All published articles of this journal are available on ScienceDirect.
Impact of Maternal Status on Dental Pain Perception in Adult Women: A Cross-sectional Study
Abstract
Background
Pain perception is a complex and subjective experience influenced by various factors, including demographic, genetic, and psychosocial characteristics. Previous research has established differences in pain perception between sexes and age groups; however, the impact of maternal status on dental pain perception in women remains understudied.
Methods
This cross-sectional study investigated the association between childbirth and perceived pain during dental procedures in adult women. Participants completed a questionnaire that assessed their demographic information, maternal history, dental anxiety, and pain perception using validated scales.
Results
Women who had experienced childbirth reported significantly higher actual pain levels during dental procedures compared to those who had not (p = 0.004). In contrast, no significant differences were found between the groups in expected pain (p = 0.995), pain that motivated dental visits (p = 0.610), or trust in the dentist (p = 0.693).
Conclusion
This study demonstrates an association between maternal status and heightened dental pain perception, potentially linked to childbirth-related neuroplastic changes. These findings highlight the need for tailored pain management strategies for mothers in dental care.
Practical Implications
Dentists should be aware of the potential for increased pain sensitivity in mothers and adjust their pain management strategies accordingly. This may include combining pharmacological and nonpharmacological approaches.
1. INTRODUCTION
Pain is an inherently individualistic and subjective experience that presents challenges for researchers and clinicians. Its perception varies greatly among individuals and is influenced by the complex interplay of biological and psychosocial factors, including demographic charac-teristics, genetic, and psychosocial characteristics. These factors collectively yield a unique constellation of influ-ences on individual pain experiences [1]. Notably, sex, age, and ethnicity have been identified as significant determinants for chronic pain and responses to experi-mentally induced pain. Furthermore, genetic and psycho-social factors exert combined effects on clinical and experimental pain intensities.
Epidemiological evidence has consistently demons-trated a higher prevalence of chronic pain in women compared to men. For instance, a nationwide survey in the United States revealed that women reported experiencing any pain over the preceding 90 days more frequently than men, often describing their pain as persistent and dis-tressing [2]. Additionally, studies have identified distinct factors influencing pain quality between genders in conditions such as burning mouth syndrome, with dep-ression and alcohol consumption linked to pain quality in men, and educational level and marital status associated with pain experiences in women [3].
Age-related differences in pain perception have also been extensively studied, suggesting that older adults may exhibit decreased sensitivity to acute and superficial pain stimuli but increased sensitivity to prolonged deep-tissue pain [4].
Stress, defined as a state of disrupted homeostasis or harmony, plays a crucial role in pain perception. Both physical and psychological stressors trigger multifaceted responses involving neural, endocrine, and behavioral adaptations. This response is characterized by the acti-vation of the sympathetic nervous system and the Hypothalamic-Pituitary-Adrenal (HPA) axis, accompanied by changes in pain thresholds and various physiological and behavioral parameters [5, 6].
Research has shown that stress and anxiety can exacerbate pain by activating the hippocampus, sugges-ting strategies to mitigate pain by modulating hippo-campuscampal activity during potentially painful pro-cedures [7]. Individual personality traits, such as a propensity for catastrophizing, can influence the impact of stressors on emotional well-being. Although findings remain mixed, some studies have indicated a higher tendency among women to engage in catastrophizing [8].
Hormonal factors, such as estrogen levels, have been implicated in pain sensitivity and hormonal fluctuations linked to variations in pain perception and sex-specific responses to pain [9].
The perinatal period induces significant neuro-biological changes in women, enhancing susceptibility to stress and its effects on pain perception. Both historical and current stress can alter maternal brain function and affect circuits involved in stress regulation, empathy, and maternal motivation. Thus, interventions aimed at redu-cing stress in mothers could potentially mitigate adverse effects on the maternal brain and, by extension, pain perception [10, 11].
Changes in the HPA axis during pregnancy and the postpartum period aimed at adapting to maternal stress highlight a critical window of vulnerability and adapt-ability. Disruptions in this adaptive process owing to severe stress can lead to dysregulation and consequent mood disorders, further complicating the relationship between maternal status and pain perception [12].
