All published articles of this journal are available on ScienceDirect.
Surgical Orthodontic Treatment of Class III Malocclusion with Unilateral Open Bite Due to Impacted Premolar with Dilacerated Root: A Case Report
Abstract
Background
Dilacerated teeth may interfere with eruption and movement, making orthodontic treatment difficult.
Case Report
This case report describes successful surgical orthodontic approaches for a 14-year-old girl with skeletal Class III malocclusion, a unilateral open bite caused by a severely dilacerated mandibular left first premolar, and severe crowding in the mandibular dentition. The patient underwent surgical subluxation of the dilacerated premolar, followed by a combination of non-extraction orthodontic therapy and orthognathic surgery.
A left lateral open bite caused by a severely dilated mandibular left first premolar was corrected through tooth traction after subluxation for root apical transection. Class I molar relationships and improved facial profiles were achieved with maxillary advancement, adjunctive counterclockwise mandibular rotation, and genioplasty.
Conclusion
This case report suggests using subluxation in severely dilacerated teeth to enable orthodontic tooth movement with high stability, thereby expanding the possibility of non-extraction treatment.
1. INTRODUCTION
Skeletal class III malocclusion has been reported to be the most frequent surgical orthodontic treatment for dentofacial deformities in the Asian region [1]. One characteristic of skeletal class III malocclusion is that the mandibular incisors are usually lingually inclined to compensation [2, 3]. In patients planned for orthognathic surgery for skeletal class III malocclusion, pre-surgical orthodontic treatment involves positioning the mandibular incisors labially for decompensation. Subsequently, mandibular setback orthognathic surgery is performed. However, the gingival labial recession caused by excessive labial proclination of the mandibular incisors has been reported, which occurs due to the exposure of the roots to the alveolar bone [4, 5]. In contrast, extracting mandibular premolars during presurgical orthodontic treatment for alignment of crowding allows for further lingual inclination of the mandibular incisors. As a result, inadequate esthetic improvement is finally obtained due to a reduced amount of mandibular setback [3-5].
