All published articles of this journal are available on ScienceDirect.
Bone Block Protection using Dense Polytetrafluoroethylene Membranes in Vertical Bone Augmentation Procedures for Atrophic Maxilla: A Case Report
Abstract
Background
Large vertical bone defects in the posterior maxilla pose a significant challenge for oral and maxillofacial surgeons aiming to rehabilitate the region with dental implants. Autogenous bone grafts remain the gold standard for bone grafting due to their trifecta of osteogenesis, osteoinduction, and osteoconduction properties. Autogenous bone blocks harvested from the anterior iliac crest are a predictable and extensively researched treatment approach for the management of localized or generalized alveolar ridge defects. The primary complications associated with reconstructing atrophic alveolar bone are wound dehiscence and subsequent exposure of the bone graft material to the oral environment, a challenge that may be unavoidable in certain cases.
Case Presentation
In this case report, we present the reconstruction of the posterior maxilla in a 30-year-old patient, utilizing an autologous bone graft harvested from the anterior iliac crest. The bone block was then shielded with a dense polytetrafluoroethylene membrane. The bone block was fixed using tenting screws, and the membrane was attached to the tent screws with special screws (tenting cap screws). Membrane exposure occurred two weeks post-surgery, and the membrane was easily removed four weeks after the procedure. There were no signs of infection or loss of bone graft material during this timeframe.
Conclusion
Applying d-PTFE to cover the bone block in extensive posterior maxillary vertical augmentation procedures effectively shields the bone block from bacterial contamination, lowers the likelihood of complications, and enhances the predictability of the procedure.
1. INTRODUCTION
Rehabilitation of the posterior maxilla with dental implants necessitates a thorough evaluation of both clinical and radiographic findings in order to achieve optimal results. Tooth loss leads to the inevitable resorption of alveolar bone in all dimensions. Trauma can result in significant bone resorption, posing challenges for placing dental implants and the need for bone augmentation procedures [1]. Vertical bone defects can be managed using vertical augmentation techniques, which can be categorized into three main methods, which include bone block graft technique, guided bone regeneration, and distraction osteogenesis [2].
Autogenous bone grafts remain the gold standard for bone grafting due to their trifecta of osteogenesis, osteoinduction, and osteoconduction properties [3]. Autogenous bone grafts can be harvested from various locations, both intraoral and extraoral, with the selection based on the volume of bone required [3]. Autogenous bone grafts harvested from the anterior iliac crest offer numerous advantages, including the ability to harvest a substantial volume, particularly marrowbone, which contains ample osteoblasts and growth factors. They are easily harvested and associated with minimal complications [4].
Exposure of the bone graft to the oral environment represents the most common complication in bone augmentation procedures [5]. The likelihood of this issue escalates with the increase of the bone defect volume, particularly in cases of vertical bone defects [6]. Expertise also proves crucial in averting this complication. Its incidence can result in various repercussions, leading to the loss of bone graft material and overall procedure failure [6, 7]. We present the case of a 30-year-old patient who underwent surgery to reconstruct a significant vertical bone defect in the posterior region of the maxilla using a bone graft harvested from the anterior iliac crest. A novel aspect of our case involves covering the bone block with a dense PTFE membrane and attaching it to the fixation screws. The purpose of this addition is to protect the bone block in the event of exposure, as anticipated during surgical planning due to the size of the bone defect.

A clinical view of the vertical bone defect.
2. CASE PRESENTATION
A 30-year-old male patient was presented to the Oral and Maxillofacial Surgery department at Tishreen University Hospital following a war injury, which led to the loss of teeth in the left posterior maxilla region and a substantial portion of alveolar bone in that area (Fig. 1). The patient demonstrated good overall health, without any systemic diseases, hereditary conditions, congenital anomalies, or syndromes. He is not currently prescribed any medications. The patient was recommended an OPG and CBCT to assess the remaining bone and formulate a treatment strategy (Fig. 2). The cone beam computed tomography (CBCT) scan revealed a significant vertical defect in the lift posterior maxilla, extended from the second premolar to the molars regions. Given the crown height space of approximately 30 mm, a decision was made to opt for localized ridge augmentation utilizing an autogenous bone block with an onlay graft technique instead of a sinus lift procedure.
Under general anesthesia, a full-thickness flap mucoperiosteal was raised using two vertical incisions and one crestal incision. Additionally, the palatal flap was also elevated to fully expose the alveolar ridge. Several perforations were made at the buccal and crestal sides of the recipient bone using a small round. The iliac bone harvesting procedure commenced with an incision made on the skin, located 1.5 cm posterior to the anterosuperior iliac spine (Fig. 2). The 3–4 cm incision ran parallel to the iliac crest, with the aim of preventing damage to the lateral femoral cutaneous nerve. The exposure of the iliac crest proceeded with the elevating of the periosteum. The harvesting site was delineated with a one-mm diameter drill, a series of holes were created, and the cutting was finalized using a rotating disc (Fig. 3). An ample amount of the cancellous bone was harvested using a curette. A hemostatic sponge (Gelfoam, Pfizer, USA) was inserted into the harvested site, and the wound was sutured closed in two layers; the periosteal layer was sutured with vicryl 4/0 (SURGIReal, USA), and the skin was closed with 5/0 nylon (SURGIReal, USA).

