All published articles of this journal are available on ScienceDirect.
Sociodemographic Influences on Periodontal Treatment: A Retrospective Analysis at Taif University Dental Hospital
Abstract
Introduction/Objectives
Periodontal diseases are highly prevalent global oral health issues that affect millions of people and lead to significant risks, including tooth loss and reduced quality of life. This study comprehensively analyzed the clinical profiles and demographics of patients treated at the periodontal clinic of Taif University Dental Hospital to investigate the associations of sociodemographic factors, including sex, age, and race, with variations in treatment modalities.
Methods
This study received approval from the Taif University Scientific Research Ethics Committee. Electronic patient records of 2,635 patients were analyzed. Descriptive and inferential statistics, including the F test and chi-square test, were used to examine treatment patterns, with significance set at 5%.
Results
This study examined 2,369 periodontal treatment patterns among 1,047 patients. Scaling and root planing emerged as the predominant treatment, constituting 94% of all procedures. Sex disparities were evident, with 42.14% of male patients and 10.10% of female patients undergoing treatment. White and Asian patients underwent more soft tissue and periodontal surgeries, with Asians receiving more crown-lengthening procedures. Crown lengthening was more frequent among patients aged >40 and 20–29 years. Periodontal surgery was common in patients aged >50 years, while gingivectomy was more frequent among those aged 30–49 years. Overall, treatment frequency was highest in the 20–49-year-old age group.
Conclusion
Significant associations observed between periodontal procedures and age and race highlight the need for individualized care, early risk assessments, and patient education. Public health initiatives, including community-based screenings, are essential for equitable access to care.
1. INTRODUCTION
Periodontal diseases include a wide range of conditions, ranging from gingivitis to severe periodontitis [1, 2]. Gingivitis, the most common form of gingival inflammation, is a reversible response to bacterial plaque that typically resolves by the effective removal of biofilm from the teeth [3]. On the other hand, periodontitis is a chronic inflammatory condition that affects the supporting tissues around teeth, posing significant risks to oral health, including tooth loss and reduced quality of life [4-6]. The onset of this condition is triggered by dysbiosis of the subgingival oral microbiome [7]. Notably, the progression of periodontitis is believed to result from a complex interaction between bacterial infection and the host immune response, with behavioral factors, such as smoking, exacerbating the condition [5, 8]. The 2017 classification of periodontal and peri-implant diseases and conditions introduced by the American Academy of Periodontology (AAP) and the European Federation of Periodontology (EFP) highlights the importance of early identification of risk factors to enable precise diagnosis and effective prevention strategies [9].
Periodontal diseases affect a significant portion of the population, with global prevalence estimates ranging between 20% and 50% [10]. The high incidence of periodontal disease across different age groups, including adolescents, adults, and older people, underscores its significance as a pressing public health issue [11, 12]. In Saudi Arabia, where the prevalence of periodontitis is 51%, it represents a considerable health concern [13]. The burden of periodontal disease necessitates not only refined clinical management but also a comprehensive understanding of the sociodemographic determinants influencing treatment accessibility and outcomes. Therefore, this study aimed to address these critical gaps by providing a comprehensive analysis of the clinical characteristics of patients treated at the periodontal clinic of Taif University Dental Hospital from 2017 to 2023. Through meticulous examination of demographic variables, such as age, sex, and race, alongside treatment modalities, it sought to explore the associations between these factors and the types of treatments received. Furthermore, by identifying these relationships, the study aimed to uncover patterns that inform the development of targeted prevention and treatment strategies. Beyond clinical practice, the findings hold transformative potential to influence health policies by addressing disparities in care delivery and guiding the strategic allocation of healthcare resources.
2. MATERIALS AND METHODS
This study was approved by the Taif University Scientific Research Ethics Committee (approval number: 45-112) and conducted according to the principles of the Declaration of Helsinki. Informed consent was obtained from all individual participants included in the study. Electronic medical records of 2,635 patients aged ≥12 years who visited the Predoctoral Dental Clinic at Taif University between September, 2017, and December, 2023, were analyzed. Comprehensive data extraction forms were developed to collect demographic information, including age, sex, nationality, and race. Patients were categorized by sex and nationality, while racial classification followed the National Institutes of Health guidelines, identifying participants as American Indian or Alaskan Native, Asian, Black or African American, Native Hawaiian or Other Pacific Islander, or White. Age groups included 13–19, 20–29, 30–39, 40–49, and ≥50 years. Periodontal procedures were classified into the following five categories: scaling and root planing, crown lengthening, gingivectomy, periodontal surgeries (e.g., open flap debridement and guided tissue regeneration), and soft tissue surgeries (e.g., root coverage and free gingival graft) (SAGER guidelines were followed).