The under-eruption of permanent teeth due to severely dilacerated roots may cause open bite malocclusion. The prevalence of root dilacerations greater than 90° has been reported to be 3.78% [6]. Roots with greater than 90° dilacerations show a predilection for the mandibular third and maxillary first molars. In addition, the prevalence in mandibular first premolars is 1.42% [7]. Factors contributing to dilaceration include dentoalveolar infection of deciduous predecessors [8], ectopic development of the tooth germ and lack of space [7], presence of an adjacent cyst or tumor [9-12], mechanical interference with eruption due to malresorption of deciduous predecessors [12], and hereditary factors [13-15]. Impacted teeth with dilacerated roots may cause aesthetic, masticatory, hygienic, and potential problems in the adjacent teeth and structures [12]. Conventional orthodontic treatment for dilacerated teeth involves extraction or prosthesis [16], although several orthodontic approaches involving orthodontic traction have been reported [12, 16].
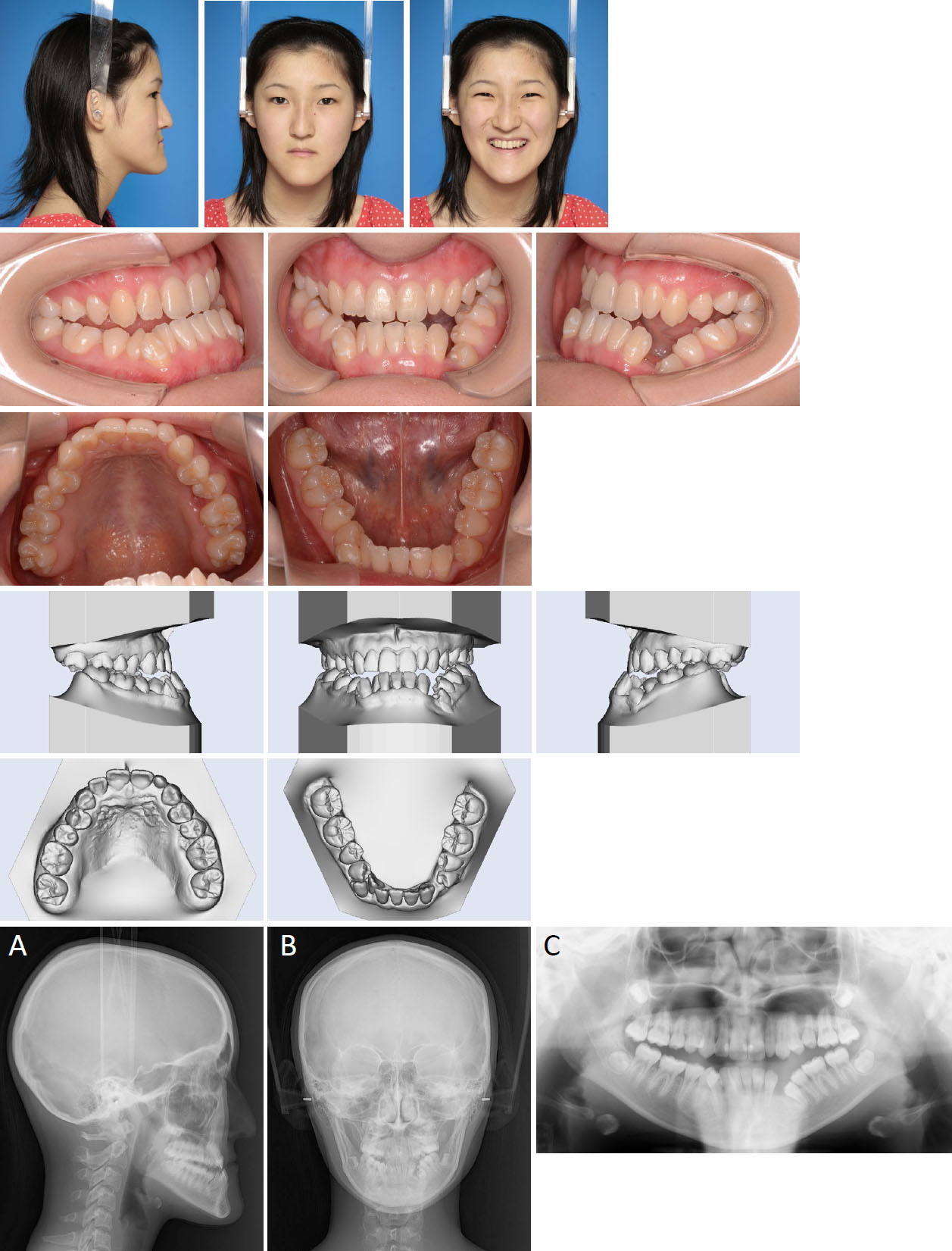
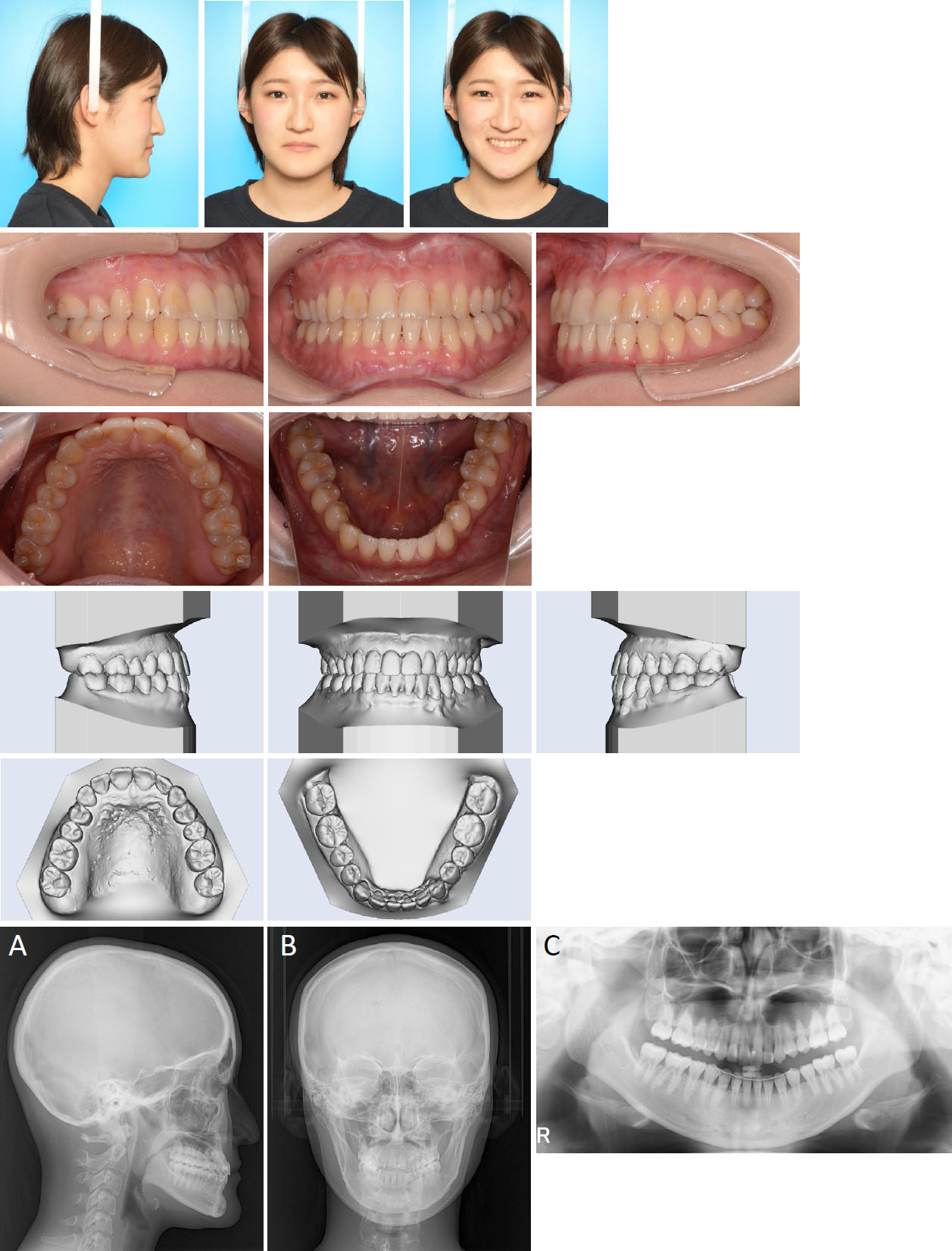
Pretreatment facial, intraoral photographs and digital models, (A) Pretreatment lateral cephalogram; (B) postero- anterior cephalogram; (C) panoramic radiograph.
In the present case, a patient with severe skeletal class III malocclusion with a left lateral open bite due to dilaceration of the mandibular left first premolar was treated with surgical subluxation of the dilacerated premolar, followed by a combination of non-extraction orthodontic therapy and orthognathic surgery.
2. CASE REPORT
2.1. Etiology and Diagnosis
