All published articles of this journal are available on ScienceDirect.
Prevalence of Root Canal Treatment for First Permanent Molars among Children:A Cross-sectional Study
Abstract
Objective
The First Permanent Molar (FPM) is the tooth most susceptible to caries. Various treatment modalities are available for the management of deep carious lesions, with root canal therapy (RCT). However, the literature is lacking data regarding the prevalence of RCT in FPM. This study aimed to determine the prevalence of RCT in FPM among children aged 9-18 years in Jeddah, Saudi Arabia.
Methods
Children aged 9-18 years who underwent RCT in three major treatment centers in Jeddah, Saudi Arabia, between September, 2010 and June, 2019, were included in the study. A data collection form was developed to extract information from the electronic records of the patients, including demographic data and details related to the root canal-treated teeth.
Results
The prevalence of RCT in FPM was 3% (811/27,414) with a mean age of 14.00±2.36. The male-to- female ratio was 1:1.74. Mandibular FPM was more frequently treated with RCT compared to the maxillary FPM, and the most commonly treated teeth were lower-left FPM (36.3%). The majority of patients (79.3%) had one treated FPM.
Conclusion
This study provides baseline data on RCT prevalence in FPMs among children in Jeddah, Saudi Arabia. The findings highlight a prevalence rate of 3%, suggesting an early onset of dental disease during childhood.
1. INTRODUCTION
The First Permanent Molar (FPM) is the most vulnerable tooth to dental caries in permanent dentition, primarily due to its early eruption in the oral cavity around the age of six [1-4]. Among young patients, FPM has a high caries rate [3]. In Saudi Arabia, it was reported that the prevalence of dental caries in FPM among school children ranged from 68 to 70% [5]. In China, the prevalence of decayed, missing, filled teeth (DMFT) in FPM was found to be 41% [6]. A study was conducted in the United Kingdom and revealed that 45% of FPMs were extracted in Manchester and 48% in Sheffield, and the major cause (70%) of extraction was dental caries with no meaningful prognosis [1].
Management of dental caries can be achieved using simple restorations [2, 3]. However, in some cases, this cannot be achieved due to the extent of the decay, leaving a weak remaining dental structure [2], or the dental caries are too deep, reaching the pulp [3]. Different modalities are available for managing deep carious lesions reaching the pulp. In the case of immature roots, treatment options include pulpotomy [7], revascularization technique [8], and apexification [8]. Root Canal Therapy (RCT) can be performed as a last resort for immature roots and as the treatment of choice for mature roots [7].
The prevalence of RCT in FPM was assessed in the literature. Ridell et al. found that among adolescents and young adults, 60% of endodontically treated teeth were FPMs [9]. Lilly et al. found that among a group of dentists, molars represented 26.7% of all teeth treated with RCT [10]. Serene and Spolsky evaluated the frequency of RCT at the University of California, Los Angeles. They reported that mandibular FPMs were the most commonly treated teeth, representing 18.1%, while maxillary FPMs were the second most commonly treated teeth (10.8%) of all RCT-treated teeth [11]. In Saudi Arabia, a study done in Abha to assess the incidence of RCT reported that the incidence of RCT performed on FPM was 1.2% [12]. To date, the literature lacks enough data about the prevalence of RCT performed in FPM in children. Identifying the prevalence of this type of intervention is essential for strategic healthcare planning and enhancing clinical preparedness. Prevalence studies provide crucial data that inform resource allocation and help tailor healthcare services to meet specific community needs effectively. Additionally, these insights are invaluable for designing educational programs aimed at equipping healthcare practitioners with the knowledge and training required to deliver comprehensive dental care to pediatric patients. By understanding prevalence rates, healthcare systems can better anticipate demand, address gaps in service, and improve patient outcomes [13].
Therefore, this study aims to determine the prevalence of RCT among children aged 9-18 years in 3 main treatment centers in Jeddah, Saudi Arabia.
