All published articles of this journal are available on ScienceDirect.
Is the Injectable Platelet-rich Fibrin (i-PRF) an Effective Method for Root Length and Alveolar Bone in Maxillary Canine Retraction? A Split-mouth Randomized Controlled Trial
Abstract
Objective
This study aimed to evaluate the effectiveness of injectable platelet-rich fibrin (i-PRF) in root resorption and alveolar bone density.
Methods
This study was a split-mouth randomized clinical trial that included 31 patients (9 males and 22 females, ages ranging from 15-25 years) treated for Class I malocclusion with the indicated extraction of the maxillary first premolar. After the first stage of the procedure, 150 gm of force was applied to the maxillary canine. Before the canine retraction, i-PRF was prepared from each patient's blood and then injected into the buccal and palatal aspects of the extraction sites. For each patient, Cone Beam Computed Tomography (CBCT) of the maxillary canine was taken before and after treatment (T1 and T4) to evaluate root resorption and bone density.
Results
A decrease in canine root length was recorded in both groups after canine retraction (p<0.001). The vertical alveolar bone increased on the buccal and lingual surfaces in both groups, and the angle of U3 to PP decreased. However, the difference was not statistically significant (p>0.05). The total alveolar bone level increased by 0.59±1.28 mm on the buccal side. These changes were statistically significant (p <0.05).
Conclusion
In this study, root resorption and alveolar bone loss were reported around the maxillary canines in both groups, i-PRF and the control. However, the difference was not statistically significant. Alveolar bone changes during orthodontic treatment were found to be small and low-risk.
Clinical Trial Registration Number
This study was registered at Clinicaltrials.gov with an identifier number: NCT06634888.
1. INTRODUCTION
Orthodontic treatment involves correcting malocclusions, enhancing dental arch aesthetics, and preserving optimal function and periodontal tissue health. It stimulates tooth movement by remodeling the periodontal ligament and alveolar bone, involving bone resorption and formation on the pressure and tension sites [1, 2].
Various factors, such as appliance type, treatment method, force direction, duration, premolar extractions, tooth distance, and root movement, influence root resorption, a common issue. Understanding these factors is crucial for managing root resorption. Accelerating tooth movement and reducing treatment duration are important for both orthodontists and patients. To ensure successful orthodontic tooth movement and stability, sufficient alveolar bone volume and root length are required. Therefore, understanding and controlling these factors is crucial for effective treatment. The use of PRF is a platelet concentrate that, when activated, releases growth factors and cytokines. These growth factors can stimulate tissue healing, angiogenesis, and cell proliferation. Prolonged orthodontic treatment increases the risk of root resorption, a negative effect on root length [3, 4]. Orthodontic acceleration in this context refers to the natural movement of teeth with a bone resorption-to-bone formation ratio of 1:1 [5]. Understanding and controlling root resorption factors is crucial. Accelerating tooth movement and reducing treatment duration is important for orthodontists and patients. Adequate alveolar bone volume and root length are essential for successful orthodontic tooth movement, and post-treatment stability prevents inflammatory processes in the periodontium [6].
Platelet based preparations from patient's blood offer a safe alternative to commercially available bioactive materials. PRF, a completely autologous fibrin matrix, was developed as a second generation platelet concentrate without anticoagulants and additives. I-PRF, obtained through low-speed centrifugation, has advantages over conventional forms, including higher rates of regenerative cells and increased growth factors during orthodontic tooth movement. Injectable platelet-rich fibrin (i-PRF) is a liquid form of PRF [7-9]. The presence of inflammatory mediators in the periodontal ligament (PDL) during orthodontic tooth movement indicates their role in the occurrence of orthodontically induced root resorption [10].
Cone beam computed tomography (CBCT) imaging provides a three-dimensional evaluation of teeth and their anatomical structures, enabling detailed visualization of teeth and surrounding structures. This allows easy detection of tooth resorption areas. CBCT imaging focuses radiation on the area of interest, encompassing all tissues in three dimensions, potentially reducing cumulative radiation exposure for patients [11-13].