The patient was a 13-years and 6-month-old girl who presented for orthodontic treatment with a chief complaint of mandibular protrusion and required surgical orthodontic treatment. However, she was kept under observation until the end of the growth period because she showed pubertal growth. The prospect of growth termination was identified at the age of 14 years and 5 months, and presurgical orthodontic treatment was initiated. The patient had a concave profile due to retruded maxilla and prognathic mandible (Fig. 1A-C). Intraoral examination revealed a complete Angle Class III molar relationship on both sides with severe crowding of the mandibular dentition. The patient had a bilateral open bite, and the left lateral open bite was more severe due to infraocclusion of the mandibular left first premolar. The maxillary left lateral incisor is a microdont. The maxillary dental midline coincided, while the mandibular dental midline deviated 3.0 mm to the right of the facial midline. The overjet was -1.5 mm, and the overbite was +0.5 mm.
Panoramic radiography revealed no horizontal or vertical bone loss and normal root length (Fig. 1C). The root of the mandibular left first premolar was bent 90° proximally in the apical 1/3, showing proximal inclination and infraocclusion (Fig. 2A). Additionally, a few millimeters of space existed between the left first premolar and the canine. The bilateral maxillary and mandibular third molars were buried in the alveolar bone. The cephalometric assessment showed that the maxilla was retruded (SNA angle, 78.2°), and the mandible was protruded (SNB angle, 85.1°) to the cranial base, resulting in a skeletal Class III relationship (ANB angle -6.9°) with an average mandibular plane angle (FMA, 31.2°) (Table 1). The size of the maxilla was average (PTM-A/PP, 46.4 mm), whereas the mandibular ramus height and body length were large (GO-Me, 81.6 mm; Ar-Me, 116.7 mm; Ar-Go, 47.2 mm) compared with the Japanese norm. Both the maxillary incisors (U1-FH, 105.1°) and mandibular incisors were inclined lingually (FMIA, 91.5°). Posteroanterior (PA) cephalometric tracing revealed that the menton coincided with the facial midline (Fig. 1B). Cervical vertebral tracing showed cervical stage 6 (CS6), indicating that peak mandibular growth had ended at least two years before this stage (not shown). In addition, the annual growth in height was within 1.0 cm, confirming that the growth was almost complete.
