All published articles of this journal are available on ScienceDirect.
The Prevalence and Pattern of Oral and Maxillofacial Injuries in Al Fujairah Population, UAE- A Retrospective Study
Abstract
Background
There is inadequate documentation of Maxillofacial Injuries prevalence and patterns of occurrence in the UAE. This study aimed to explore the prevalence and trends of maxillofacial injuries among patients at Al-Fujairah Hospital, UAE, focusing on gender distribution, affected age groups, common causes, injury locations, associated soft tissue damage, diagnostic methods, and treatment approaches.
Methodology
The retrospective study was conducted at Al Fujairah Hospital, UAE, between January 2003 and February 2015 and included 716 medical records of patients (59 males and 118 females) with maxillofacial injuries. The age range was from 3 to 64 years, with a mean (SD) age of 27(6.23) years. The data included demographic details, clinical findings, radiological findings, and intervention modalities. Descriptive statistics and the Chi-square test were used to study the prevalence and trends of maxillofacial injuries.
Results
The age group 21-40 was the most affected. The age group older than 60 years old was the least affected. Oral and maxillofacial injuries were more prevalent in urban regions (n=113 (82.5%)) cases compared to rural areas (n=24(17.5%)). The majority of the victims were students. Road traffic accidents were the predominant cause of oral and maxillofacial injuries (34.5%), followed by workplace accidents (28.2%), falls (25.2%), assaults (7.7%), and others (4.1%). Among the patients, 76.4% experienced mandible or midface fractures or both. Among these, the most sustained were mandibular fractures (46.8%), followed by zygomatic complex fractures (17.0%), and 12.7% sustained mid-facial fractures. Additional fracture locations comprise nasal (27%), orbital (16%), dentoalveolar (10%), and frontal bone (7%). Of the Mandibular fractures, condylar fractures were the most common (5.4%), followed by fractures of the angle (3.8%), body (3.3%), symphysis (1.6%), and parasymphysis (1.1%). The predominant soft tissue injury was laceration, followed by contusions and incised wounds. Regarding the radiological investigations, OPGs were most commonly used for diagnosing mandibular fractures. In contrast, CT scans were commonly used to diagnose midfacial injuries, and the differences were statistically significant (p<0.05).
Conclusion
The study underscores the need for targeted preventive strategies for maxillofacial injuries, primarily caused by road traffic accidents in Al-Fujairah.
1. INTRODUCTION
Maxillofacial injuries pose a remarkable challenge to healthcare services globally due to their high rate of occurrence, mortality, and financial insinuations [1]. The World Health Organisation has stated that rapid industrial growth and population explosion in developing as well as developed countries have resulted in lifestyle modification, which in turn has led to an alarming rise in trauma rates, especially involving fractures of the maxillofacial region, owing to its specific anatomical location in the human body [2]. The maxillofacial region succumbs to maxillofacial injury, whose magnitude and causative factors diversify within the same geographical locality. This diversity is observed due to its multifactorial nature, which includes cultural, economic, social, and environmental factors [3]. These facial injuries may lead to considerable deformity or morbidity, which has serious repercussions on the individual's quality of life and productivity. The predominant causative factor for maxillofacial injuries on a global scale is road traffic accidents (RTA). In addition, falls, attacks and industrial accidents are secondary in the array of lists. Though RTAs are reported to be the leading cause of head and neck injuries in developing countries, communal or social-emotional violence contributes the same in developed countries [4].
Facial trauma can cause physical, functional, and aesthetic damage, ranging from simple injuries to complex ones involving skeletal structures [5]. Recent studies reveal a significant prevalence of oral and maxillofacial injuries, especially in severe accidents or traumatic incidents. Maxillofacial trauma cases exhibit a distinct epidemiology, characterized by more severe injuries and an increased incidence of both soft and hard tissue injuries. Facial gunshot injuries are infrequently documented yet can yield devastating outcomes [6]. Males in Sub-Saharan Africa experience a higher incidence of facial fractures than females, likely attributable to violence, falls, and societal expectations of conventional male roles [1]. Thus, periodic assessment of the etiology of maxillofacial injuries facilitates the formulation of preventive strategies.