2. MATERIALS AND METHODS
This cross-sectional study was conducted at three major treatment centers in Jeddah, Saudi Arabia. The centers were King Abdulaziz University Dental Hospital (KAUDH), King Fahad Armed Forces Hospital (KFAFH), and King Abdulaziz Medical City (KAMC). Ethical approvals were obtained from the Research Ethics Committee of KAUFD (172-11-19, 005-01-19), the Research Ethics Committee of KFAFH (REC 470), and the Institutional Review Board of the Ministry of National Guard at King Abdullah International Medical Research Center (KAIMRC) (SP20/426/J). Consent to participate was acquired from the participants’ parents and/or guardians prior to their inclusion in the study.
The study included healthy patients (ASA I) aged 9 to 18 years who underwent RCT in their FPMs between September 1st, 2010, and June 30th, 2019. Patients with medical conditions, younger than 9 years or older than 18 years, or who underwent any endodontic treatment other than full pulpectomy (such as pulpotomy, apexogenesis, apexification) were excluded. All patients fitting the inclusion criteria were included in the study. Hence, sample size calculation was not required.
The electronic filing systems in the aforementioned centers were used to identify the list of all patients aged from 9 to 18 years who attended the dental clinics during the period between the 1st of September, 2010 and the 30th of June, 2019. Then, the list was filtered to identify those who underwent RCT in their FPMs. A data collection form was assembled to record the information from the patients' electronic files. The first part of the form included questions regarding the patients’ demographic data, including age, gender, and nationality. The second part of the data collection form included a record of the number and code of the RCT-treated teeth.
2.1. Ascertainment of Exposure
After the electronic filing was screened for patients receiving RCT during their childhood, the faculty and residents of the endodontic and pediatric departments were contacted, and their patients’ lists were screened to ensure that their patients were included in the electronic hospital list. Moreover, we contacted 405 (50%) and examined 201 (25%) patients mentioned in the electronic hospital list and ensured their exposure to RCT.
3. RESULTS
The total number of patients who visited the three above-mentioned treatment centers from the 1st of September, 2010, until the 30th of June, 2019, with the age range from 9 to 18 years, was found to be 27,414, of which 16,703 were from KAUDH, 5530 from KFAFH, and 5181 from KAMC.