However, little is known about the effects of the placement of biomaterials on the root length of the moved tooth and on the surrounding supporting bone tissue during orthodontic movement. This study aimed to evaluate and compare these effects after distalization of maxillary canines in the alveolar margin preserved with i-PRF and control alveolar in adult patients using cone beam computed tomography (CBCT).
2. MATERIALS AND METHODS
2.1. Study Participants
2.1.1. Inclusion Criteria
Patients who have completed permanent tooth replacement and were in cervical vertebral maturation stages 5 and 6 (CS5 and CS6), where cervical vertebrae 2, 3, and 4 have a concave curved lower border, and at least one of the C3 or C4 cervical vertebra is upright or at least square in shape, patients with Angle Class I malocclusion who had undergone bilateral extraction of the maxillary first premolars, patients with no missing teeth except for third molars, no previous orthodontic treatment, had good periodontal health and had the symmetric position of maxillary first premolar before retraction, and patients and/or their legal guardians for those who were under 18 years old agreed to participate in the study were included in this study.
2.1.2. Exclusion Criteria
Patients suffering from bleeding disorders, diabetes, bone diseases, periodontal disease, and cancer, as well as those using drugs, such as aspirin, heparin, warfarin, non-steroidal anti-inflammatory drugs, and glucocorticoids, which may affect the speed of tooth movement and the ability to clot and stop bleeding, were excluded. Moreover, patients with trauma and facial deformities, smokers, or pregnant were excluded from the study.
2.2. Study Design
Thirty-one subjects (9 males and 21 females) aged 15-25 years who needed bilateral maxillary canine retractions were involved in this study. This study was a randomized controlled clinical trial with a split-mouth study design with an allocation ratio of 1:1. It was a single-blind study where the statistician was blinded regarding the origin and grouping of data. It was also ensured that the coinvestigator conducting the measurements was blinded. Both the principal investigator and patients were not blinded by the procedures. The same orthodontist provided the orthodontic treatment for all participants. The right and left sides were randomly allocated to either the experimental treatments with i-PRF or the control treatment. For patients with even numbers, i-PRF was applied to the left side, and the control treatment was applied to the right side. Conversely, for patients with odd numbers, i-PRF was applied to the right side, and the control treatment was applied to the left side.
2.3. Study Procedure
Patients with bilateral Angle Class I malocclusion, who were indicated for maxillary first premolars extraction, were included in this study. Standardized intraoral and extraoral photographs of the patients, along with panoramic and cephalometric radiographs, were taken before orthodontic treatment. All the treatments were performed by the same orthodontist, and the measures were analyzed using WebCeph software (AssembleCircle Corp., Korea). To participate in the study, legal guardians for those who were under 18 years old signed a permission form after obtaining information about the objectives and methods of the study.
A split-mouth randomized controlled trial design was carried out. The i-PRF was used on the left side, and physiological saline was used on the right side of the patients with even numbers. On the other hand, the i-PRF was used on the right side for patients with an odd number, whereas physiological saline was used on the left side.
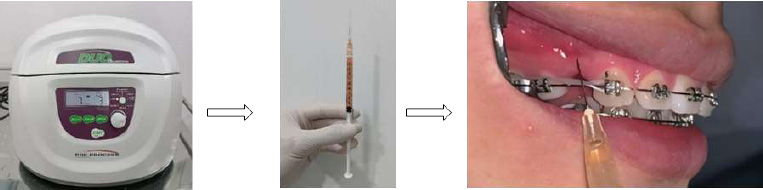
i-PRF was injected after low-speed centrifugation at 700 rpm in 3 minutes using Choukroun Duo Centrifuge (Process for PRF, Nice, France).