Sports injuries mostly involve soft tissue, and the incidence of maxillofacial injuries is generally low, suggesting that sports are relatively safe for the maxillofacial complex [7]. Bite wounds are a special area of traumatology due to their high propensity for complications. Mammalian bites account for 10% of patient management, with dogs being the most common perpetrator. Human bites are more serious due to higher infection rates, with most occurring during fights and sexual assaults [8]. In addition, traumatic dental injuries constitute an unneglectable facet of maxillofacial injuries. These injuries, especially in children and young adults, account paramount public health burden [9]. Dental injuries and those of the surrounding maxillofacial region are frequent in occurrence and have been estimated to have affected around 25-30% of the permanent dentition globally, eventually causing functional disability and aesthetic concerns [10]. It has been previously demonstrated that conditions such as Class II malocclusions, Class II Skeletal sagittal pattern, and increased overjet and facial divergence are some of the significant risk factors for such injuries [11]. Moreover, individuals with orthodontic treatment needs and lower socioeconomic status have exhibited a strong positive correlation with the occurrence of traumatic dental injuries [12].
The above-mentioned estimates justify treatment priorities for maxillofacial injuries, which are utmost warranted. Therapeutic intervention must commence without delay, as airway blockage represents the most critical and urgent life-threatening consequence. Initial wound management is crucial for infection prevention. Nasal skeleton and soft tissues often require surgical repair, using autogenous grafts for primary reconstruction and secondary revision surgery. Multidisciplinary teams may also be required [13].
As the face is fundamental for every individual's unique identity, it plays a pivotal role in social reception. Thus, the targets of such injuries are affected psycho-socially and aesthetically, which, in turn, leave a considerable impact on communal relationships, employment prospects, and societal integrity. This further underscores the necessity to regularly verify the frequency and patterns of maxillofacial injuries [14, 15]. The study's findings are intended to address this ceaseless issue, which may aid in deploying preventive strategies to abate the incidence and ensuing morbidities caused by maxillofacial injuries.
There exists evidence in the literature regarding the epidemiological characteristics of maxillofacial trauma. However, there is limited data regarding this from the state of Al Fujairah, UAE. Therefore, the study aimed to explore the prevalence and trends of maxillofacial injuries among patients at Al-Fujairah Hospital, UAE, focusing on gender distribution, affected age groups, common causes, injury locations, associated soft tissue damage, diagnostic methods, and treatment approaches.
2. MATERIAL AND METHODS
The Research Ethical Committee of the Hamdan Bin Mohammed College of Dental Medicine (HBMCDM) and the Ethical Committee of the Ministry of Health and Prevention (MOHAP) approved the undertaking of this study.
This retrospective, descriptive hospital-based study was carried out at Al Fujairah Hospital, UAE, within the Oral and Maxillofacial Surgery and Emergency Medicine departments. Data was collected from January 2003 to February 2015, including archival access. Al Fujairah Hospital is the largest referral hospital in the region and serves as the sole referral centre for all complex oral and maxillofacial injuries in the state. Therefore, the sample derived from the hospital database is considered to be a true representation of the entire state's cases. The study assessed complete patient records from individuals who sought treatment for oral and maxillofacial injuries in these two departments.
2.1. Selection Criteria and Variables Recorded
2.1.1. Study Sample
This study enrolled 716 patient records with oral and maxillofacial injuries and followed a strict selection criterion. Inclusion criteria: 1. All patient records presented to the two departments with oral and maxillofacial injuries; 2. Records accompanied by radiological reports; and 3. Records of patients residing only in Al Fujairah, UAE. Exclusion criteria: 1. Records with incomplete patient information; 2. Patients who refuse to get treated; and 3. Patients who were previously treated in other hospitals. The data was retrieved from hospital databases using private online and offline resources to gather information on the patient's social-demographic information, chief complaint, injury location, cause, and condition.
A structured form was employed to gather data regarding patients' socio-demographic information, patient’s chief complaint, the area at which the injury occurred, etiology of the injury, the overall condition of the patient immediately post-injury and after that, and the duration from injury to hospital presentation.
Clinical findings were recorded, including the type and site of injuries, including those of the soft tissue and hard tissue. The recorded soft tissue injuries were contusions, abrasions, lacerations, avulsions, cut wounds, and bruises. Hard tissue injury was characterized as a fracture of the facial bones, encompassing the nasal bone, maxilla, mandible, zygoma, frontal, palatal, and orbital bones. Injuries related to the temporomandibular joint were also recorded.
Radiological assessments were orthopantomography (OPG) and computed tomography (CT). The patient records indicated that interventions included essential resuscitation measures such as airway management, breathing monitoring, bleeding control, medication administration, and surgical procedures. Additionally, complications such as wound infections, osteomyelitis, and malunion were documented. Furthermore, the duration of hospital admission was noted in relation to the type of injury and the treatment provided.