2.1. Statistical Analysis
Categorical variables were analyzed descriptively and presented as absolute and relative frequencies, whereas quantitative variables were reported as means, standard deviations, and medians. A parametric approach was used for inferential analysis due to the large sample size. Mean values were compared using the F test from the analysis of variance model. Associations between categorical variables were evaluated using chi-square and Fisher’s exact tests when expected frequencies were below five, with statistical significance set at 5% (α = 0.05). Data analysis was performed using IBM SPSS Statistics for Windows, version 29 (IBM Corp., Armonk, N.Y., USA).
3. RESULTS
3.1. Sample Characteristics
Among 2,635 patients, 1,047 received treatment at periodontal clinics, accounting for 39.69% of patients and resulting in 2,369 procedures performed. The mean number of procedures per patient was 2 (± 3.5). Of the total patients, 2,437 were men, with 1,027 (42.14%) undergoing periodontal treatment, whereas only 20 (10.10%) of 198 women received such procedures (Table 1). Table 2 illustrates age-related treatment trends, revealing a low treatment prevalence of 11% among patients aged 13–19 years. In contrast, approximately 50% of patients aged 20–49 received treatment, with the highest rates in the 30–39-year-old (51.3%) and 40–49 year old (48.8%) age
| Sex | Total Patients | Periodontal Patients | Periodontal Procedures | |||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Male | 2,437 | 92.48% | 1,027 (42.14%) | 98.08% | 2,321 | 97.97% |
| Female | 198 | 7.52% | 20 (10.10%) | 1.91% | 48 | 2.02% |
| Total | 2,635 | 100% | 1,047 (39.69%) | 100% | 2,369 | 100% |
| Age | Total Patients | Periodontal Patients | Periodontal Procedures | |||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| 13–19 y | 490 | 18.60% | 54 (11.02%) | 5.16% | 103 | 4.35% |
| 20–29 y | 899 | 34.12% | 412 (45.82%) | 39.35% | 1,017 | 42.93% |
| 30–39 y | 479 | 13.66% | 246 (51.35%) | 23.50% | 554 | 23.39% |
| 40–49 y | 360 | 12.05% | 176 (48.88%) | 16.81% | 394 | 16.63% |
| ≥50 y | 407 | 15.45% | 159 (39.06%) | 15.19% | 301 | 12.71% |
| Total | 2,635 | 100% | 1,047 (39.73%) | 100% | 2,369 | 100% |
| Nationality | Periodontal Patients | Mean | Standard Deviation | Median | Periodontal Procedures | p-value | ||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | |||||
| Saudi Arabia | 522 | 49.86% | 2.3 | 3.0 | 2.0 | 1,205 | 50.87% | <0.008* |
| Egypt | 155 | 14.80% | 1.6 | 1.2 | 2.0 | 256 | 10.81% | |
| Syria | 15 | 1.43% | 2.1 | 1.8 | 2.0 | 31 | 1.31% | |
| Yemen | 78 | 7.45% | 2.1 | 1.4 | 2.0 | 165 | 6.96% | |
| India | 19 | 1.81% | 2.3 | 4.0 | 1.0 | 44 | 1.86% | |
| Afghanistan | 53 | 5.06% | 3.9 | 7.4 | 2.0 | 212 | 8.95% | |
| Bangladesh | 59 | 5.64% | 1.9 | 1.2 | 2.0 | 114 | 4.81% | |
| Burma | 21 | 2.01% | 2.2 | 1.0 | 2.0 | 46 | 1.94% | |
| Pakistan | 57 | 5.44% | 1.8 | 1.1 | 2.0 | 102 | 4.31% | |
| Sudan | 41 | 3.92% | 3.3 | 9.7 | 2.0 | 137 | 5.78% | |
| Others | 27 | 2.58% | 2.1 | 1.0 | 2.0 | 57 | 2.41% | |
| Total | 1,047 | 100% | - | - | - | 2,369 | 100% | |
groups. When examining the number of patients visiting periodontal clinics and periodontal procedures performed across different nationalities, Saudi Arabian patients had the highest percentage of periodontal procedures (Table 3). The mean number of procedures per patient was 2.3 for Saudis and 3.9 for Afghans, with a significant difference between nationalities (p < 0.008, F test).