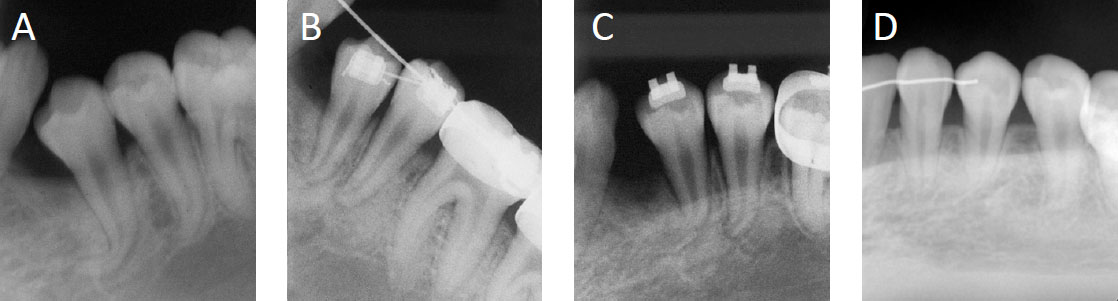
Dental radiographs of mandibular left first premolar, (A) Pretreatment; (B) After 2 weeks of subluxation; (C) After 2 months of subluxation; (D) 2 years posttreatment.
| Angular Analysis (°) | Mean | SD | Pre treatment (T1) | Post Treatment (T2) | 2 Years Post Treatment (T3) |
|---|---|---|---|---|---|
| SNA | 80.8 | 3.6 | 78.2 | 82.1 | 82.1 |
| SNB | 77.9 | 4.5 | 85.1 | 83.5 | 83.5 |
| ANB | 2.8 | 2.4 | -6.9 | -1.4 | -1.4 |
| FMA | 30.5 | 3.6 | 31.2 | 27.1 | 27.1 |
| Gonial angle | 122.1 | 5.3 | 123.6 | 118.7 | 118.7 |
| Occ Plane to FH | 16.9 | 4.4 | 16.2 | 12.9 | 12.9 |
| U1-FH | 112.3 | 8.3 | 105.1 | 115.1 | 115.1 |
| L1-Mp | 93.4 | 6.8 | 59.1 | 85.9 | 83.1 |
| FMIA | 56 | 8.1 | 91.5 | 67.9 | 70.7 |
| IIA | 123.5 | 10.6 | 166.1 | 132.3 | 134.8 |
| Linear analysis (mm) | - | - | - | - | - |
| S-N | 67.9 | 3.7 | 69.5 | 69.5 | 69.5 |
| N-Me | 125.8 | 5 | 127.1 | 122.4 | 122.4 |
| N/PP | 56 | 2.5 | 59.1 | 59.1 | 59.1 |
| Me/PP | 68.6 | 3.7 | 68.2 | 64.6 | 64.6 |
| PTM-A/PP | 47.9 | 2.8 | 46.4 | 46.4 | 46.4 |
| Go-Me | 71.4 | 4.1 | 81.6 | 77.2 | 77.2 |
| Ar-Me | 106.6 | 5.7 | 116.7 | 111.8 | 111.8 |
| Ar-Go | 47.3 | 3.3 | 47.2 | 48.1 | 48.1 |
| Wits appraisal | -1.1 | 1.8 | -15.5 | -6.8 | -6.8 |
| Overjet | 3.1 | 1.1 | -1.5 | 2 | 2.5 |
| Overbite | 3.3 | 1.9 | 0.5 | 2 | 2 |
We diagnosed this patient with Angle Class III malocclusion, a skeletal Class III jaw-base relationship, severe crowding of the mandibular dentition, left lateral open bite due to severely dilacerated mandibular left first premolar, and lingual inclination of the maxillary and mandibular incisors.
2.2. Treatment Objectives
The treatment objectives were as follows: correction of facial appearance, establishment of an ideal incisor and molar relationships, and correction of the dilacerated mandibular left first premolar.
2.3. Treatment Alternatives
To achieve treatment objectives, two possibilities were considered and discussed with the patient.