Despite the extensive research on pain perception and its modulators, few studies have directly examined the influence of maternal status on dental pain perception in women. This study aimed to fill this gap by offering insights into how maternal status uniquely affects of experiences of dental pain in women.
2. MATERIALS AND METHODS
2.1. Subjects
This observational, descriptive, cross-sectional study was approved by the ethics committee of the Dental college at King Abdulaziz University, Jeddah, KSA (No. 138-11-24). The study was conducted between June 2019 and January 2020 at a dental clinic in King Abdulaziz University Hospital. Adult females were approached in the waiting room and informed of the study. If they met the sampling criteria, they were asked to sign a consent form before enrolment in the study.
2.2. Inclusion Criteria
Healthy females of childbearing age (20 – 50 years old) who needed routine dental treatment, including scaling and simple restoration, were enrolled in the facility.
2.3. Exclusion Criteria
Participants were excluded if emergency dental treatment was required, severe dental pain was present, or if the treatment was complicated or lengthy (oral surgery or surgical extractions).
2.4. Sample Size Calculation
Females of childbearing age who underwent routine dental restoration or periodontal scaling were approached and asked to participate in the study. Eligible participants were informed about the research and, if they agreed, were asked to sign an informed consent form.
A post-hoc power analysis was conducted using G*Power to determine the adequacy of the sample size for detecting differences in perceived pain between mothers and non-mothers. With an observed effect size of d = 0.705 and a sample size of 52 mothers and 24 non-mothers, the analysis indicated a power of 0.805, confir-ming that the sample size was adequate for the analysis conducted.
2.5. Questionnaire
The questionnaire started with a brief explanation of the aim of the study and then a statement indicating to the participants that their answers would be stored and transmitted securely to protect confidentiality.
A questionnaire with two parts was written in English and translated into Arabic. The Arabic version was given to participants. The first part of the questionnaire was per-formed immediately, and the second part was performed after completion of their routine dental treatment. Validated scales were used to measure pain and anxiety.
2.6. Pre-treatment Questions
This section included sociodemographic data (age, sex, nationality, occupation, education, and area of residence], and maternal history (number of children, and type of birth).
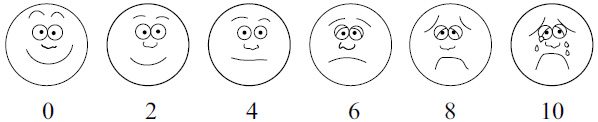
The Wong Baker face scale.
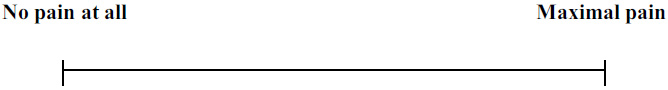
Visual analog scale.
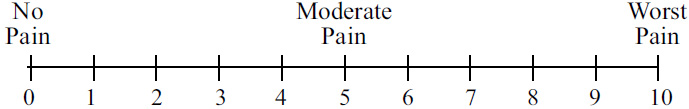
Numerical pain scale.
Anxiety was assessed using the Modified Dental Anxiety Scale (MDAS), which consists of five questions and summed together to produce a total score of 5–25. It can be integrated into everyday dental practice as a clinical aid and screen for dental anxiety and has shown high reliability and validity [13].
Participants rated their anticipated pain using the Wong-Baker Face Scale, the visual analogue scale, and the numerical pain scale (Figs. 1-3). The Wong-Baker Face Scale shows a series of faces ranging from a happy face at 0 (no pain), to a crying face at 10 “hurts like the worst pain imaginable” [14]. This scale is easy to use and comprehend and has high validity and reliability.
The Visual Analogue Scale (VAS) shows a straight line with the endpoints defining extreme as ‘no pain at all’ and ‘pain as bad as it could be.’ Participants were asked to mark their anticipated pain level between the two endpoints and the distance between ‘no pain at all’ and the mark was used to assess the level of pain [15]. This scale is one of the most frequently used scales in clinical settings and is valid and reliable.
The Numerical Pain Scale (NPS) shows a line with numbers marked from 0 (no pain) to 10 (hurts like the worst pain imaginable). Participants rated their anticipated pain [15]. Previous studies have found this scale to be valid and reliable.
2.7. Post-treatment
Following treatment, participants rated their actual pain levels using the Wong-Baker face pain scale, VAS, and NPS.