Before beginning the canine distalization, the optimal sliding process was performed following the leveling and alignment phase. Before retracting the canines, the upper arch was fixed with a 0.016 x 0.022 stainless steel wire (SS) (3M, USA), and a force of 150 gm was exerted using chain elastics from the brackets of the canines to the bands of the first molars. Before retraction, i-PRF injections were administered between the maxillary canine and second premolar in one quadrant, while physiological saline (0.9% sodium chloride) was injected in the contralateral quadrant. This procedure was repeated after one month.
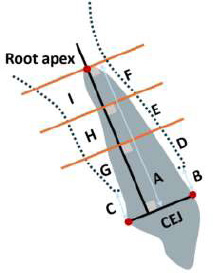
Variables were measured with CBCT in the sagittal plane. A. Root length; B and C. Vertical alveolar bone level (from CEJ to alveolar crest); D, E, and F. Cervical, middle, and apical areas of the buccal alveolar bone; G, H, and I. Cervical, middle, and apical portions of the lingual alveolar bone (Int Soc Prev Community Dent [14].
2.4. Preparation and Application of i-PRF
Venous blood was taken from each patient using 10 ml tubes (plastic tubes) without any additives or anticoagulants. This was done as fast as possible, and each tube was placed into the PRF centrifuge. The tubes were spun for 3 minutes at 700 rpm at room temperature by a Choukroun Duo Centrifuge (Process for PRF, Nice, France). The uppermost 1 mL of the blood was then collected and represented as i-PRF, and then it was injected into the mesial and distal canine tooth. Before the injection of PRF, The buccal and palatal mucosa of the extraction sites were anesthetized with a topical spray (lidocaine 8%) for pain control. Except for PRF injection, the tools, materials, and processes were the same for both groups. (Fig. 1).
2.5. CBCT Imaging and Measurements
All patients in this study underwent a cone beam computed tomography (CBCT) using an Orthophos SL 3D X-ray machine (Dentsply Sirona, USA). The times before and after canine retraction (T1 and T4) were noted. The teeth were located using axial navigation guidance from the multi-planar reconstruction (axial, sagittal, and coronal) of the CBCT following the measurements described previously (Fig. 2) [14].
Cone beam computed tomography (CBCT) was used before and four months after retraction, with imaging conducted using the Orthophos SL 3D X-ray machine (Dentsply Sirona, Charlotte, CA, USA) while adhering to As Low As Reasonably Achievable (ALARA) guidelines to minimize radiation exposure [15] (Fig. 3).
2.6. Ethics Approval
This research was approved by the ethics committee of the Can Tho University of Medicine and Pharmacy, Vietnam (approval number: 22.049.HV/PCT-HĐĐĐ). This study was registered at Clinicaltrials.gov with an identifier number: NCT06634888.
2.7. Statistical Analysis
Statistical analysis was performed using the IBM SPSS Statistics version 20, and probability values equal to or less than 0.05 were considered significant. The Shapiro–Wilk test revealed that the data were normally distributed. Paired sample t-tests and independent sample t-tests were conducted to compare the changes between groups (Fig. 4).
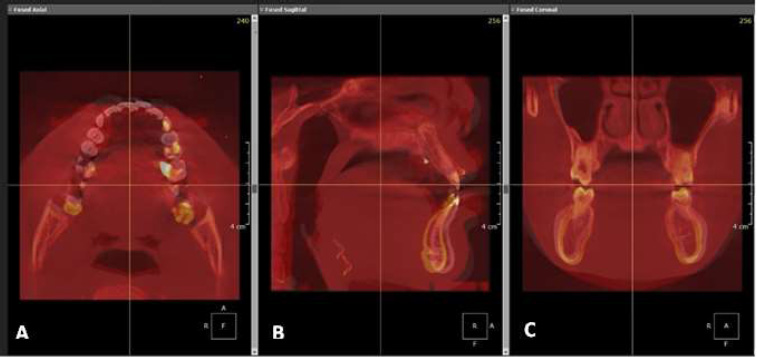
Orientation of the planes in the CBCT images. (A) Axial plane. (B) Sagittal plane. (C) Coronal plane after superimposition. Available online under the terms of the Creative Commons Attribution-Non Commercial-ShareAlike License (CC BY-NC-SA) [14].