3.2. Periodontal Procedures
Table 4 presents the trend analysis of periodontal procedures performed at Taif University Dental Hospital. Scaling and root planing emerged as the predominant treatments, accounting for 94% of all procedures. Periodontal and soft tissue surgeries were the less frequently performed treatments, each comprising 0.76% of the procedures.
| Procedure | N | % |
|---|---|---|
| Scaling and root planing | 2,226 | 93.96 |
| Crown lengthening | 77 | 3.25 |
| Gingivectomy | 30 | 1.27 |
| Periodontal surgeries | 18 | 0.76 |
| Soft tissue surgeries | 18 | 0.76 |
| Total | 2,369 | 100% |
Fig. (1) shows the summary of trend analysis of the number of patients and periodontal procedures performed from 2017 to 2023. The mean number of procedures per year was 2.1 (± 3.3), reflecting moderate variation over the years. Specifically, the data show a general downward trend in the number of procedures performed, with the mean decreasing from 4.1 in 2017 to 1.5 in 2023. In 2017, 75% of the patients who visited the hospital underwent periodontal procedures. A marked change in this percentage was observed between 2017 and 2018. This reduction can be attributed to the opening of the university dental hospital in 2017, which initially attracted a high volume of patients. However, in 2018, the number of patients decreased as students focused on completing treatments for their existing cases, following the patient-centered approach policy. Additionally, the COVID-19 pandemic further reduced visits in 2020. Patient numbers gradually increased again in 2021 as more students entered clinical training. The variation was significant (p < 0.001), as determined by the F tests.
The association between sex and the frequency of various periodontal procedures performed was not statistically significant (Table 5). However, significant associations were found between age and specific procedures (Table 6). For scaling and root planing, statistically significant associations were observed in both the 20–29 and 40–49-year-old age groups. Similarly, for crown-lengthening procedures, statistical significance was found in the 20–29-, 40–49-, and ≥50-year-old age groups. Regarding gingivectomy procedures, statistical significance was observed in the 30–39- and 40–49 year-old age groups. Significant associations were noted for periodontal surgery in the 20–29 and ≥50 year-old age groups but not for soft tissue surgeries (Fig. 2).
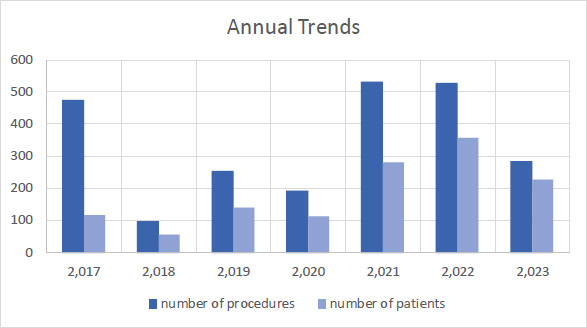
Annual trends in the number of patients and periodontal procedures.