2.2. Statistical Analysis
The collected data were entered into a Microsoft Excel spreadsheet and were subjected to statistical analysis by using Statistical Package for Social Sciences program (SPSS) Version 20 IBM, USA. Descriptive statistics were performed to check the distribution of the population based on age, gender, and prevalence of maxillofacial injuries. The association between the study subjects and study parameters was checked by using Chi-square test with a significance level, p-value≤ 0.05 as statistically significant.
3. RESULTS
3.1. Socio-demographic Pattern
The study comprised a total of 716 patient records with oral and maxillofacial injuries, out of which 579 (83.5%) were males, while 118 (16.5%) were females, with a Male Female ratio of 5:1. The age range was 3 to 64 years with a mean age of 27.0± 6.23 years and a median age of 29 years. The age group of 21-40 was the most affected. The age group of >60 was the least affected. Oral and maxillofacial injuries were more prevalent in urban regions, with 113 cases (82.5%), compared to rural areas, which reported 24 cases (17.5%) in this group. The majority of the victims were students.
3.2. Causes of Injury and the Victims Involved
Road traffic accidents (RTA) were the predominant cause of oral and maxillofacial injuries, accounting for 34.5%, particularly among UAE citizens. Other notable causes included workplace accidents (28.3%) and falls (25.2%), while assaults accounted for 7.7% of the cases. For the injuries caused by road traffic accidents (RTA) among both the UAE nationals and expatriate groups, it was noted that UAE national car drivers were at higher risk of sustaining facial injuries compared with expatriate drivers, with a statistically significant difference between the two groups (p<0.05) (Table 1). Motorcycle accidents were the least cause of injury among UAE national and expatriate populations (17.6% vs. 2.7%, respectively) (Table 1).
Comparison of RTA patterns before and after March 2008 showed a significantly high incidence before March 2008, comprising 62.6% compared to 24% post-2008 (p <0.001). The driver's origin significantly impacted the likelihood of a car accident. In addition, it was noted that the proportion of accidents involving UAE national drivers and motorcyclists was significantly higher than those involving expatriate drivers (p<0.001) and moto cyclists (p<0.06). There were no significant differences between the UAE nationals and expatriate drivers with respect to car passengers and pedestrians.
3.3. Pattern of Site-specificity
Table 2 shows the distribution of trauma by site among 716 patients treated for oral and maxillofacial fractures at Fujairah Hospital from 2003 to 2015. Among the 716 patients, 548 (76.4%) experienced mandible or midface fractures or both. Among these, the most sustained mandibular fractures were 335 (46.8%), followed by zygomatic complex fractures, numbering 122 (17.0%). Nineteen individuals (12.7%) sustained mid-facial fractures. Additional fracture locations comprise nasal (27%), orbital (16%), dentoalveolar (10%), frontal (7%), and soft tissue (5%) (Fig. 1). The associated soft tissue injuries comprised lacerations, followed by bruises and cut wounds. Of the Mandibular fractures, condylar fractures were the most common (5.4%), followed by fractures of the angle (3.8%) and body (3.3%), while the symphysis (1.6%) and parasymphysis (1.1%) represented the least. In addition, the predominant soft tissue injury was laceration, followed by contusions and incised wounds.
3.4. Diagnostic Imaging Methods Employed
Regarding the radiological investigations (Table 3), OPGs were most commonly used for diagnosing mandibular fractures. In contrast, CT scans were widely used to diagnose midfacial injuries, and the differences were statistically significant.