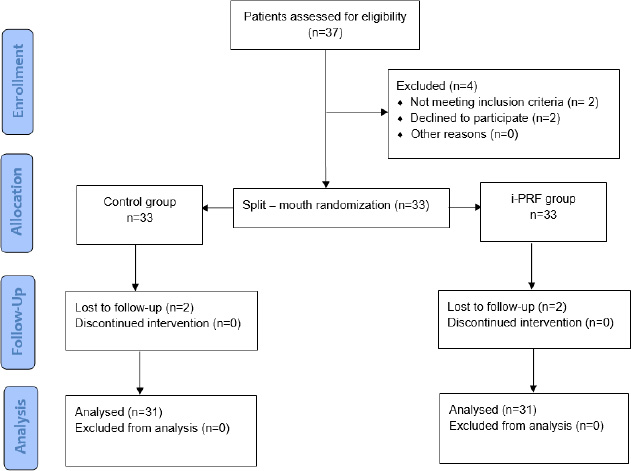
CONSORT flow diagram.
3. RESULTS
In the study on 31 patients, males accounted for 29%, and females accounted for 71% of the total population, and the mean age was 20±3.856.
The lengths of the retracted canines within each group were statistically significantly reduced at T4 compared to T1 (p<0.001). The i-PRF reduced root resorption, which was statistically significant (p<0.05) (Table 1).
A paired t-test revealed that the mean values of the alveolar bone vertically before and after the treatment in both groups were not statistically significant (p>0.05). The vertical alveolar bone increased on the buccal and lingual sides in both groups. However, the difference was not statistically significant (p>0.05), and the angle of U3 to PP decreased in both groups (Table 2).
It was found that i-PRF caused changes in the alveolar bone. The buccal crestal area increased by 0.08±0.34 mm, the middle area increased by 0.1±0.35 mm, the apical area increased by 0.49±2.13mm, and the total area increased by 0.66±2.22 mm. The lingual crestal area decreased by 0.28±1.26 mm, the middle area decreased by 0.54±1.22 mm, the apical area decreased by 1±4.93 mm, and the total area decreased by 1.82±8.41 mm. Similar to the PRF injection group, there was an increase in the buccal crestal area of 0.11±0.36 mm, middle area of 0.26±0.78 mm, apical area of 0.22±1.07 mm, and total area of 0.59±1.28 mm. The lingual crestal decreased by 0.21±1.22 mm, the middle area decreased by 0.88±5.51 mm, the apical area decreased by 1.32±4.46 mm, and the total area decreased by 2.41±1.65 mm, which was not statistically significant (p>0.05) in the control group (Table 3).
| - | T1 | T4 | p | Δ(T4-T1) | p |
|---|---|---|---|---|---|
| i-PRF group | 15.42±1.41 | 14.96±1.37 | <0.001* | -0.46±0.33 | 0.004** |
| Control group | 15.55±1.23 | 14.74±1.08 | <0.001* | -0.8±0.54 |
| - | T1 | T4 | p | Δ(T4-T1) | p | |
|---|---|---|---|---|---|---|
| Buccal alveolar bone in vertical | i-PRF group | 2.75±0.67 | 2.89±0.81 | 0.127* | 0.14±0.49 | 0.966** |
| Control group | 2.48±0.47 | 2.61±0.43 | 0.118* | 0.13±0.46 | ||
| Lingual alveolar bone in vertical | i-PRF group | 2.86±0.82 | 2.99±0.77 | 0.094* | 0.13±0.1 | 0.59** |
| Control group | 2.71±0.66 | 2.91±0.77 | 0.085* | 0.19±0.62 | ||
| The angle of U3 to PP | i-PRF group | 110.4±6.92 | 104.02±6.54 | <0.001* | 6.39±6.38 | <0.001** |
| Control group | 110.98±5.1 | 105.29±6.1 | <0.001* | 5.69±4.63 | ||
*Paired sample t-test, **Independent sample t-test.