| Periodontal Procedures | Sex | Yes | No | Total | p-value | ||
|---|---|---|---|---|---|---|---|
| N | % | N | % | ||||
| Scaling and root planing | Male | 2,179 | 93.9% | 142 | 6.1% | 2,321 | 0.363 |
| Female | 47 | 97.9% | 1 | 2.1% | 48 | ||
| Crown lengthening | Male | 77 | 3.3% | 2244 | 96.7% | 2,321 | 0.405 |
| Female | 0 | 0.0% | 48 | 100% | 48 | ||
| Gingivectomy | Male | 30 | 1.3% | 2291 | 98.7% | 2,321 | 1 |
| Female | 0 | 0.0% | 48 | 100% | 48 | ||
| Periodontal surgeries | Male | 17 | 0.7% | 2,304 | 99.3% | 2,321 | 0.301 |
| Female | 1 | 2.1% | 47 | 97.9% | 48 | ||
| Soft tissue surgeries | Male | 18 | 0.8% | 2,303 | 99.2% | 2,321 | 1 |
| Female | 0 | 0.0% | 48 | 100% | 48 | ||
| Periodontal Procedures | Age Group | Yes | No | Total | p-value | ||
|---|---|---|---|---|---|---|---|
| N | % | N | % | ||||
| Scaling and root planing | 13-19 y | 97 | 94.2% | 6 | 5.8% | 103 | 0.927 |
| 20–29 y | 942 | 92.6% | 75 | 7.4% | 1017 | 0.018* | |
| 30–39 y | 513 | 92.6% | 41 | 7.4% | 554 | 0.123 | |
| 40–49 y | 384 | 97.5% | 10 | 2.5% | 394 | 0.001* | |
| ≥ 50 y | 290 | 96.3% | 11 | 3.7% | 301 | 0.063 | |
| Crown lengthening | 13-19 y | 2 | 1.9% | 101 | 98.1% | 103 | 0.773 |
| 20–29 y | 54 | 5.3% | 963 | 94.7% | 1,017 | <0.001* | |
| 30–39 y | 17 | 3.1% | 537 | 96.9% | 554 | 0.783 | |
| 40–49 y | 2 | 0.5% | 392 | 99.5% | 394 | <0.001* | |
| ≥ 50 y | 2 | 0.7% | 299 | 99.3% | 301 | 0.007* | |
| Gingivectomy | 13-19 y | 2 | 1.9% | 101 | 98.1% | 103 | 0.378 |
| 20–29 y | 14 | 1.4% | 1003 | 98.6% | 1017 | 0.677 | |
| 30–39 y | 12 | 2.2% | 542 | 97.8% | 554 | 0.030* | |
| 40–49 y | 0 | 0% | 394 | 100% | 394 | 0.006* | |
| ≥ 50 y | 2 | 0.7% | 299 | 99.3% | 301 | 0.418 | |
| Periodontal surgeries | 13-19 y | 0 | 0% | 103 | 100% | 103 | 1 |
| 20–29 y | 3 | 0.3% | 1,014 | 99.7% | 1017 | 0.024* | |
| 30–39 y | 5 | 0.9% | 549 | 99.1% | 554 | 0.587 | |
| 40–49 y | 3 | 0.8% | 391 | 99.2% | 394 | 1 | |
| ≥ 50 y | 7 | 2.3% | 294 | 97.7% | 301 | 0.005* | |
| Soft tissue surgeries | 13-19 y | 2 | 1.9% | 101 | 98.1% | 103 | 0.183 |
| 20–29 y | 4 | 0.4% | 1013 | 99.6% | 1017 | 0.075 | |
| 30–39 y | 7 | 1.3% | 547 | 98.7% | 554 | 0.157 | |
| 40–49 y | 5 | 1.3% | 389 | 98.7% | 394 | 0.204 | |
| ≥ 50 y | 0 | 0% | 301 | 100% | 301 | 0.154 | |
Table 7 presents the relationship between race and the frequency of different periodontal procedures. Notably, statistically significant findings were observed in Asian patients who underwent crown-lengthening procedures. For periodontal and soft tissue surgeries, statistical significance was observed in both the Asian and White populations. However, no statistically significant associations were found in scaling, root planing, or gingivectomy between the two races. Regarding the gingivectomy procedures, statistical significance was noted for Saudis (Table 8).
4. DISCUSSION
This study aimed to analyze patient clinical profiles from the periodontal clinic of Taif University Dental Hospital (2017–2023) to explore correlations between patient characteristics and periodontal treatment.
In this study, scaling and root planing were the common treatments. This is consistent with established evidence, highlighting their efficacy in managing periodontal disease, particularly in patients with mild-to-moderate periodontitis [14]. The widespread use of scaling and root planing reflects the critical role of controlling
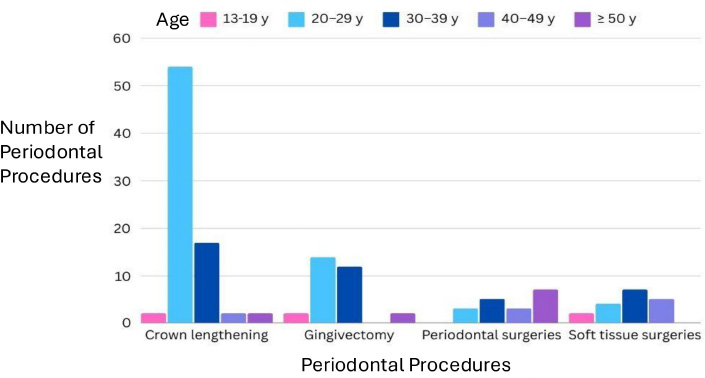
Periodontal procedures by age.