1) The first alternative involved a combination of fixed orthodontic treatment with extraction of the maxillary first premolars and orthognathic surgery using Le Fort I osteotomy for maxillary advancement and impaction combined with bilateral sagittal split osteotomy for mandibular setback. Corticotomy of the mandibular incisors and osteotomy of the mandibular left first premolar and posterior teeth were planned as additional surgical procedures. Maxillary and mandibular third molar extractions are required. The advantage of this plan may be correcting mandibular protrusion by increasing the mandibular setback. In addition, corticotomy of the mandibular incisors may reduce the risk of gingival recession due to excessive labial movement of the mandibular incisors within the thin trabecular bone. Furthermore, the infraocclusion of the mandibular left molar was corrected using osteotomy. In contrast, extracting the bilateral maxillary first premolars may cause an increase in the lingual inclination of the maxillary incisors, and the appearance of the retruded upper lip cannot be improved. Combining corticotomy of the mandibular incisor with osteotomy of the mandibular left molars increases surgical invasiveness.
2) The second alternative involved combining fixed orthodontic treatment with non-extraction and orthognathic surgery using Le Fort I osteotomy for maxillary advancement combined with bilateral sagittal split osteotomy to adjust the mandibular position. Maxillary and mandibular third molar extractions are required. Although the number of mandibular setbacks was less than that in the first plan, genioplasty as an additional surgical approach contributed to improving the profile and reducing the long lower facial height by removing the middle of the bony mentum. To minimize gingival recession, alignment by labial inclination of the mandibular incisors was performed separately during the pre- and post-surgical orthodontic stages. A dilaceration tract was observed in the mandibular left first premolar immediately after surgical subluxation and apical root dissection. This plan is less surgically invasive than the first plan.
After explaining the treatment options to the patient, the second option was chosen. Informed consent was obtained from the guardian prior to the procedure.
2.4. Treatment Progress
The maxillary teeth were bonded with pre-adjusted edgewise brackets (0.022 × 0.028-inch slot), and leveling and alignment were initiated using sequential nickel-titanium alloy wires. Additionally, a transpalatal arch was placed on the maxillary first molar to reduce the width between the molars. The following month, pre-adjusted edgewise brackets (0.022 × 0.028-inch slot) were bonded to the mandibular teeth, excluding the right mandibular lateral incisor, canine, and both first premolars. The mandibular teeth were then leveled and aligned using sequential nickel-titanium alloy wires. The mandibular dentition was expanded by the buccal uprights of the lingually inclined mandibular molars.
Under local anesthesia, the mandibular third molars were extracted, and the mandibular left first premolar was subluxated for root apical transection. During apical root transection, the elevator was inserted into the distobuccal cervical area, the teeth were moved, and the root was intentionally fractured at the tip region. Orthodontic traction of the mandibular left first premolar was initiated five days after subluxation when the spontaneous pain had disappeared. A pre-adjusted edgewise bracket was bonded to the mandibular left first premolar, and orthodontic force was applied by placing a round 0.014-inch nickel-titanium wire over the 0.016 × 0.022-inch main beta-titanium archwire. Two weeks later, the mandibular left first premolar showed decreased mobility and tenderness without any spontaneous pain (Fig. 2B). Seven weeks later, mobility and tenderness disappeared in the mandibular left first premolar, the archwire was replaced with a 0.018-inch nickel-titanium alloy wire, and orthodontic traction was continued. Two months after the subluxation, partial resorption of the root fracture fragment was observed (Fig. 2C). Eight months after the initiation of presurgical orthodontic treatment, 0.019 × 0.025 inch beta-titanium wires were placed in both the arches for intermaxillary fixation during orthognathic surgery, which was followed by Le Fort I osteotomy, bilateral sagittal split osteotomy, and genioplasty. The bony mentum was vertically reduced by 3.0 mm at the pogonion position. To correct the deteriorated molar relationship to Angle Class III on the left side due to orthognathic surgery relapse, a miniscrew implant (1.6 mm in diameter, 6 mm in length, Platon Japan Co., Tokyo, Japan) was placed in the buccal region between the premolars, followed by the retraction of the mandibular arch using miniscrew anchorage. The fixed appliances were removed after three years and three months of treatment (Figs. 3 and 4), and the patient received a maxillary wraparound retainer and a mandibular bonded lingual retainer. The patient was followed up for two years (Fig. 5).