The list was then filtered in order to identify the patients who underwent RCT. The number of patients who had RCT in their FPMs was 945, at which 273/945 (28.9%) were from UDH, 320/945 (33.9%) were from KFAFH and 352/945 (37.2%) were from KAMC. The electronic files for those patients were reviewed according to the inclusion criteria. One hundred and thirty-four patients were excluded from the three centers, either because they had a medical condition or because they had other forms of pulp treatment techniques. Hence, the total number of patients who had RCT in their FPMs was 811 (Fig. 1). Accordingly, the prevalence of RCT performed on FPM among children of 9-18 years was 3% in the selected treatment centers (Table 1).
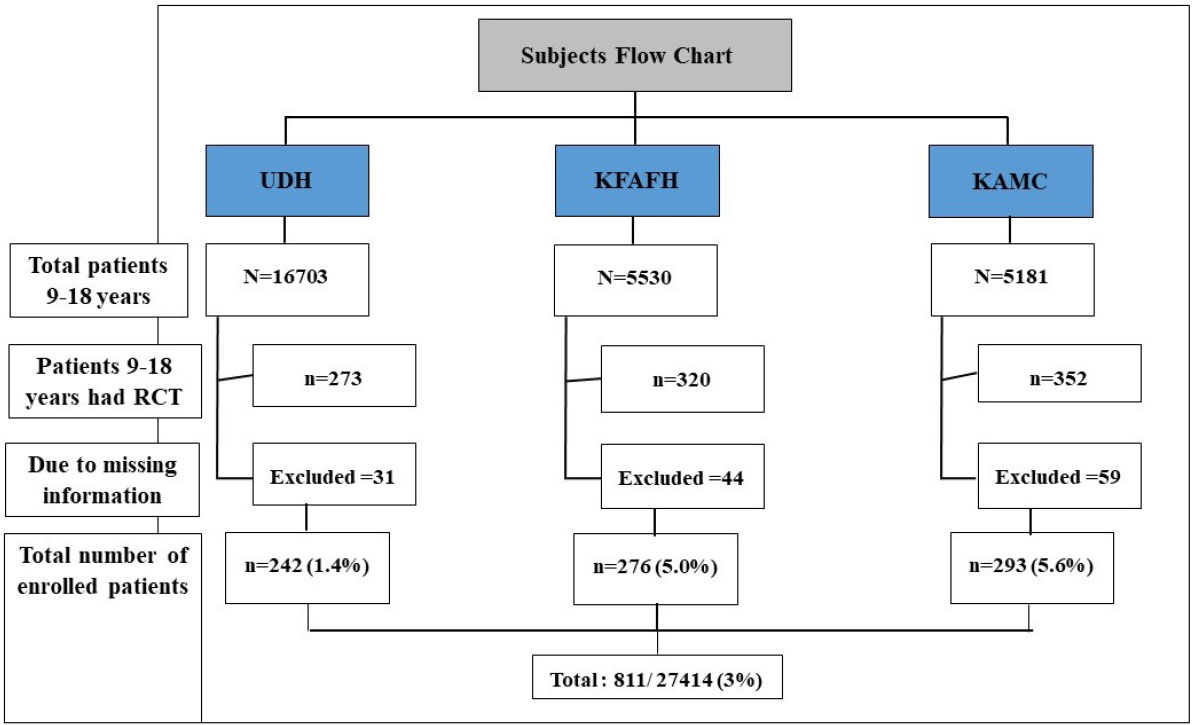
Flow chart of patients (aged 9 to 18 years) who underwent root canal therapy between September 1st, 2010, and June 30th, 2019.
Note:
UDH: University Dental Hospital, KFAFH: King Fahad Armed Forces Hospital, KAMC: King Abdulaziz Medical Center, RCT: Root Canal Treatment.
| Center | Total Number of Patients | Number of Excluded Patients$ | Number of Patients with RCT | RCT Prevalence |
|---|---|---|---|---|
| KAUDH | 16,703 | 31 | 242 | 1.4% |
| KFAFH | 5,530 | 44 | 276 | 5% |
| KAMC | 5,181 | 59 | 293 | 5.6% |
| Total | 27,414 | 134 | 811 | 3% |
Out of 811 patients, males represented 36.5% (n=296), and females represented 63.9% (n=515), with a ratio of 1:1.74. This difference between the number of male and female patients treated in the three treatment centers was not statistically significant (P=0.287). However, there was a significant difference between the mean age of children treated with RCT in the three centers, with younger age in KAUH (13.51±2.32 years) and the mean total age of 14.00±2.36 (Table 2).
Regarding the number of root canal-treated FPM per patient, 79.3% (n=643) of the patients had one RC-treated FPM, 17.1% (n=139) of the patients had two RC-treated FPM, 3.1% (n=25) had three RC-treated FPM, and 0.5% (n=4) had four RC-treated FPM. The difference in the number of RCT-treated FPM per patient among the three centers was statistically significant (p <0.001), as mentioned in Table 2.
The total number of FPM treated with RCT was 1011 teeth. Treatments done in the maxillary arch were found to make up 32.6% (n=330), while in the mandibular arch, it was 67.4% (n=681), and the difference was statistically significant (P-value 0.004). The percentages of RCTs done categorized by tooth code number are as follows: 15.1% (n=153) for tooth number 16, 17.5% (n=177) for tooth number 26, 36.3% (n=367) for tooth number 36, and 31.1% (n=314) for tooth number 46. The difference between the total number of treated teeth when considering the tooth code number among the three centers was statistically significant, with a p-value of 0.031, as reported in Table 3.