| Periodontal Procedures | Race | Yes | No | Total | p-value | ||
|---|---|---|---|---|---|---|---|
| N | % | N | % | ||||
| Scaling and root planing | White | 1586 | 94.1% | 100 | 5.9% | 1,686 | 0.745 |
| Black | 145 | 97.3% | 4 | 2.7% | 149 | 0.076 | |
| Asian | 496 | 92.7% | 39 | 7.3% | 535 | 0.167 | |
| Crown lengthening | White | 48 | 2.8% | 1638 | 97.2% | 1,686 | 0.084 |
| Black | 4 | 2.7% | 145 | 97.3% | 149 | 1 | |
| Asian | 25 | 4.7% | 510 | 95.3% | 535 | 0.035* | |
| Gingivectomy | White | 26 | 1.5% | 1660 | 98.5% | 1,686 | 0.059 |
| Black | 0 | 100% | 149 | 100% | 149 | 0.256 | |
| Asian | 4 | 0.7% | 531 | 99.3% | 535 | 0.223 | |
| Periodontal surgeries | White | 8 | 0.5% | 1678 | 99.5% | 1,686 | 0.012* |
| Black | 0 | 100% | 149 | 100% | 149 | 0.624 | |
| Asian | 10 | 1.9% | 525 | 98.1% | 535 | 0.002* | |
| Soft tissue surgeries | White | 18 | 1.1% | 1668 | 98.9% | 1,686 | 0.007* |
| Black | 0 | 100% | 149 | 100% | 149 | 0.624 | |
| Asian | 0 | 100% | 535 | 100% | 535 | 0.019* | |
| Periodontal Procedures | Nationality | Yes | No | Total | p-value | ||
|---|---|---|---|---|---|---|---|
| N | % | N | % | ||||
| Scaling and root planing | Saudi | 1,123 | 93.2% | 82 | 6.8% | 1,205 | 0.110 |
| Non-Saudi | 1,103 | 94.8% | 61 | 5.2% | 1,164 | ||
| Crown lengthening | Saudi | 40 | 3.2% | 1165 | 96.8% | 1,205 | 0.847 |
| Non-Saudi | 37 | 3.2% | 1,127 | 96.8% | 1,164 | ||
| Gingivectomy | Saudi | 21 | 1.7% | 1,184 | 98.3% | 1,205 | 0.035* |
| Non-Saudi | 9 | 0.8% | 1,155 | 99.2% | 1,164 | ||
| Periodontal surgeries | Saudi | 8 | 0.7% | 1,197 | 99.3% | 1,205 | 0.584 |
| Non-Saudi | 10 | 0.9% | 1,154 | 99.1% | 1,164 | ||
| Soft tissue surgeries | Saudi | 13 | 1.1% | 1,192 | 98.9% | 1,205 | 0.069 |
| Non-Saudi | 5 | 0.4% | 1,159 | 99.6% | 1,164 | ||
microbial biofilms and mitigating inflammation in periodontal treatment protocols [15, 16]. This finding underscores the importance of focusing on early diagnosis and non-invasive interventions to control microbial biofilms and inflammation, thereby reducing the progression to advanced disease states. However, periodontal surgeries, such as open flap debridement, osseous surgery, and guided tissue regeneration, were less frequently performed, representing only 0.76% of all procedures. These interventions are typically reserved for advanced periodontitis cases characterized by significant attachment loss, osseous defects, and the necessity for regenerative therapy [17]. Although these procedures are essential for managing severe periodontal disease and promoting tissue regeneration, their lower prevalence in this dataset reflects the predominance of milder periodontal conditions among the patient population [17-19]. Therefore, these patterns emphasize the critical need for clinicians to prioritize preventive and non-surgical approaches while ensuring timely referral for surgical interventions when necessary.
Crown lengthening procedures accounted for 3.25% of treatments in this study, with a higher prevalence observed among Asians and individuals aged >40 years. These findings are consistent with those of previous research, which suggests that crown lengthening is more frequently required among patients aged 30–50 years [20]. Soft tissue surgeries and gingivectomies were less commonly performed in this study, comprising 0.76% and 1.27% of treatments, respectively. These surgical interventions are typically employed to address gingival health and aesthetic concerns in specific conditions, such as managing gingival overgrowth, aesthetic crown lengthening, gingival recession, and improving overall periodontal health [18, 19, 21]. Although these procedures were not prevalent in the study population, gingivectomies were notably more frequent among individuals aged 30–49 years and within the Saudi population than within the non-Saudi population. This trend suggests that non-surgical interventions, such as scaling and root planing, are prioritized due to their effectiveness in managing periodontal disease. Furthermore, the lower occurrence of surgical procedures could reflect the success of preventive measures and non-invasive treatments in maintaining gingival health in the studied population. These findings call for enhanced public health initiatives to raise awareness about surgical options and their benefits in specific cases, particularly in populations showing lower uptake.
