| Baseline | 87 (100) | 0 (0) | 0 (0) | - |
| 6 Months | 87 (100) | 0 (0) | 0 (0) | NC |
| 12 Months | 85 (97.8) | 2 (2.2) | 0 (0) | NC |
| Retention | ||||
| Baseline | 87 (100) | 0 (0) | 0 (0) | - |
| 6 Months | 87 (100) | 0 (0) | 0 (0) | NC |
| 12 Months | 78 (89.7) | 9 (10.3) | 0 (0) | NC |
| Variable | Categories | Baseline | 12 Months | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Anatomical Form | |||||||||
| Alpha | Bravo | Charlie/Delta | p-value* | Alpha | Bravo | Charlie/Delta | p-value¶ | ||
| Used material | Multilayer Zirconia | 69 (85.2) | 3 (50) | 0 (0) | 0.212 | 66 (84.6) | 6 (66.7) | 0 (0) | 0.463 |
| Lithium Disilicate | 12 (14.8) | 3 (50) | 0 (0) | 12 (15.4) | 3 (33.3) | 0 (0) | |||
| Chewing khat | Yes | 12 (14.8) | 0 (00) | 0 (0) | 0.564 | 9 (11.5) | 3 (33.3) | 0 (0) | 0.302 |
| No | 69 (85.8) | 6 (100) | 0 (0) | 69 (88.5) | 6 (66.7) | 0 (0) | |||
| Smokeless tobacco | Yes | 72 (82.8) | 0 (0) | 0 (0) | NC | 72 (82.8) | 0 (0) | 0 (0) | NC |
| No | 15 (17.2) | 0 (0) | 0 (0) | 15 (17.2) | 0 (0) | 0 (0) | |||
| Arch | Mandible | 24 (29.6) | 0 (0) | 0 (0) | 0.368 | 18 (23.1) | 6 (66.1) | 0 (0) | 0.109 |
| Maxilla | 57 (70.4) | 6 (100) | 0 (0) | 60 (76.9) | 3 (33.3) | 0 (0) | |||
| Side of the arch | Right | 39 (48.1) | 3 (50) | 0 (0) | 0.970 | 36 (46.2) | 6 (66.7) | 0 (0) | 0.506 |
| Left | 42 (51.9) | 3 (50) | 0 (0) | 42 (55.8) | 3 (33.3) | 0 (0) | |||
| Tooth type | Anterior | 50 (66.6) | 10 (80) | 0 (0) | 0.542 | 50 (66.6) | 10 (80 | 0 (0) | 0.942 |
| Posterior | 25 (33.3) | 2 (20) | 0 (0) | 25 (33.3) | 2 (20) | 0 (0) | |||
| Marginal adaptation | |||||||||
| Used material | Multilayer Zirconia | 63 (80.8) | 6 (100) | 0 (0) | 0.419 | 45 (75) | 27 (100) | 0 (0) | 0.099 |
| Lithium Disilicate | 15 (19.2) | 0 (0) | 0 (0) | 15 (25) | 0 (0) | 0 (0) | |||
| Chewing khat | Yes | 6 (7.7) | 6 (66.7) | 0 (0) | 0.007¶ | 6 (10) | 6 (22.2) | 0 (0) | 0.343 |
| No | 72 (92.3) | 3 (33.3) | 0 (0) | 54 (90) | 21 (81.8) | 0 (0) | |||
| Smokeless tobacco | Yes | 72 (82.8) | 0 (0) | 0 (0) | NC | 72 (82.8) | 0 (0) | 0 (0) | NC |
| No | 15 (17.2) | 0 (0) | 0 (0) | 15 (17.2) | 0 (0) | 0 (0) | |||
| Arch | Mandible | 21 (26.7) | 3 (33.3) | 0 (0) | 0.812 | 15 (25) | 9 (33.3) | 0 (0) | 0.683 |
| Maxilla | 57 (73.1) | 6 (66.7) | 0 (0) | 45 (75) | 18 (66.7) | 0 (0) | |||
| Side of the arch | Right | 36 (46.2) | 6 (66.7) | 0 (0) | 0.501 | 30 (50) | 12 (44.4) | 0 (0) | 0.768 |
| Left | 42 (53.8) | 3 (33.1) | 0 (0) | 30 (50) | 15 (55.6) | 0 (0) | |||
| Tooth type | Anterior | 58 (70.0) | 2 (50.0) | 0 (0) | NC | 58 (70.0) | 2 (50.0) | 0 (0) | NC |