| Alveolar Bone | Group | T1 | T4 | p | Δ(T4-T1) | p |
|---|---|---|---|---|---|---|
| Buccal | ||||||
| Crestal | i-PRF group | 1.64±0.7 | 1.72±0.65 | 0.19* | 0.08±0.34 | 0.742** |
| Control group | 1.68±0.69 | 1.79±0.67 | 0.1* | 0.11±0.36 | ||
| Middle | i-PRF group | 3.02±0.75 | 3.12±0.73 | 0.118* | 0.1±0.35 | 0.302** |
| Control group | 2.69±0.66 | 2.95±0.79 | 0.073* | 0.26±0.78 | ||
| Apical | i-PRF group | 4.97±1.94 | 5.46±2.5 | 0.215* | 0.49±2.13 | 0.533** |
| Control group | 5.01±2.35 | 5.23±2.3 | 0.273* | 0.22±1.07 | ||
| Lingual | ||||||
| Crestal | i-PRF group | 3.3±1.7 | 3.02±1.38 | 0.222* | -0.28±1.26 | 0.813** |
| Control group | 3.93±1.62 | 3.73±1.97 | 0.353* | -0.21±1.22 | ||
| Middle | i-PRF group | 17.12±6.59 | 16.59±6.89 | 0.514* | -0.54±4.52 | 0.79** |
| Control group | 17.91±5.53 | 17.04±6.73 | 0.383* | -0.88±5.51 | ||
| Apical | i-PRF group | 29.65±10.67 | 28.64±10.3 | 0.264* | -1±4.93 | 0.783** |
| Control group | 31.82±9.16 | 30.49±9.31 | 0.109* | -1.32±4.46 | ||
4. DISCUSSION
The study utilized a randomized clinical trial method, assigning participants into separate groups, with only the researchers and participants being aware of the allocation. Orthodontic treatment requires sufficient bone to prevent root resorption and alveolar bone loss. Factors affecting this procedure include root morphology, tooth agenesis, asthma, diabetes, and nail-biting habits. Mechanical factors include orthodontic forces, tooth movement type, treatment duration, and applied forces. The periodontal ligament plays a crucial role in root resorption by regulating osteoclast differentiation. Understanding these factors is essential for successful orthodontic treatment [16, 17].
Orthodontics and clinical research have reported the importance of platelet-rich fibrin due to its obvious osteogenic properties [18, 19]. Growth factors in PRF stimulate angiogenesis and impact cell proliferation and differentiation. They contain inflammation cytokines like IL-6, IL-1β, IL-1, and TNF-α and healing cytokines like IL-4 and VEGF, which have anti-inflammatory properties. PRF accelerates angiogenesis and creates fibroblasts and osteoblasts, enhancing healing. The presence of these inflammatory mediators during orthodontic tooth movement suggests their role in orthodontically induced root resorption [20, 21]. Two studies demonstrated that i-PRF was able to induce maxillary bone regeneration during sinus augmentation in a rabbit model [22, 23]. Y et al. proposed the use of PRF to minimize the resorption of hard tissues immediately post-extraction [24]. For pain control, local anesthesia (lidocaine containing adrenaline 1/100,000) was given at the target sites before the PRF injection. It is a submucosal injection rather than a subperiosteal injection. Its mechanism is similar to the injection of local anesthesia and does not follow a specific injection pattern.