| Victims of Trauma | Origin | No | Yes | Total | Chi-square | p-value |
|---|---|---|---|---|---|---|
| Car driver | UAE | 77(71.3%) | 31(28.7%) | 108(59.3%) | 299.6 | <0.001* |
| Expatriate | 69(93.2%) | 5 (6.8%) | 74 (40.7) | |||
| TOTAL | 146(80.2%) | 36(19.8%) | 182 (100%) | |||
| Car passenger | UAE | 105(97.2%) | 3 (2.8%) | 108(59.3%) | 163.4 | 0.673 |
| Expatriate | 72 (97.3%) | 2 (2.7%) | 74 (40.7%) | |||
| TOTAL | 177(97.2%) | 5 (2.8%) | 182 (100%) | |||
| Pedestrian | UAE | 108(59.7%) | 0 | 108(59.3%) | 163.5 | 0.407 |
| Expatriate | 73 (98.6%) | 1 (1.4%) | 74(40.7%) | |||
| TOTAL | 181(99.4%) | 1(0.6%) | 182 (100%) | |||
| Motor Cyclist | UAE | 89(82.45%) | 19(17.6%) | 98(54%) | 177.8 | 0.006* |
| Expatriate | 72 (97.3%) | 2 (2.7%) | 74(40%) | |||
| TOTAL | 161(88.4%) | 21(11.6%) | 182(100%) |
| Parameter |
Frequency N |
Percentage % |
|---|---|---|
| Etiology | ||
| Car driver | 140 | 19.6 |
| Car passenger | 24 | 3.3 |
| Pedestrian | 4 | 0.5 |
| Assault | 55 | 7.7 |
| Motorcyclist | 82 | 11.4 |
| Fall | 180 | 25.2 |
| Industrial | 202 | 28.2 |
| Others | 29 | 4.1 |
| Specific sites of injury | ||
| Maxilla | 91 | 12.7 |
| Mandible | 335 | 46.8 |
| Zygomatic arch | 122 | 17 |
| Others | 168 | 23.5 |
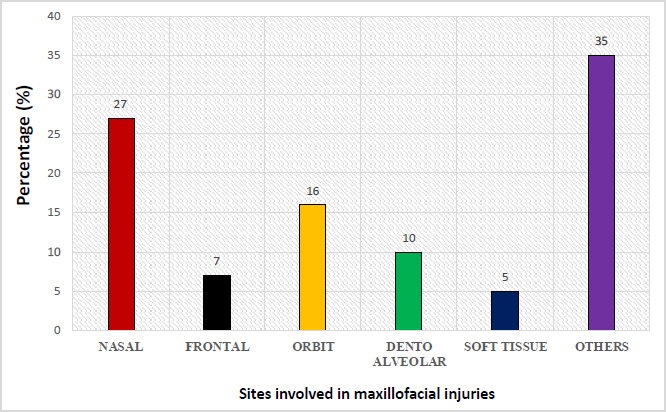
Prevalence of specific sites of the skull involved in maxillofacial injuries.
| Radiological Investigation | Facial Injuries | Mandibular Injuries | Total Cases | Chi-square | p-value |
|---|---|---|---|---|---|
| OPG | 112 (30.6%) | 253 (69.4%) | 365 (58%) | 533.8 | < 0.001 |
| CT-Scan | 235 (88.6%) | 30 (11.4%) | 265 (42%) | ||
| TOTAL | 347 (55%) | 283 (45%) | 630 (100%) |
| Parameter |
Frequency N |
Percentage % |
|---|---|---|
| Treatment options | ||
| ORIF | 324 | 45.3 |
| Wiring | 350 | 48.9 |
| Suturing | 6 | 0.8 |
| Surgery | 22 | 3.1 |
| Medication | 2 | 0.2 |
| Treatment referral | 13 | 1.7 |
3.5. Treatment Modalities Implemented
The surgeons used several treatment modalities for the reduction and fixation of facial fractures. Most facial fractures were treated by open reduction and internal fixation (ORIF), constituting 48.95, and 45.3% were treated using intermaxillary or mandibular-maxillary fixation (Table 4). Surgical debridement and wound suturing were also used to treat soft tissue injuries.
4. DISCUSSION
The Fujairah emirate, the fifth-largest state in the UAE, has limited studies on documentation of facial injuries. With the causes varying globally and factors like climate, social trends, and population influencing the prevalence, there is a dire necessity for periodic ratification of the characteristics of such injuries. This will, in turn, pave the way for healthcare service providers and policymakers to implement strategies for preventing and managing such crucial injuries by amending the existing system of policies and healthcare facilities. The current study indicated that men experienced a greater incidence of maxillofacial injuries than women, with a male-to-female ratio of 5:1. This finding is similar to several previous reports [1]. This high frequency in men could be generally attributed to their involvement in high-risk activities such as construction, driving, and sports.
Conversely, women in the UAE predominantly engage in less hazardous social tasks, leading to a reduced frequency of injuries. However, the current study results indicate that road traffic accidents (RTA) are the most common cause of injury, accounting for 34.4% of all facial skeletal and soft tissue injuries. A previous study by Agnihotri et al., who assessed the pattern of maxillofacial injuries, demonstrated that road traffic accidents are the leading cause of facial trauma, and this could be attributed to the victims’ negligence of safety measures like usage of seatbelts or helmets and violation of traffic rules such as speeding [16]. Other studies also corroborate our findings, stating that RTAs are the leading cause of such traumatic injuries [17]. The rise in RTA in the UAE is due to the gradual increase in motor vehicles and motorcycles, which are more attractive and cheaper than commercial taxis. However, most motorcyclists are owned by youth, who often take risks and do not abide by traffic rules [18].