| Posterior | 25 (30.0) | 2 (50) | 0 (0) | 25 (30.0) | 2 (50) | 0 (0) | |||
| Restoration integrity | |||||||||
| Used material | Multilayer Zirconia | 72 (82.8) | 0 (0) | 0 (0) | NC | 66 (88) | 6 (50) | 0 (0) | 0.069 |
| Lithium Disilicate | 15 (17.2) | 0 (0) | 0 (0) | 9 (12) | 6(50) | 0 (0) | |||
| Chewing khat | Yes | 12 (13.8) | 0 (0) | 0 (0) | NC | 12 (16) | 0 (0) | 0 (0) | 0.398 |
| No | 75 (86.2) | 0 (0) | 0 (0) | 63 (84) | 12 (100) | 0 (0) | |||
| Smokeless tobacco | Yes | 72 (82.8) | 0 (0) | 0 (0) | NC | 72 (82.8) | 0 (0) | 0 (0) | NC |
| No | 15 (17.2) | 0 (0) | 0 (0) | 15 (17.2) | 0 (0) | 0 (0) | |||
| Arch | Mandible | 24 (27.6) | 0 (0) | 0 (0) | NC | 21 (28.0) | 3 (25) | 0 (0) | 0.931 |
| Maxilla | 63 (80.4) | 0 (0) | 0 (0) | 54 (72.0) | 9 (75) | 0 (0) | |||
| Side of the arch | Right | 42 (48.3) | 0 (0) | 0 (0) | NC | 39 (52.0) | 3 (25) | 0 (0) | 0.319 |
| Left | 45 (51.7) | 0 (0) | 0 (0) | 36 (48.0) | 9 (75) | 0 (0) | |||
| Tooth type | Anterior | 58 (70.7) | 2 (40.0) | 0 (0) | 0.489 | 60 (71.4) | 2 (40.0) | 0 (0) | 0.484 |
| Posterior | 24 (29.3) | 3 (60.0) | 0 (0) | 24 (28.6) | 3 (60.0) | 0 (0) | |||
| Color match | |||||||||
| Used material | Multilayer Zirconia | 57 (100) | 15 (50) | 0 (0) | 0.001¶ | 42 (100) | 30 (66.7) | 0 (0) | 0.018¶ |
| Lithium Disilicate | 0 (0) | 15 (59) | 0 (0) | 0 (0) | 15 (33.3) | 0 (0) | |||
| Chewing khat | Yes | 12 (13.8) | 0 (0) | 0 (0) | 0.482 | 11 (14.3) | 1 (25.0) | 0 (0) | 0.048¶ |
| No | 75 (86.2) | 0 (0) | 0 (0) | 72 (85.7) | 3 (75.0) | 0 (0) | |||
| Smokeless tobacco | Yes | 72 (82.8) | 0 (0) | 0 (0) | NC | 70 (82.5) | 2 (100) | 0 (0) | 0.012¶ |
| No | 15 (17.2) | 0 (0) | 0 (0) | 15 (17.2) | 0 (0) | 0 (0) | |||
| Arch | Mandible | 9 (15.8) | 15 (50) | 0 (0) | 0.050¶ | 6 (14.2) | 18 (40) | 0 (0) | 0.124 |
| Maxilla | 48 (84.2) | 15 (50) | 0 (0) | 36 (85.7) | 27 (60) | 0 (0) | |||
| Side of the arch | Right | 30 (52.6) | 12 (40) | 0 (0) | 0.524 | 27 (64.3) | 15 (33.3) | 0 (0) | 0.096 |
| Left | 27 (47.4) | 18 (60) | 0 (0) | 15 (35.7) | 30 (66.7) | 0 (0) | |||
| Tooth type | Anterior | 60 (73.2) | 0 (0) | 0 (0) | 0.913 | 58 (74.3) | 2 (22.2) | 0 (0) | 0.550 |
| Posterior | 22 (26.8) | 5 (100) | 0 (0) | 20 (25.7) | 7 (77.8) | 0 (0) | |||
| Secondary caries | |||||||||
| Used material | Multilayer Zirconia | 72 (82.8) | 0 (0) | 0 (0) | NC | 72 (82.8) | 0 (0) | 0 (0) | NC |
| Lithium Disilicate | 15 (17.2) | 0 (0) | 0 (0) | 15 (17.2) | 0 (0) | 0 (0) | |||
| Chewing khat | Yes | 12 (13.8) | 0 (0) | 0 (0) | NC | 12 (16.0) | 0 (0) | 0 (0) | 0.648 |
| No | 75 (86.2) | 0 (0) | 0 (0) | 73 (84.0) | 2 (100) | 0 (0) | |||