Preoperative OPG showed a large vertical defect in the left posterior region of the maxilla.

Harvesting of the bone block from the iliac crest.
The recipient site preparation, graft shaping, and membrane fixation were carried out utilizing a special kit (InnoGenic™ GBR Kit, Cowell Co, South Korea). The harvested thick block was contoured to fit in the recipient site. The bone block was secured in place using two tenting screws (Tenting screw, Cowell Co, South Korea). The spaces formed between the bone block and the host bone were filled using a particulate cancellous bone graft harvested from the iliac crest (Fig. 4). The d-PTFE membrane (Teflon Sheet, Cowell Co, South Korea) was secured to the tenting screws using tenting cap screws (Tenting cap, Cowell Co, South Korea) (Fig. 5). The vertical incisions were extended apically, the periosteum was scored, and the flap was mobilized to permit a tension-free primary closure, which was closed with 4/0 nylon (SURGIReal, USA) (Fig. 6). Patients were prescribed amoxicillin/clavulanate 875/125 mg (Augmentin 1000, Maatouk Pharma, Syria) twice daily for 5 days, potassium diclofenac 50 mg (Flam K, Asia Co, Syria) as required, and antimicrobial mouthwash (Fresh Mouth, BIOGHAR, Syria) for 7 days.
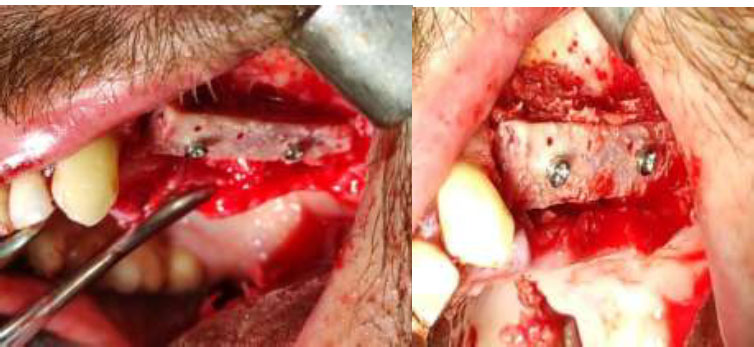
Fixation of the bone block using two tenting screws.
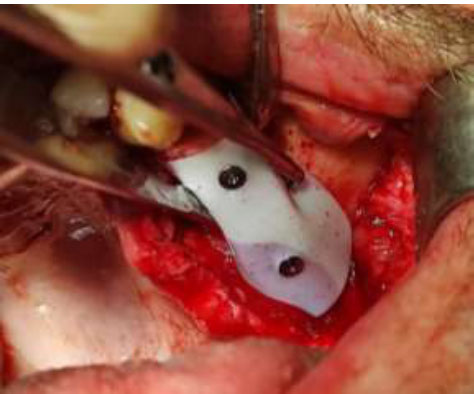
Securing the dPTFE membrane to the bone block using two cap screws.
Although the membrane exposure was anticipated, it was less extensive than expected and occurred after 2 weeks (Fig. 7). The authors only cleaned the exposed area with a saline solution. The patient was recommended to rinse with a saline solution daily and maintain oral care. The Healing process was uneventful, with no significant complications. There were no infections or loss of bone graft material. The membrane was removed 4 weeks after the surgery. A CBCT scan was taken 6 months postoperatively to evaluate the bone height gained. The preoperative and 9-month postoperative mean height was (3.1) mm and (9.6) mm, respectively. The alveolar width gain was (6.5) mm (Fig. 8).

Wound closure using the simple interrupted suturing technique.