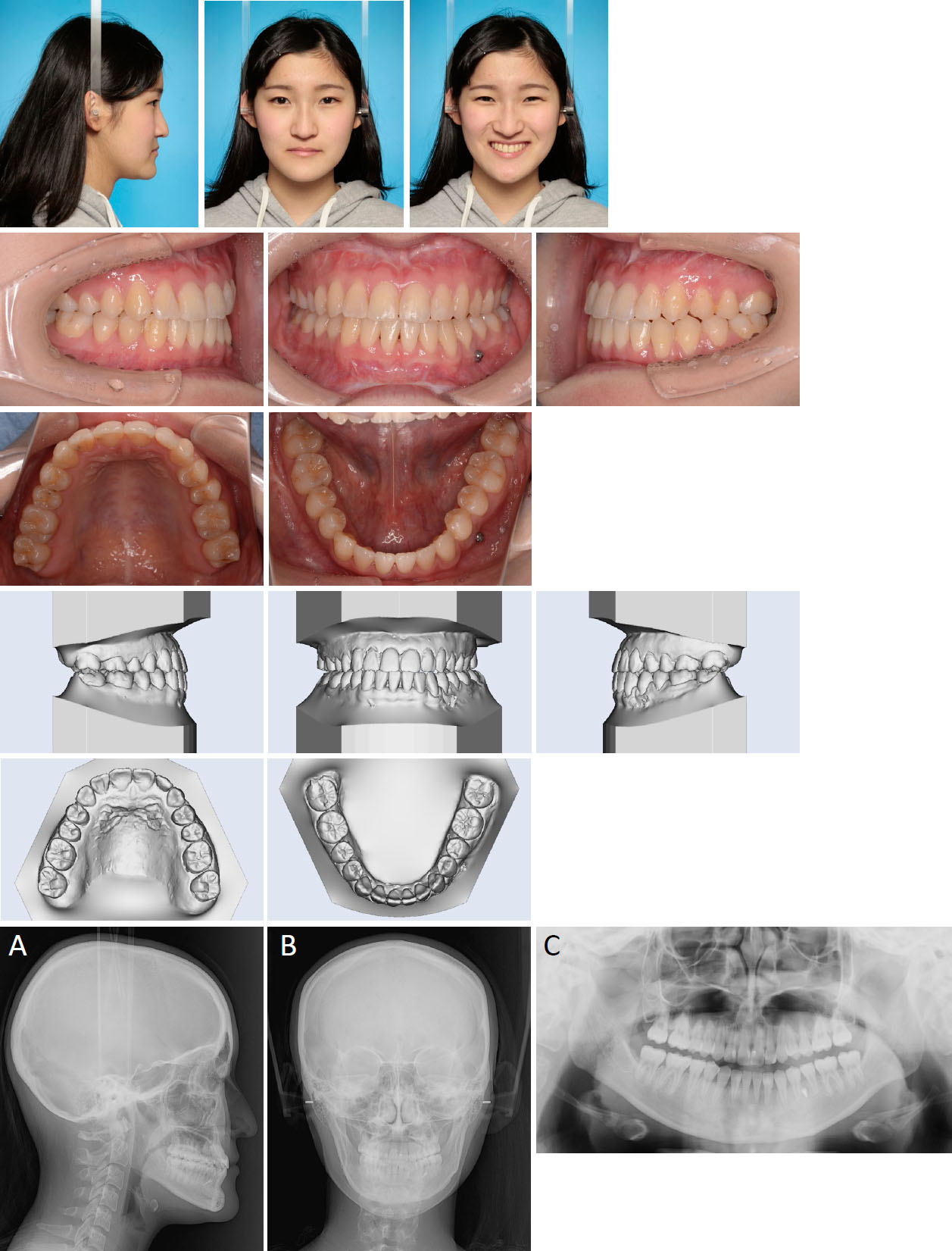
Posttreatment facial, intraoral photographs and digital models, (A) lateral cephalogram; (B) posteroanterior cephalogram; (C) panoramic radiograph.
2.5. Treatment Results
Post-treatment records showed that the facial profile was improved by the advanced maxilla, adjustive mandibular counterclockwise rotation, and genioplasty (Fig. 3). The anterior crossbite and lateral open bite were resolved, and proper Class I canine-molar relationships were achieved on both sides. The mandibular and maxillary anterior crowding was successfully corrected. Although the left lateral occlusion was imperfect, the patient’s chief complaint and facial profile improved. Panoramic radiography showed satisfactory root parallelism, although moderate apical root resorption was observed in the anterior mandibular teeth (Fig. 3C). Cephalometric analysis (Fig. 3A, Table 1) and superimposition (Fig. 4) showed that the SNA angle (82.1°) was improved by advancing the maxilla. The mandibular plane angle decreased from 31.2° to 27.1° owing to the influence of counterclockwise rotation and genioplasty. The mandibular incisors were significantly proclinated from 91.5° to 67.9° (FMIA), and the maxillary incisors were proclinated from 105.1° to 115.1° (U1-FH). The maxilla was advanced by 4.5 mm and impacted by 1.0 mm at the anterior nasal spine, and the mandible was positioned in an equivalent anteroposterior position with a slight counterclockwise rotation. After two years of retention, the lateral occlusion became shallower due to the buccal inclination of the mandibular left second premolar, and a slight leftward deviation of the mandibular dental midline was observed. However, the patient showed good occlusal stability and facial aesthetics (Fig. 5). Resorption of the fractured root apex of the left mandibular first premolar was also observed (Fig. 2D).