| Smokeless tobacco | Yes | 72 (82.8) | 0 (0) | 0 (0) | NC | 72 (82.8) | 0 (0) | 0 (0) | NC |
| No | 15 (17.2) | 0 (0) | 0 (0) | 15 (17.2) | 0 (0) | 0 (0) | |||
| Arch | Mandible | 24 (27.6) | 0 (0) | 0 (0) | NC | 24 (27.6) | 0 (0) | 0 (0) | NC |
| Maxilla | 63 (80.4) | 0 (0) | 0 (0) | 63 (80.4) | 0 (0) | 0 (0) | |||
| Side of the arch | Right | 42 (48.3) | 0 (0) | 0 (0) | NC | 42 (48.3) | 0 (0) | 0 (0) | NC |
| Left | 45 (51.7) | 0 (0) | 0 (0) | 45 (51.7) | 0 (0) | 0 (0) | |||
| Tooth type | Anterior | 60 (70.0) | 0 (0) | 0 (0) | NC | 60 (70.0) | 0 (0) | 0 (0) | NC |
| Posterior | 27 (30.0) | 0 (0) | 0 (0) | 27 (30.0) | 0 (0) | 0 (0) | |||
| Retention | |||||||||
| Used material | Multilayer Zirconia | 72 (82.8) | 0 (0) | 0 (0) | NC | 69 (92) | 3 (25) | 0 (0) | 0.001¶ |
| Lithium Disilicate | 15 (27.2) | 0 (0) | 0 (0) | 6 (8) | 9 (75) | 0 (0) | |||
| Chewing khat | Yes | 12 (13.8) | 0 (0) | 0 (0) | NC | 11 (16) | 1 (100) | 0 (0) | 0.030¶ |
| No | 75 (86.2) | 0 (0) | 0 (0) | 75 (84) | 0 (0) | 0 (0) | |||
| Smokeless tobacco | Yes | 72 (82.8) | 0 (0) | 0 (0) | NC | 70 (82.8) | 2 (100) | 0 (0) | 0.894 |
| No | 15 (17.2) | 0 (0) | 0 (0) | 15 (17.2) | 0 (0) | 0 (0) | |||
| Arch | Mandible | 24 (27.6) | 0 (0) | 0 (0) | NC | 15 (20) | 9 (75) | 0 (0) | 0.024¶ |
| Maxilla | 63 (72.4) | 0 (0) | 0 (0) | 60 (80) | 3 (25) | 0 (0) | |||
| Side of the arch | Right | 42 (48.3) | 0 (0) | 0 (0) | NC | 33 (44) | 9 (75) | 0 (0) | 0.252 |
| Left | 45 (51.7) | 0 (0) | 0 (0) | 42 (56) | 3 (25) | 0 (0) | |||
| Tooth type | Anterior | 60 (73.2) | 0 (0) | 0 (0) | NC | 60 (70.6) | 0 (0) | 0 (0) | 0.706 |
| Posterior | 27 (26.8) | 0 (0) | 0 (0) | 25 (29.4) | 2 (100) | 0 (0) | |||
Table 3 presents the USPHS parameters in relation to the two types of cemented full-crown prostheses at baseline and after the end of the study (12 months). No cases of charlie or delta scores were documented in all parameters or tested variables. The anatomical forms of prostheses were clinically excellent for all parameters and variables, except in materials used in maxillary arches at baseline and at 12 months for khat chewers. The acceptable values increased at the conclusion of the study, but no significant differences were found among the variables and categories, with p ≥ 0.050. Differences in khat chewing were recorded (p = 0.007) at baseline, and no other significant differences were recorded for marginal adaptation parameters. The number of acceptable cases increased at 12 months for all variables and categories. Similarly, the majority of the cemented and assessed
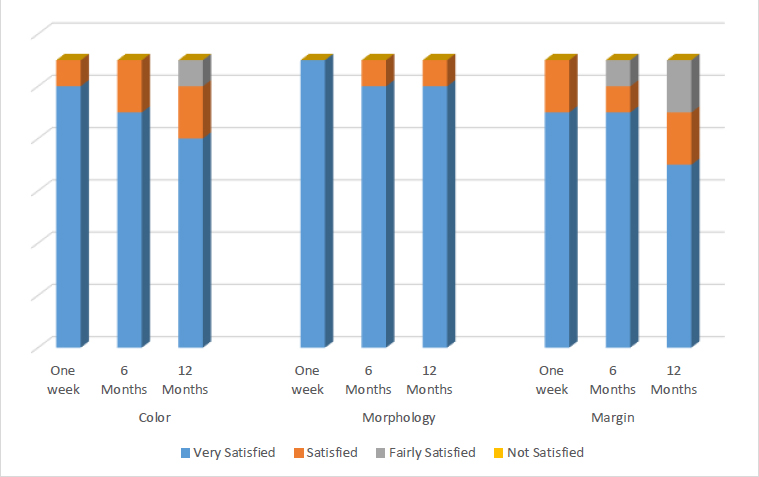
Participant satisfaction using VAS.