For validity, the questionnaire was revised by two senior experts in preventive dentistry, and modifications were made according to their comments.
2.8. Statistical Analysis
Statistical analysis was conducted using a cross-sectional design to explore the association between childbirth and perceived pain during dental procedures as measured by the NPS. Participants were divided into two groups based on their childbirth history. Descriptive statistics, including frequencies, percentages, means, standard deviations, medians, and Interquartile Ranges (IQR), were used to summarise the data.
Robust imputation techniques were employed to handle missing data and ensure the integrity of the analysis. The dataset revealed the following missing values: expected pain (3), actual pain (1), income (1), deliveries (1), and stress (3). Medians were imputed for missing values for numeric variables (expected pain, actual pain), whereas modes were used for missing values for categorical variables (income, deliveries, stress).
An inferential analysis was performed using a two-sample t-test to compare mean pain scores between women who had undergone childbirth and those who did not. For non-normally distributed variables, such as expected pain, actual treatment pain, and trust in the dentist, the Mann-Whitney U test was employed. Spearman’s rank correlation was used to assess the relationships between pain scores and other ordinal variables, such as trust in the dentist and expected pain. Furthermore, linear regression analysis was conducted with actual pain as the response variable and maternity status as the main predictor; income level and pain experienced when visiting the dentist were added as potential confounders. All statistical analyses were performed using R version 4.4.1.
3. RESULTS
3.1. Descriptive Statistics
The study cohort comprised 78 women, of whom 53 had experienced childbirth (Group 1), and 25 had not (Group 2) (Table 1),. Participants were predominantly non-Saudi (54%), followed by Saudi Arabians (46%). The income distribution indicated that a larger proportion of parti-cipants earned between 3000 and 10000 (40%), while fewer participants reported incomes of less than 3000 (33%) or more than 10000 (27%). The overall mean score of expected pain reported during dental visits was 3.88 on a scale of 0 to 10.
3.2. Pain Measures by Childbirth Status
A significant difference in the actual pain experienced during the dental procedures was observed between the two groups (Table 2). Women who had undergone childbirth reported a higher median pain score of 4.4 (SD=2.35), compared to 2.76 (SD=2.08) for those who had not (t-test -2.99(CI -2.77: -0.54), p=0.004). This indicates that mothers reported significantly higher levels of pain than non-mothers, suggesting that childbirth status may influence perceived pain during dental procedures. In contrast, no significant differences were found in the expected pain during dental visits between the two groups, with both reporting a median pain score of 5 (p=0.995). Similar findings were observed for pain that made one visit the dentist and trust in the dentist, with no significant differences noted between the groups (p=0.610 and p=0.693, respectively).
3.3. Correlation Analysis
Spearman correlation analysis showed no significant correlation between actual pain and trust in the dentist (-0.06, p=0.66) or expected pain during dental visits (-0.04, p=0.77). However, a notable correlation was observed between trust in the dentist and expected pain, with a correlation coefficient of 0.93 (p < 0.001), suggesting that higher trust in the dentist was associated with higher expected pain. (Table 3).
3.4. Linear Regression Analysis
Linear regression analysis was conducted to examine the relationship between actual pain levels during dental procedures and maternal status, adjusted for potential confounders, including maternity status (baby delivery), income level, and pain upon visiting the dentist (Table 4). The model revealed a significant effect of maternity status on reported pain levels.
| Variables | % | N |
|---|---|---|
| Nationality | 46 | 36 |
| Saudi | 54 | 42 |
| Non-Saudi | - | - |
| Income | - | - |
| Less than 3,000 | 33 | 26 |
| 3,000-10,000 | 40 | 31 |
| More than 10,000 | 27 | 21 |
| Childbirth | - | - |
| Yes | 68 | 53 |
| No | 32 | 25 |
| Dental treatment makes you nervous | - | - |
| Yes | 55 | 43 |
| No | 45 | 35 |
| Fear of Anesthesia | - | - |
| Yes | 78 | 61 |
| No | 22 | 17 |
| Sound of instruments | - | - |
| Yes | 36 | 28 |
| No | 64 | 50 |
| Sharp instruments | - | - |
| Yes | 23 | 18 |
| No | 78 | 60 |
| Rubber dam | - | - |
| Yes | 1 | 1 |
| No | 99 | 77 |
| Jaw pain | - | - |
| Yes | 1 | 1 |
| No | 99 | 77 |
| Nothing | - | - |
| Yes | 6 | 5 |
| No | 94 | 73 |
| Trust your doctor Median (IQR) | 8(4) | |
| Pain that makes you visit dentist Median (IQR) | 7(4) | |
| Expected pain during visit Median (IQR) | 5(2) | |
| Actual pain mean (SD) | 3.88(2.50) | |
The results indicated that, on average, women who had undergone childbirth reported higher pain levels (coefficient = 1.504, 95% CI: 0.30 to 2.71) compared to those who had not. This finding suggests a significant association between childbirth history and perceived pain during dental procedures.