The predominant age group impacted is 21-40 years, perhaps indicative of increased physical activity and self-mobility. Numerous studies have indicated that the majority of injury victims were predominantly males aged between 20 and 40 years [16, 19, 20].
It was further reported that household and schoolyard accidents are major contributors to facial injuries in children and adolescents, as these environments often present various trauma risks [21, 22]. Such injuries typically occur through mechanisms like falls, collisions, or impacts with objects. In households, furniture and stairs are common hazards, especially for younger children, with falls being the leading cause of facial fractures. Additionally, accidental contact with sharp kitchen tools or hot surfaces can cause facial lacerations or burns. Toys with sharp edges or improper use pose another risk, particularly for toddlers with underdeveloped motor skills. In school settings, physical activities, especially contact sports like football and basketball, are prominent causes of facial injuries [23, 24].
The study found that mandibular fractures were more common in patients with facial trauma compared to mid-facial fractures. Due to its prominent anatomic location in the facial region, the mandible renders it more vulnerable to fracture. The high incidence of mandibular fracture has also been reported by several previous studies, constituting the same reason [20, 25]. The management of facial soft tissue injuries is a substantial component of the responsibilities of oral and maxillofacial surgeons. Lacerations were identified as the most common type of soft tissue injury, which agrees with previous studies, which reported lacerations and abrasions as the most prevalent [25]. A study by Gassener et al. reported that soft tissue injuries commonly involve the lips extraorally, the gingiva, the buccal mucosa, and the tongue intraorally [26].
The treatment rendered to patients mainly involved open reduction and internal fixation, with intermaxillary fixation being regarded as the principal mode of treatment. Previous studies have also considered this treatment modality the most commonly utilized one. Any difference in the treatment provided may be attributed to the site and severity of the injuries and the hospital policies [27, 28]. The results indicate the necessity for specific interventions and improved treatment regimens for maxillofacial fractures. Future research should investigate the underlying causes, develop awareness campaigns, and conduct longitudinal studies.
4.1. Clinical Implications
Clinically, the study emphasizes the importance of timely and effective management of maxillofacial injuries, with open reduction and internal fixation (ORIF) as a preferred treatment modality. The insights provided are particularly relevant to oral and maxillofacial surgeons, emergency healthcare providers, and public health policymakers, offering actionable data to guide both preventive strategies and therapeutic approaches.
Furthermore, the results underscore the necessity of establishing regional trauma centers equipped with multidisciplinary teams for efficient management and rehabilitation of maxillofacial trauma cases. This study contributes to the growing body of evidence aimed at improving outcomes and guiding preventive policies in the field of maxillofacial trauma care.
CONCLUSION
This retrospective study highlights the prevalence, etiology, and patterns of maxillofacial injuries in the Al-Fujairah population. Road traffic accidents emerged as the leading cause of these injuries, predominantly affecting young adult males, with mandibular fractures being the most common type. The findings underscore the need for targeted preventive measures, such as public awareness campaigns, stricter enforcement of road safety regulations, and improved use of protective devices like seatbelts and helmets.
AUTHORS’ CONTRIBUTION
M.A.J., A.M., A.H.: Study conception and design; A.H., A.S., S.A.: Data collection; M.A.J., A.M., D.A.: Analysis and interpretation of results; A.M., S.A.K., M.A.J., D.A., P.K.Y.: Draft the manuscript. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| SPSS | = Statistical Package for Social Sciences program |
| OPG | = Orthopantomography |
| CT | = Computed tomography |
| RTA | = Road traffic accidents |
| ORIF | = Open reduction and internal fixation |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Research Ethical Committee of the Hamdan Bin Mohammed College of Dental Medicine (HBMCDM) and the Ethical Committee of Ministry of Health and Prevention (MOHAP), UAE approved the undertaking of this study (MOHAP/DXB/SUBC/NO-6/2016).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
ACKNOWLEDGEMENTS
We would like to acknowledge the Ministry of Health, UAE, for their immense help and valuable guidance in carrying out this study.
DISCLOSURE
“The pattern of oral and maxillofacial injuries among patients attending Fujairah Hospital, Fujairah, UAE.”
Available at: https://repository.mbru.ac.ae/entities/publication/7ec1e346-93d4-4e2a-8fe7-d4db223b2b78