The data revealed a sex disparity in periodontal treatment, with a higher percentage of men (42.14%) receiving treatment than women (10.10%). This finding aligns with existing research, which suggests notable sex differences in periodontal health and treatment [22, 23]. Socio-cultural norms and healthcare-seeking behaviors play a pivotal role in shaping these disparities. Studies have reported that women tend to exhibit greater oral health awareness, preventive behaviors, and oral hygiene practices than men [22, 24, 25]. However, despite their heightened awareness, women may face barriers to accessing dental care, including financial limitations, caregiving responsibilities, and societal expectations [26]. Women also reported experiencing higher levels of dental anxiety and phobia than men, which may hinder timely treatment-seeking [26, 27]. Abe et al. [22] highlighted a significant sex gap in oral hygiene behaviors, with men demonstrating poorer oral hygiene during late adolescence than women, which correlates with a higher risk of gingival bleeding. Studies suggest that men are generally at greater risk of severe periodontal disease than women, potentially explaining the higher treatment rates observed among men than among women in this study [8, 28]. These factors collectively indicate that the sex disparity in treatment does not solely reflect differences in disease prevalence but also variations in healthcare-seeking behaviors and access to care. Therefore, policymakers and clinicians should address these challenges by developing community-based oral health programs targeting women and providing affordable care and support for overcoming dental anxiety. Campaigns promoting oral health awareness and encouraging preventive behaviors in men could also further reduce the disease burden.
The data revealed a distinct age-related pattern in periodontal treatment, with the lowest and highest engagement observed in patients aged 13–19 (11%) and 20–49 (~50%) years, respectively. A significantly higher frequency of periodontal surgeries was observed among patients aged ≥50 years. This finding aligns with the results of existing literature highlighting age as a significant factor in periodontal disease development and progression [8, 10, 23, 25]. As individuals age, they become more susceptible to periodontal tissue breakdown due to cumulative exposure to risk factors, such as poor oral hygiene, chronic inflammation, and systemic health conditions [29]. Aging is also associated with physiological changes in periodontal tissues, including gingival recession, loss of periodontal attachment, and alveolar bone resorption, all of which contribute to periodontal disease onset and progression [30, 31]. Therefore, the observed age-related treatment patterns correspond with the natural progression of periodontal diseases over the lifespan [30]. The peak treatment engagement among individuals aged 20–49 years reflects a critical life period during which periodontal disease onset and progression are more likely to occur [32]. Factors, such as hormonal fluctuations, lifestyle behaviors, and systemic health conditions, can also exacerbate periodontal inflammation and tissue destruction during this time [33]. Individuals in this age group may be more aware of their oral health needs and proactive in seeking treatment to address periodontal issues and prevent further disease progression [30]. Conversely, the lower treatment engagement observed among pediatric patients likely reflects a lower prevalence of severe periodontal disease in this group, along with potential challenges in accessing specialized periodontal care for children [34]. These findings underscore the need for tailored interventions at different life stages. Additionally, integrating periodontal education into school health programs can promote routine screenings and early preventive strategies for adolescents. Routine screenings are crucial for middle-aged adults, who are at higher risk of periodontal disease, enabling early diagnosis and intervention. Targeted outreach programs for older adults can also help address existing gaps in care and improve overall periodontal health.