In contrast, the variables “pain to visit” and “income levels” did not demonstrate statistically significant effects on actual pain, with confidence intervals including zero (pain to visit: 95% CI: -0.03 to 0.41; income category 2: 95% CI: -0.98 to 1.58; income category 3: 95% CI: -1.56 to 1.34). This indicates that while these variables were included as potential confounders in the model, they did not significantly contribute to explaining the variations in actual pain levels.
| - | Median | p-value |
|---|---|---|
| Actual pain score** | ||
| Childbirth | - | - |
| Yes | 4.5 | 0.007 |
| No | 2.5 | |
| Expected pain | ||
| Childbirth | - | - |
| Yes | 5 | 0.916 |
| No | 5 | |
| Pain to visit the dentist | ||
| Childbirth | - | - |
| Yes | 7 | 0.512 |
| No | 7 | |
| Trust in dentist | ||
| Childbirth | - | - |
| Yes | 8 | 0.62 |
| No | 9 |
| - | Actual Pain | Excepted Pain | Trust in Doctor | Pain to Visit the Dentist |
|---|---|---|---|---|
| Actual pain | 1.0 | - | - | - |
| Expected pain | -0.04 (0.77) | 1.0 | - | - |
| Trust in doctor | -0.06 (0.66) | 0.93* (<0.001) | 1.0 | - |
| Pain to visit the dentist | 0.19 (0.11) | 0.12 (0.32) | 0.08 (0.61) | 1.0 |
| Variable | Coefficient | P-value | 95% CI |
|---|---|---|---|
| Unadjusted model | |||
| Childbirth (yes) | 1.66 | 0.006 | 0.49 to 2.81 |
| Adjusted model | |||
| Childbirth (yes) | 1.5 | 0.015 | 0.30 to 2.71 |
| Pain experienced to visit Dentist | 0.19 | 0.09 | -0.03 to 0.41 |
| Income (3,000-10,000) | 0.3 | 0.64 | -0.98 to 1.58 |
| Income (>10,000) | -0.12 | 0.88 | -1.56 to 1.34 |
In summary, the results of this study demonstrated a statistically significant increase in the level of pain perceived by women who had undergone childbirth during dental procedures compared to those who had not. These findings underscore the importance of considering childbirth history in pain management and treatment planning in dental care settings. The lack of significant correlations between other pain-related anticipatory measures and demographic factors suggests that childbirth experiences uniquely influence pain perception.
4. DISCUSSION
This cross-sectional study investigated the intriguing question of whether maternal status influences dental pain perception in women. Our findings provide compelling evidence that mothers reported significantly higher actual pain during dental procedures than women who had not given birth, highlighting a potential modulation of pain sensitivity associated with childbirth. These findings align with studies suggesting increased pain sensitivity in mothers due to neuroplastic changes during the perinatal period [17]. For instance, a study conducted by Barba-Müller et al. in 2019 demonstrated that pregnancy-induced adaptations in brain regions like the amygdala and hippocampus contributed to heightened sensitivity to nociceptive stimuli. Similarly, Dekel et al., in 2019, found that postpartum changes in the Hypothalamic-Pituitary-Adrenal (HPA) axis exacerbated stress responses, which could amplify pain perception in clinical settings. Thus, our study adds to this body of evidence by uniquely exploring dental pain as a specific modality [27].