| Variable | Healthcare Center |
Total n (%) |
p-value | |||
|---|---|---|---|---|---|---|
|
KAUDH n (%) |
KFAFH n (%) |
KAMC n (%) |
||||
| Age | Mean ±SD | 13.51±2.32 | 14.48±2.33 | 14.10±2.40 | 14.00±2.36 | 0.001* |
| Gender | Males | 98 (40.5) | 98 (35.5) | 100 (34.1) | 296 (36.5) | 0.287 |
| Females | 144 (59.5) | 178 (64.5) | 193 (65.9) | 515 (63.9) | ||
| Nationality | Saudi | 107 (44.2) | 276 (100) | 293 (100) | 676 (83.4) | <0.001* |
| Non-Saudi | 135 (55.8) | 0 | 0 | 135 (16.6) | ||
| No. of RC treated teeth per patient | One | 188 (77.7) | 195 (70.7) | 260 (88.7) | 643 (79.3) | <0.001* |
| Two | 45 (18.6) | 67 (24.3) | 27 (9.2) | 139 (17.1) | ||
| Three | 8 (3.3) | 12 (4.3) | 5 (1.7) | 25 (3.1) | ||
| Four | 1 (0.4) | 2 (0.7) | 1 (0.3) | 4 (0.5) | ||
| Total | 242 (100) | 276 (100) | 293 (100) | 811 (100) | - | |
| Variable | Healthcare Center | Total n (%) | p-value | ||||
|---|---|---|---|---|---|---|---|
|
KAUDH n (%) |
KFAFH n (%) |
KAMC n (%) |
- | ||||
| Location | Maxillary molars (16,26) | 77 (25.2) | 135 (36.3) | 118 (35.4) | 330 (32.6) | 0.004* | |
| Mandibular molars (36,46) | 229 (74.8) | 237 (63.7) | 215 (64.6) | 681 (67.4) | |||
| Tooth code number | Upper right permanent molar (16) | 36 (11.8) | 57 (15.3) | 60 (18) | 153 (15.1) | 0.031* | |
| Upper left permanent molar (26) | 41 (13.4) | 78 (21) | 58 (17.4) | 177 (17.5) | |||
| Lower left permanent molar (36) | 123 (40.2) | 132 (35.5) | 112 (33.6) | 367 (36.3) | |||
| Lower right permanent molar (46) | 106 (34.6) | 105 (28.2) | 103 (30.9) | 314 (31.1) | |||
| Total | 306 (30.3) | 372 (36.8) | 333 (33) | 1011 (100) | - | ||
4. DISCUSSION
This study aimed to determine the prevalence of RCT among children aged 9 to 18 years across three major treatment centers in Jeddah, Saudi Arabia. Studying the prevalence and distribution of RCT is of prime importance, as it informs the need for this type of treatment and helps in the planning and allocation of healthcare resources. Moreover, it also enables comparisons with other populations and monitors changes in prevalence trends over time [14, 15]. Due to the limited information available regarding the prevalence of RCT in FPMs among children, a cross-sectional study design was used to provide baseline data for future prospective studies.
The study was conducted in Jeddah, Saudi Arabia, the country's second-largest city, and is known for its diverse population [16]. The research was carried out at three main treatment centers, namely, KAUDH, KFAFH, and KAMC. These centers were selected because they are considered referral centers for specialized treatments with a high patient flow and volume. Additionally, KAUDH serves a heterogeneous population, while KFAFH and KAMC primarily cater to military families. Furthermore, these centers are geographically distributed across different regions of Jeddah, with KFAFH in the north, KAMC in the south, and KAUDH centrally located [17]. These characteristics aid in the generalizability of the data and help reduce selection bias.
The prevalence of RCT in FPMs among children in this study was found to be 3%. By comparison, in adults, a systematic review that included 72 studies reported a prevalence of 55.7% among them [18]. On the other hand, few studies have assessed the prevalence of RCT among children. A study conducted in the USA reported a 6.7% prevalence of RCT among pediatric patients relative to the total RCTs performed across all age groups, including adults. Furthermore, the study was limited to a single university hospital and only involved patients from endodontic clinics, thereby introducing potential selection and information bias [19], which consequently caused selection and information bias. Another study in Sweden reviewed the radiographs of all 19-year-old patients and found a 9.1% prevalence of endodontically treated teeth [20]. While some of these RCTs might have been performed during childhood, others could have been conducted during early adulthood. Consequently, our study provides original and valuable data for future research.