The frequency of periodontal procedures was significantly associated with race in this study. Saudis had a higher incidence of gingivectomies, whereas Afghans exhibited the highest average number of procedures, highlighting a potential disparity in periodontal healthcare needs across nationalities. Asian and White patients underwent more periodontal and soft-tissue surgeries, with crown-lengthening procedures being more prevalent among Asians than among White patients. These findings align with research suggesting that periodontal disease prevalence and treatment vary significantly across ethnic and racial groups [35]. Studies have consistently demonstrated differences in the prevalence, severity, and treatment outcomes of periodontal disease among racial and ethnic populations [35, 36]. For instance, African American and Hispanic populations are known to experience higher rates of periodontal disease than White individuals [37]. Moreover, disparities in access to dental care and periodontal service utilization are observed among racial and ethnic groups, with minority populations usually facing obstacles, such as financial limitations, language barriers, and a lack of culturally competent care [38]. The observed differences in periodontal treatment utilization among nationalities in this study may reflect underlying disparities in oral health awareness, genetic predispositions, cultural practices, access to healthcare, and socio-economic factors [36]. For example, Afghans may have higher treatment needs and a greater prevalence of periodontal disease due to limited access to preventive services, cultural influences on oral hygiene, or genetic susceptibility [39]. Conversely, Saudis may exhibit different healthcare-seeking behaviors or have better access to resources, which could influence their periodontal treatment utilization [13]. To address these disparities, policymakers should implement culturally tailored oral health education programs, increase access to affordable dental care, and promote training in culturally competent care among healthcare providers.
This study demonstrated that treatment engagement peaks in middle adulthood, highlighting the significance of early intervention and preventive strategies in maintaining periodontal health throughout life [34]. Early detection and management of periodontal diseases can prevent or delay the progression to more severe periodontitis, thereby reducing the necessity for invasive treatments [34, 40]. Targeting modifiable risk factors, such as smoking cessation, improved dietary habits, and enhanced oral hygiene practices, can significantly reduce the burden of periodontal diseases and promote overall oral health across all age groups [34, 40]. Encouraging regular dental check-ups and implementing comprehensive periodontal screening protocols can also facilitate the early identification of risk factors, allowing for timely and effective interventions. Clinically, the disparities in treatment utilization highlight the need for individualized care, incorporating routine risk assessments to identify high-risk populations and facilitate early interventions. Educating patients on the importance of regular dental visits and periodontal health for overall well-being is also crucial. On a policy level, integrating periodontal care into public health initiatives, with community-based screening programs targeting underserved populations, is vital. Therefore, strengthening collaborations between healthcare providers and public health authorities can enhance preventive efforts and ensure equitable access to care across all demographics.
4.1. Study Limitations
This study provides valuable insights into periodontal treatment demographics at Taif University Dental Hospital. However, its single-center design limits the generalizability of the findings. By concentrating on sex, age, and nationality, the study did not account for other factors, such as socioeconomic status and oral hygiene. Unmeasured confounders, such as smoking status and overall health, may also influence the findings. The small number of women further restricts applicability across the sexes. Therefore, to mitigate these limitations, future studies should adopt a prospective, multicenter design with comprehensive data collection, encompassing a larger and more balanced sample. Furthermore, additional demographic and health-related variables should be incorporated, particularly focusing on socioeconomic status and behavioral factors, such as smoking and oral hygiene habits. This approach would provide a deeper understanding of periodontal treatment disparities and yield more generalizable conclusions.
CONCLUSION
This study provides valuable insights into the sociodemographic factors influencing periodontal treatment utilization at Taif University Dental Hospital. The findings reveal significant associations between treatment frequency and patient race and age, highlighting the need for tailored approaches to address disparities in access to care. Treatment trends show a predominance of non-surgical interventions, such as scaling and root planing, and surgical procedures for gingival health and aesthetics. Therefore, understanding these patterns is essential for optimizing treatment planning and improving patient outcomes. Further research is needed to uncover the factors driving these demographic trends and develop more effective strategies for diverse patient populations.
AUTHORS’ CONTRIBUTION
S.A.H.: Study conception and design, data collection, analysis and interpretation of results, and manuscript preparation.
LIST OF ABBREVIATIONS
| AAP | = American Academy of Periodontology |
| EFP | = European Federation of Periodontology |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Taif University Scientific Research Ethics Committee (approval number: 45-112), Saudi Arabia.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all individual participants included in the study.
AVAILABILITY OF DATA AND MATERIALS
All data presented in this study are original and have been generated as part of this research. The data supporting the findings of the article is available in the Zenodo Repository at [https://zenodo.org/records/14865983, reference number DOI: 10.5281/zenodo.4865983
(https://doi.org/10.5281/zenodo.14865983).
FUNDING
This work was financially supported by the Deanship of Graduate Studies and Scientific Research at Taif University, Saudi Arabia.
ACKNOWLEDGEMENTS
Declared none.