Several potential mechanisms might explain the elevated pain sensitivity observed in mothers [18]. One possibility involves alterations in the HPA axis activity [19]. Pregnancy and postpartum periods are characterized by a physiological adaptation of the HPA axis, leading to a state of hypo-reactivity to stress [20]. However, adverse experiences during pregnancy or postpartum depression can disrupt this adaptive process, resulting in HPA axis dysregulation and increased sensitivity to pain stimuli [21]. Our study did not directly assess HPA axis function, but future research exploring this pathway could shed light on its role in modulating pain perception in mothers.
Another potential mechanism involves modifications to brain regions involved in pain processing. Pregnancy and motherhood are associated with structural and functional changes in brain regions such as the amygdala, hippo-campus, and anterior cingulate cortex [22]. These areas play crucial roles in pain modulation, emotional regu-lation, and stress responses. It is conceivable that these neuroplastic changes, while adaptive to maternal care-giving behaviors, may also lead to a heightened sensitivity to nociceptive input, as observed in our study. Similar findings were reported by Kim et al. in 2016 [23], who found that various conditions, such as extreme stress, trauma, and mental disorders, can disturb normative changes in the brain, making mothers more vulnerable. Due to the remarkable plasticity of the maternal brain, it may be more sensitive to both positive and negative experiences, such as stress and interventions, throughout pregnancy and in the early postpartum phase.
Our findings resonate with previous research sugg-esting that mothers exhibit increased sensitivity to threat-related stimuli and experience more negative effects than non-mothers [23]. This heightened emotional reactivity might amplify pain perception through descen-ding pain modulation pathways originating in the prefrontal cortex and limbic system [24]. Additionally, altered stress per-ception and processing capabilities in mothers could contribute to increased pain sensitivity via stress-induced activation of pain-promoting pathways in the brainstem and spinal cord [25].
It is important to note that our study did not find significant differences between mothers and non-mothers in terms of expected pain or pain that motivated them to visit the dentist. This suggests that the observed difference in actual pain perception was not likely due to preexisting biases or expectations regarding dental procedures. However, further research with larger sample sizes and longitudinal designs is required to confirm these findings and explore the underlying mechanisms in greater detail.
Although our study demonstrated heightened pain in mothers during dental procedures, further research is needed to explore the specificity and extent of this sensi-tization. Understanding the specificity of pain sensitization can inform targeted pain management strategies for mothers in various healthcare settings [26]. The clinical implications of this study are far-reaching, particularly in promoting patient-centered care in dental settings. Dentists must recognize that motherhood-related neuroplastic changes may predispose women to heightened sensitivity to dental stimuli. Accordingly, treatment plans should be individualized to account for this increased pain perception, ensuring that mothers receive adequate support before, during, and after procedures. Furthermore, integrating education on maternal pain sensitivity into dental training programs could prepare future practitioners to handle this unique patient demographic effectively. Therefore, further research should evaluate the association between child-bearing and generalized hyperalgesia across different modalities.
Our findings suggest a potential heterogeneity in pain responses among mothers. While childbirth appears to be a general sensitizing factor, individual differences in childbirth experiences (vaginal vs. cesarean, postpartum complications, emotional well-being) might further modu-late pain perception [27]. Additionally, pre-existing chronic pain conditions, genetic predispositions, and psychological factors like anxiety and depression could interact with childbirth-induced neuroplasticity, contributing to indi-vidual variations in pain sensitivity [28]. Future research investigating these interactions is crucial for personalized pain management approaches in mothers.
It is crucial to investigate the long-term consequences of childbirth-induced pain sensitization. Specifically, the duration of the effect and vulnerability to chronic pain development is worth exploring. Alternatively, the effects of specific interventions or lifestyle modifications on pro-moting neuroplastic changes that normalize pain response after childbirth need to be investigated. Investigating the reversibility and long-term trajectory of pain sensitization offers valuable insights into preventive strategies and rehabilitation programs for mothers with chronic pain.
This study highlights the need for tailored pain manage-ment strategies for mothers in dental settings. Therefore, dentists should consider a combination of pharmacological and non-pharmacological approaches. Pharmacological regimens might require adjustments based on individual pain profiles and potential interactions with breastfeeding or other maternal medications [29]. Non-pharmacological techniques such as cognitive-behavioral therapy, mind-fulness practices, and relaxation strategies can empower mothers to actively manage their pain and reduce reliance on medication [30]. Furthermore, fostering a patient-centered environment that acknowledges and validates the pain experiences of mothers is crucial for building trust and improving dental care outcomes [31].