3. DISCUSSION
3.1. Differences in the Treatment Choice of Non-extraction or Extraction of Premolar on Decompensation of the Mandibular Dentition in Presurgical Orthodontic Treatment
In this case, the anterior section of the mandibular arch showed severe crowding with a 7 mm arch length discrepancy, and extraction of the mandibular left first premolar was also considered. However, mandibular premolar extraction for Class III surgery patients has shown that lingually inclined mandibular incisors cannot be fully corrected, which reduces the correction of the anteroposterior relationship between the maxilla and the mandible. Therefore, the left first premolar was not extracted. Furthermore, because of the infraocclusion of the mandibular left first premolar, the mandibular left second premolar and first molar were also infraoccluded, and the occlusal plane angle of the mandibular left lateral teeth was greater than that of the mandibular right lateral teeth. The mandibular left lateral teeth were considered for osteotomy during orthognathic surgery to align them with the occlusal plane.
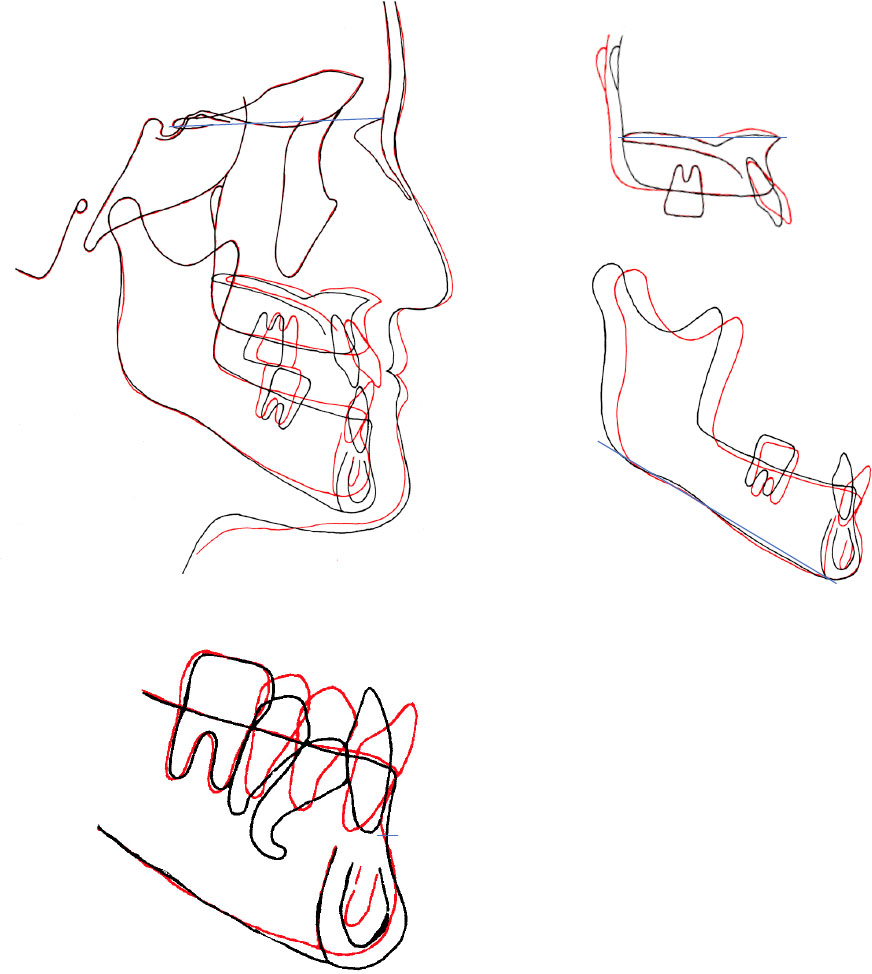
Superimposed lateral cephalometric tracings; pretreatment, black line; posttreatment, red line.
Facial, intraoral photographs and digital models after 2 years of retention, (A) lateral cephalogram; (B) posteroanterior cephalogram; (C) panoramic radiograph.