The rationale behind the use of Platelet-Rich Fibrin (PRF) in orthodontic treatment, including its potential impact on root resorption, is based on its biological properties. PRF is a platelet concentrate that, when activated, releases growth factors and cytokines [25]. These growth factors can stimulate tissue healing, angiogenesis, and cell proliferation. Although it is commonly used to accelerate wound healing and tissue regeneration, its application in orthodontics has been explored for its ability to reduce inflammation, promote bone formation, and minimize side effects, such as root resorption. However, the specific mechanism by which PRF may influence root resorption, especially when injected into cortical bone, remains unclear. Applying PRF to cortical bone may limit its direct effects on the periodontal ligament, which is critical for root health, despite its potential systemic effects that indirectly influence root resorption during orthodontic treatment.
This current study suggested that orthodontic force is a contributing factor causing root resorption, which is consistent with findings from previous studies. Several studies have reported that heavy force causes more root resorption [26, 27]. The optimal orthodontic force is designed to move teeth without causing discomfort or tissue damage. Research on canine distalization suggests a maximum force of 150–200 gm on the tooth-bone interface, which maximizes tooth movement speed. Lighter forces below this level do not cause tooth movement. Root resorption is a three dimensional change in bone length occurring on the buccal-lingual and mesial-distal sides. CBCT imaging has been shown to detect root resorption with greater accuracy and less severity compared to two dimensional imaging methods. CBCT imaging provides a detailed visualization of teeth and adjacent anatomical structures, enhancing the evaluation of teeth and their surrounding structures [12]. Following the phases of leveling and alignment, we conducted CBCT scans to evaluate the alveolar bone loss around the maxillary canine, which resulted from two different retraction methods.
The findings of the present study were similar to the results of a study by Zeitounlouian et al., showing a decrease in root length in both the i-PRF and control groups [28]. Furthermore, the efficacy of i-PRF in preserving bone and preventing root resorption in orthodontic patients was similar to the one reported in another recent study by Zeitounlouian et al., which found that i-PRF was not practical in preventing canine root resorption during canine retraction. After tooth extraction, the remaining alveolar bone underwent remodeling and resorption due to the absence of the physiological stimulation typically provided by the teeth. Schropp et al. observed changes that occurred following tooth extraction in humans. They reported that the width of the alveolar ridge reduced by up to 50% during the 12-month observation period after the extraction. Horowitz et al. reported that in the first 3 months, the buccal alveolar resorption was about 56%, the lingual alveolar resorption was about 30%, and the buccal resorption was prominent and more extensive than the lingual alveolar resorption [29].
Jiang et al. reported in a clinical study that older people tend to have more root resorption [27]. The prevalence of root resorption was high, and the factors affecting it were found to be complex and multiple, including internal and external factors. Patient factors, such as genetics, age at the start of treatment, gender, nutrition, root morphology, alveolar bone density, type of malocclusion, etc., are considered internal factors. Root resorption can be caused by orthodontic treatment, but it can also be caused by factors other than orthodontics, like the type of appliance, treatment technique, continuous or intermittent force, force magnitude and direction, length of time the force is applied, premolar extractions, tooth distance, and root movement [30, 31]. However, the causes and mechanisms of resorption are not completely understood.
CONCLUSION
The root resorption and alveolar bone loss around the maxillary canines were reported in both groups, i-PRF and the control, but the difference was not statistically significant. Alveolar bone changes during orthodontic treatment were found to be small and low-risk.
AUTHOR'S CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| i-PRF | = Injectable Platelet-rich Fibrin |
| CBCT | = Cone beamcomputed tomography |
| PDL | = Periodontal ligament |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This research was approved by the ethics committee of the Can Tho University of Medicine and Pharmacy, Vietnam (approval number: 22.049.HV/PCT-HĐĐĐ). This study was registered at Clinicaltrials.gov with an identifier number NCT06634888.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article will be available from the corresponding author [L.N.L] upon reasonable request.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not for profit sectors.
ACKNOWLEDGEMENTS
The authors are grateful for the facilities and support provided by the Faculty of Odonto and Stomatology, Can Tho University of Medicine and Pharmacy.