The link between childbirth and pain sensitivity extends beyond the dental setting and highlights the importance of integrating pain management into broader maternal health care [32]. Prenatal and postpartum care should incorporate pain assessment and education as routine components. Additionally, healthcare providers across various specialties should be aware of the potential heightened pain sensitivity in mothers and adjust their diagnostic and treatment approaches accordingly. Holi-stically recognizing and addressing the pain experiences of mothers can significantly improve their overall well-being and quality of life.
While our study provides valuable insights into the link between maternal status and dental pain perception, it has some limitations that warrant further consideration.
The cross-sectional design precluded causal inferences regarding the impact of childbirth on pain sensitivity. We cannot definitively claim that childbirth causes heightened pain perception, but only that mothers reported expe-riencing more actual pain during dental procedures than non-mothers. Longitudinal studies that track pain per-ception before and after childbirth are necessary to establish causality. Additionally, the sample size of the present study was moderate, which potentially limited the generalisability of our findings. Large-scale studies with more diverse populations are required to confirm the observed associations and explore potential subgroup differences. Further, our study relied solely on self-reported pain scores that are inherently subjective and prone to bias. Factors such as anxiety, fear of dental procedures, and cultural influences can affect the manner in which individuals report pain. Incorporating objective pain measures such as functional Magnetic Resonance Imaging (fMRI) or Electroencephalography (EEG) could provide more objective data on pain processing differences between mothers and non-mothers.
Our study did not account for all other potential confounding factors that might influence pain perception, such as specific birth experiences, differences in delivery mode (vaginal vs. caesarean), presence of postpartum complications, or breastfeeding status. Chronic and preexisting chronic pain conditions may also interact with childbirth-induced neuroplasticity, thereby affecting pain perception. Psychological factors such as anxiety, dep-ression, or fear of dental procedures could influence pain reporting and perception. Socioeconomic factors, such as access to healthcare, education levels, and social support networks, can influence pain experiences and pain management strategies. Future research addressing these limitations will strengthen our understanding of the complex interplay between motherhood and pain perception.
Although our study explored dental pain as a model for nociceptive processing, it is unclear whether the observed sensitization is specific to dental stimuli or can be generalized to other types of pain. Further studies investi-gating pain sensitivity in mothers across different pain modalities are necessary to better understand the broad implications of childbirth-induced neuroplasticity. By acknowledging and addressing these limitations, we can interpret our findings with greater caution and pave the way for future research to refine our understanding of pain perception in mothers and optimize pain management strategies for this population.
CONCLUSION
In conclusion, the present study provides compelling evidence that mothers report significantly higher actual pain during dental procedures than women who have not given birth. These findings suggest that motherhood, potentially through childbirth-induced neuroplastic changes, may alter pain processing pathways, leading to increased pain sensitivity. Although the underlying mecha-nisms remain unclear, our findings have significant implications for both dental practitioners and maternal healthcare providers. Dentists should recognize increased pain sensitivity in mothers and adapt treatment protocols accordingly. Strategies include building trust through clear communication, using tailored local anesthetics, and employing nonpharmacological methods like cognitive-behavioral techniques and mindfulness. Pre-visit pain assessments can further enhance patient comfort and satisfaction. Holistically recognizing and addressing the pain experiences of mothers within a broader maternal healthcare framework is crucial to ensure their well-being and quality of life. This study also highlights the need for further research to investigate the specificity and long-term consequences of childbirth-induced pain sensiti-zation. Future research with longitudinal designs, objective pain measures, and consideration of individual differences and contributing factors could pave the way for personalized pain management strategies for mothers, empowering them to manage pain effectively and thrive throughout motherhood.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| MDAS | = Modified Dental Anxiety Scale |
| VAS | = Visual Analogue Scale |
| NPS | = Numerical Pain Scale |
| fMRI | = functional Magnetic Resonance Imaging |
| EEG | = Electroencephalography |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This observational, descriptive, cross-sectional study was approved by the ethics committee of the Dental college at King Abdulaziz University, Jeddah, KSA (No. 138-11-24).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article will be available from the corresponding author [H.A.] upon reasonable request.
ACKNOWLEDGEMENTS
Declared none.