A prevalence of 3% could be considered significant, given that the failure rate of RCTs has been reported at 21% after a mean follow-up period of 5.54 ± 2.92 years [21, 22]. Furthermore, caries was found to be the primary reason for RCT in all prior studies [20], which is a preventable disease. These study findings urge public health services and community health care providers to exert more effort in early caries prevention.
Additionally, this study found that more than half (63.9%) of the treated patients were females, which was aligned with the findings of a study by Ng et al., which reported that 58% of root canal treatments were performed on female patients [23]. These findings might be due to the slight predominance of females in the study sample, which could reflect the gender-based differences in health-seeking behavior and increased awareness of females to seek healthcare [23].
The mean age of children receiving RCT on the FPM was 14 years, which is older than the mean age reported in a Turkish study (11 years) [24]. This age difference may be attributable to the Turkish study's data collection from pediatric departments, which might not include all patients up to 18 years old.
In this study, mandibular FPMs were the most commonly treated, likely due to their higher caries rate compared to maxillary FPMs, which may be attributed to their earlier eruption timing, anatomical structure, and location, making them prone to food entrapment and susceptible to caries formation. Mimoza and Vito also found that mandibular FPMs have a higher prevalence of caries than maxillary FPMs [25]. Additionally, Chen et al. confirmed this by reporting a higher caries prevalence in mandibular molars compared to maxillary molars [26].
The strengths of this study include its use of data from three main treatment centers, thus reflecting the diverse population of Jeddah. It also provides valuable insights and information that is needed for future research and community services which was not previously reported. As for the study limitations, the primary expected limitation of such a prevalence study that relies on hospital records is the ascertainment of exposure. To mitigate this limitation, we contacted and examined patients from the electronic hospital list. In addition, we checked the list of the departments via their treatment providers.
This study underscores the importance of enhanced preventive strategies and early interventions so as to reduce the need for RCT in children. Future research should aim to expand these findings by incorporating more diverse healthcare settings and employing prospective study designs in order to gain a comprehensive understanding of RCT prevalence trends and their underlying determinants. These efforts will contribute to better planning and allocation of dental health resources and ultimately improve pediatric oral health outcomes.
CONCLUSION
This study provides critical baseline data on the prevalence of RCT in FPMs among children in Jeddah, Saudi Arabia. The findings highlight a prevalence rate of 3%, which suggests a notable burden of endodontic treatment in children.
AUTHORS’ CONTRIBUTION
N.O.B., W.D., and H.J.S.: Contributed to the conceptualization; N.O.B., W.D., M.I.A., J.T., and H.J.S.: Proposed the methodology; W.D., M.I.A., J.T., and H.J.S.: Collected the data; W.D. and H.J.S.: Took part in data analysis and interpretation; N.O.B., W.D., and H.J.S.: Participated in project administration; N.O.B., W.D., and H.J.S.: Carried out the supervision; N.O.B. and W.D.: Wrote the original draft; N.O.B., W.D., and H.J.S.: were involved in writing and editing the final draft.
LIST OF ABBREVIATIONS
| FPM | = First permanent molar |
| RCT | = Root canal therapy |
| DMFT | = Decayed missing, filled teeth |
| KAUDH | = King Abdulaziz University Dental Hospital |
| KFAFH | = King Abdulaziz Medical City |
| KAMC | = King Abdulaziz Medical City |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approvals were obtained from the Research Ethics Committee of KAUFD King Abdulaziz University Faculty of Dentistry (172-11-19, 005-01-19), Research Ethics Committee of KFAFH King Fahad Armed Forces Hospital (REC 470), and the Institutional Review Board of the Ministry of National Guard at KAIMRC King Abdullah International Medical Research Center, Saudi Arabia (SP20/426/J).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Consent to participate was acquired from the participants’ parents and/or guardians prior to them being included in the study.