restorations exhibited excellent values at baseline for most variables and categories concerning the marginal integrity parameter. The values of bravo (acceptable) increased toward the end of the study for the same tested variables and categories, but no significant differences were observed.
Compared with other parameters, color matching recorded a higher number of clinically acceptable values for both types of restoration materials, and arches at baseline showed significant differences (p = 0.001, 0.050). Significant differences in materials used, khat chewing, and use of smokeless tobacco were found in the 12-month assessment period (p = 0.018, 0.048, and 0.012, respectively). No changes were recorded in the secondary caries parameter in relation to the variable tested at 6 and 12 months after recall. A significant difference in the retention parameter was found at the 12-month period for material, khat chewing, and arch (p = 0.001, 0.030, and 0.024, respectively).
Overall, participant satisfaction regarding the morphology of the cemented CAD/CAM crowns ranged from very satisfied to satisfied, according to the VAS. In addition, ratings of very satisfied and fairly satisfied for color and margin were recorded during the recall periods. The color parameter score decreased from 10 cases to 9 and 8 cases, ultimately dropping to the very satisfied categories after 6 and 12 months. A slight decline from the very satisfied category to the satisfied category on the morphological parameters was found after the 6th and 12th-month follow-ups (from 11 cases to 10 cases), and all cases were unchanged during the 12-month follow-up. In relation to crown margin parameters, a fairly satisfied rating was recorded in three cases after 6 and 12 months (Fig. 3).
4. DISCUSSION
In the field of prosthodontics, CAD/CAM restorations are being increasingly utilized. The use of these fabricated materials for dental restorations inside the mouth lacks substantial scientific evidence despite positive findings from clinical studies [2, 47]. The overall survival rate is defined as the permanent presence of a prosthesis despite complications being considered acceptable and without requiring replacement [48]. This study investigated the effect of social habits (khat or smokeless tobacco) on the clinical performance of cemented multilayer zirconia and lithium disilicate CAD/CAM at different teeth in a faculty training setting using the USPHS.
In this study, the case scores were clinically excellent (alpha) for both CAD/CAM materials at different recall intervals for 87 multilayer zirconia and lithium disilicate CAD/CAM restorations, but few scores were clinically acceptable (bravo) in the USPHS criteria within the 12-month period. The null hypotheses were partially accepted, given that statistically significant differences were observed at recall intervals in the USPHS parameters in relation to the types of social habits, types of material, and types of arches. This result was in accordance with previous studies that demonstrated highly successful clinical performance after the use of the USPHS criteria [35, 37, 38].
In this study, at the 12th month of follow-up, the anatomical forms of prostheses were clinically excellent for all parameters and variables, except when both materials were used for khat chewers and maxillary arches. The acceptable values increased at the end of the study, but no significant differences among all variables and categories were observed, with p ≥ 0.050. These findings were similar to those of Konstantinidis et al., who reported that zirconia crowns show excellent performance after 12 months, and they are clinically acceptable, with no significant relationships among variables [36]. For the marginal adaptation parameter, khat chewing cases were rated as excellent and clinically acceptable, whereas the number of acceptable cases did not increase after 12 months of follow-up. Khat chewing showed a significant difference at the baseline assessment possibly because of the assessed number of restorations in khat chewers and nonchewers. Of the restorations, 100% of cases without smokeless tobacco use were rated as excellent at the 12th month of follow-up for marginal adaptation. These results could be related to the findings of previous studies. Cases without Charlie scores were recorded during the 1-year recall period [36-38].