3.2. Criteria for Anteroposterior Intermaxillary Relationships in Surgical and Nonsurgical (camouflage) Treatment Cases in Skeletal Class III
A recent study investigated 403 orthognathic patients and reported that Class III patients were the most prevalent (62.3%), and their mean ANB angle was –3.57° (95% Cl, –3.92° to –3.21°) [1]. Cephalometric measure- ments that relate the maxilla to the mandible (e.g., ANB angle and Wits appraisal) are particularly helpful for quantifying the severity of malocclusion. The patient treated in the present report showed a more severe skeletal Class III jaw-base relationship (ANB, –6.9°) compared to the mean values (–3.57°) in recent investigations [1]. In addition, Wits appraisal is most decisive in distinguishing orthognathic surgical treatment cases from camouflage treatment cases [12]. The previous study reported that the average Wits appraisal for surgical treatment was –13.02 mm, and for camouflage treatment was –4.54 mm. The Wits appraisal value of the present report was –15.5 mm and is classified as a surgery accordingly.
3.3. Orthodontic Tooth Traction after Subluxation for the Dilacerated Premolar
The mandibular left first premolar had erupted with infraocclusion and may have had ankylosis in addition to eruption failure due to a root deviation of 90°. Orthodontic treatment for ankylosis includes surgical subluxation, followed by tooth movement [17], osteotomy [18], and preprosthetic orthodontic treatment after extraction [2]. Dental radiographs (Fig. 2A) and cone-beam computed tomography (CBCT) (not shown) showed a continuous or evident periodontal ligament space, making the possibility of ankylosis unlikely. Ankylosis was diagnosed by confirming the absence of periodontal ligament space using CBCT [19]. Although widespread ankyloses can be diagnosed using CBCT, small ankyloses cannot be diagnosed using CBCT alone [19]. Hence, orthodontic tooth movement should be considered in the differential diagnosis of ankylosis [20]. Based on the radiographic findings in this case, the possibility of ankylosis of the mandibular left first premolar was low; however, a 90° root deviation and infraocclusion were observed. Therefore, we considered the possibility of localized ankylosis, and subluxation was used to fracture the dilacerated root and mobilize it before orthodontic traction was applied. Orthodontic traction was not initiated immediately after the subluxation because the mandibular left first premolar was significantly mobile, and there was spontaneous pain. Initially, a light orthodontic force was applied to the first premolar using a 0.014 inch nickel-titanium alloy wire to prevent the obstruction of blood flow to the periodontal ligament and pulp due to excessive orthodontic force. Two weeks after the subluxation, the mobility of the mandibular left first premolar decreased, and orthodontic traction was continued using an upsized wire. Seven weeks after the subluxation, the mobility of the mandibular left first premolar was stabilized, and further orthodontic traction and leveling continued.
3.4. Posttreatment Stability of Mandibular First Premolar guided Eruption by Orthodontic Traction after Subluxation
After six years and eight months of retention, the mandibular left first premolar remained vital, which may have been due to the light and continuous orthodontic force applied using a nickel-titanium wire after subluxation, which prevented pulp necrosis due to blood flow inhibition. A case of pulpal necrosis due to traction after subluxation has been reported [21]. Therefore, it is important to apply an appropriate orthodontic force after subluxation and not inhibit pulpal blood flow. It has also been reported that the fractured roots of permanent incisors are physiologically resorbed by connective tissue interposition, which usually occurs within one year after root fracture [22, 23]. In this case, resorption of the fractured root was observed two months after apical transection (Fig. 2C), and the fractured root was completely resorbed two years after retention (Fig. 2D). Connective tissue was interposed between the mandibular left first premolar and its fractured root as it healed, and physiological root resorption occurred.
CONCLUSION
Our case report suggests that the use of subluxation in severely dilacerated premolars expands the potential for presurgical orthodontic treatment with non-extraction in skeletal Class III orthognathic surgery. This technique extrudes dilacerated premolars without causing pulp necrosis or periodontal problems and develops a proper lateral occlusal relationship. This treatment improved the skeletal relationships and facial profiles of patients with severe skeletal Class III malocclusion and dilaceration.
AUTHORS’ CONTRIBUTION
H.K. and I.M.: Study conception and design; M.Y., A.Y., Y.M., and T.S.: Draft manuscript. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| PA | = Posteroanterior |
| CS6 | = Cervical Stage 6 |
| CBCT | = Cone-Beam Computed Tomography |
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient’s guardian for the publication of this case report, including accompanying images.