Exposure of the dPTFE membrane to the oral cavity after 2 weeks.
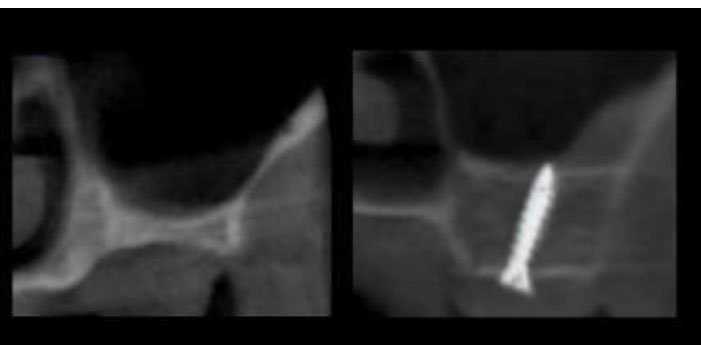
CBCT scan pre-surgery and 9 months post-surgery.
3. DISCUSSION
The Interest in bone grafting materials and techniques has grown significantly following the introduction of intraosseous dental implants. These implants necessitate a sufficient quantity and quality of existing bone, often leading to the need for bone grafting procedures [8, 9]. Vertical alveolar bone augmentation techniques can be categorized into four main methods: bone block graft technique (only graft), guided bone regeneration, osteoperiosteal flaps, and distraction osteogenesis [2].
Bone grafting to address vertical bone defects using bone graft harvested from the iliac crest offers numerous advantages. Firstly, the iliac crest provides a substantial amount of bone graft material, making it well-suited for extensive vertical augmentation procedures. Secondly, iliac bone grafts exhibit high osteogenic potential, facilitating new bone formation and seamless integration with the surrounding bone structures.
3.1. Biocompatibility
Iliac bone grafts are highly tolerated by the body, lowering the chances of rejection or adverse reactions.
3.2. Structural Stability
The dense cortical bone present in the iliac crest provides structural integrity, which is crucial for supporting vertical augmentation and preventing resorption over time [2, 10, 11].
While a bone graft sourced from the iliac crest offers numerous benefits, it also comes with several drawbacks:
3.2.1. Surgical Morbidity
The process of harvesting bone from the iliac crest involves creating an additional surgical site, which can result in donor site morbidity. This may manifest as pain, scarring, and potential complications.
3.2.2. Limited Graft Shape and Size
Iliac bone grafts may not always align perfectly with the shape and size requirements of the recipient site. This mismatch may necessitate additional shaping or manipulation during the surgical procedure.
3.2.3. Resorption Risk
Despite the initial stability, iliac bone grafts may undergo resorption over time, leading to potential volume loss and compromised vertical augmentation results.
3.2.4. Additional Surgical Time and Expertise
Harvesting and preparing iliac bone grafts require specific surgical skills and may extend the duration of the procedure, adding complexity to the overall surgical process [2, 10, 11].
Exposure of bone blocks or barrier membranes in bone augmentation procedures is a common and significant complication, which can pose a threat to the success of the entire procedure [5, 6]. After exposure, the practitioner should anticipate that bone regeneration might not be as intended, as this complication can hinder the expected amount of bone formation. The prognosis may worsen if contamination and bacterial invasion of the bone graft material take place, leading to dissolution and loss of the graft material, which necessitates the removal of the bone block and curettage of the affected area [6]. The prevention of exposure and subsequent complications is essential in maintaining the integrity of the bone graft material and promoting successful bone regeneration. The findings from this case report suggest that the use of d-PTFE membranes can contribute to reducing the risks associated with bone block exposure and enhancing the overall outcomes of vertical bone augmentation procedures in atrophic maxilla cases.
D-PTFE membranes offer outstanding protection by isolating bone block or bone graft material from bacterial contamination. D-PTFE membranes surpass e-PTFE membranes due to their smaller pore size, measuring less than 0.3 µm, compared to e-PTFE membranes ranging from 0.5 to 30 µm. The superior isolation capabilities of d-PTFE membranes stem from their pore size being smaller than the average size of bacteria, which ranges from 0.5 to 5.0 µm. This prevents bacteria from penetrating the bone graft material, effectively preventing contamination [12-16].
Over the years, tenting screws have been utilized in various implantology and bone augmentation practices. These screws have been applied in both horizontal and vertical bone augmentation techniques as a space maintenance device [17-20], as well as in socket and alveolar ridge preservation procedures [21]. In this case, tenting screws were utilized to secure the bone block to the recipient bone. These screws can be connected with tenting cap screws to firmly attach the membrane to the bone block, eliminating the requirement for bone pins. This method offers enhanced surgical convenience, ensuring a precise fit of the membrane onto the bone block and reducing surgical time. Moreover, the membrane can be easily removed through a crestal incision, eliminating the necessity for extensive flap dissection.
CONCLUSION
Based on our case report findings, it can be inferred that applying d-PTFE to cover the bone block in extensive posterior maxillary vertical augmentation procedures effectively shields the bone block from bacterial contamination, lowers the likelihood of complications, and enhances the predictability of the procedure. The incorporation of tenting screws with tenting cap screws for securing the bone block and membrane simplifies the surgical process, decreases its duration, and streamlines membrane removal.
AUTHORS’ CONTRIBUTIONS
W.A.: Study conception and design; Z.A.: Data collection; Z.A.: Analysis and interpretation of results; W.A. and Z.A.: Draft manuscript. All authors reviewed the results and approved the final version of the manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The ethical approval for publication of this case report was provided by the Ethical Review Board of Tishreen University Hospital, Syria with Number 2605 on 20 Feb 2024.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for publication of this case report and accompanying images.