Regarding color match, at the 12th month of recall, statistically significant differences were found, regardless of the type of material. The baseline of color match for khat chewing and smokeless tobacco variables had 100% excellent scores, but the number of acceptable cases increased in the 12th month. These results were consistent with those of Fasbinder et al., who revealed that 87% of lithium disilicate cases had mild discoloration after 24 months of follow-up [49]. Moreover, previous studies have demonstrated the influence of nutrition, dental hygiene, and smoking on discoloration [50, 51]. Our findings revealed significant differences between types of material, and this difference may be explained by variation in sample size between the two materials. The good marginal adaptation of cemented restorations prevents the development of caries. Some studies, including our present study, observed no changes in the secondary caries parameter in relation to variables tested at 6 and 12 months after recall [37, 38].
Regarding retention, 100% of cemented crowns were recorded with excellent scores at baseline and 6 months; however, the number of acceptable cases increased at 12 months. The present results were consistent with previous clinical investigations, which found no loss of retention for monolithic zirconia crowns [37]. However, Moura et al. [38] observed loss of retention after 6 months of follow-up for lithium disilicate. Notably, crown retention loss is associated with adhesive cementation type and mechanical tooth preparation settings, such as the area, height, width, and convergence degree of prepared surfaces [52, 53].
An in vitro study showed high values of color change parameters for advanced lithium disilicate anatomical crowns after immersion in social habits, including khat and smokeless tobacco use [30]. The cemented restorations constructed from zirconia and lithium disilicate CAD/CAM materials showed similar clinical outcomes in the biological, technical, and aesthetic behavior of both materials [54].
Overall, the results of most of the parameters assessed in this clinical study indicated non-significant results. This could be related to various factors, including the small sample size, the assessed different periods, the specific brand of multilayer zirconia and lithium disilicates utilized, their composition, the generation of adhesive cements employed, and the application of CAD/CAM technology in the fabrication of the assessed prostheses. All these resulted in smooth surfaces that minimize the adhesion of external stains potentially caused by khat and smokeless tobacco. Previous studies showed that khat and smokeless tobacco result in clinically acceptable color changes and minimal alterations in surface roughness after immersion for different periods on zirconia and lithium disilicate samples [28, 29]. The chemical structures and content of lithium disilicate provide numerous benefits, such as expedited processing through rapid sintering, applicability for full and partial coverage and veneers, and suitability for anterior or posterior teeth [30].
Regarding patient satisfaction based on VAS, our study showed that most patients were very satisfied in all parameters. This result was similar to the findings of many clinical studies, which showed high satisfaction mentioned for similar parameters [32, 52-55]. In the present study, participants reported similar satisfaction ratings for the colors and margins of both tested materials. These outcomes aligned with those of a previous systematic review and clinical study [1, 36]. In addition, a similar finding was documented 24 months after the recall for lithium disilicate ceramic and 12 months after the recall of zirconia crowns [36].
The clinical implications are that the CAD/CAM ceramic prostheses fabricated from multilayer zirconia or lithium disilicate demonstrated promising clinical performance after 1 year of follow-up. However, social habits may substantially affect the clinical performance of CAD/CAM ceramic crowns. The limitations of the present study were the limited number of patients, the restricted number of crowns evaluated, and the short evaluation period.
CONCLUSION
After 1 year of recall, the overall survival rate was high, and the clinical performance of the crowns (multilayer zirconia or lithium disilicate) showed statistically significant differences in color and retention. These differences were attributed to social habits. Long-term clinical studies with a large sample size are required to adequately evaluate the potential effect of the assessed social habits with other types of habits and staining materials on the clinical performance of CAD/CAM ceramic prostheses.
AUTHOR'S CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| VAS | = Visual analog scale |
| USPHS | = United States Public Health Service |
| SD | = Standard deviation |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study received approval from the ethics committee of the College of Dentistry, Jazan University, Saudi Arabia (# CODJU-2317F; June 12, 2023).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
ACKNOWLEDGEMENTS
Declared none.


