All published articles of this journal are available on ScienceDirect.
Influence of Acidic Drinks and Brushing on Microhardness of Restorative Resin Materials
Abstract
Background
Various factors, including acidic diets and beverages, can compromise the longevity of restorations by affecting their physical and mechanical properties.
Objectives
This study aims to evaluate, in vitro, the performance of different resin restorative materials and their interaction in an exogenous acid medium (orange juice), as well as erosion and whether there is interference in the microhardness of the composite resins.
Materials and Methods
48 samples from your different materials were distributed across 8 groups. Microhardness measurements were conducted before and after immersion in orange juice for 2 weeks, followed by brushing simulations. The data was analyzed using SPSS 20, initially checking for normality, and then two-way ANOVA followed by Tukey’s post hoc tests were applied for comparison at the significance level of 95%.
Results
There was a significant change in microhardness values among both groups (orange juice and distilled water) (p<0.05), with the orange juice group displaying a greater reduction in hardness over time. Vita Enamic showed the greatest amount of reduction in values (p<0.05) yet still maintained higher values compared to the other materials. Charisma Classic experienced the least, though a significant change (P<0.05) in microhardness when exposed to orange juice.
Conclusion
Overall, all materials showed a significant decrease in microhardness when immersed in orange juice, which highlights the erosive effects of acidic environments on resin restorative materials. Simulated brushing after acid exposure had minimal impact on the results.
1. INTRODUCTION
Resin composites have become the preferred material for dental restorations due to their similarity to natural tooth structure in terms of physical, chemical, and mechanical properties, as well as aesthetics [1]. For this reason, composite resins have been the subject of intensive research over the past decade aimed at enhancing their unfavorable properties [2]. Surface micro- hardness is a critical property for composite materials, influencing performance, durability, aesthetics, and the longevity of dental restorations, helping them withstand various forces. High microhardness ensures resistance to wear and abrasion, maintaining surface integrity and smoothness, which is crucial for preventing plaque accumulation and staining. Preserving this microhardness is essential to prevent issues like microfractures, enhance structural integrity, ensure the material's resilience to masticatory forces, and avoid long-term problems such as pigment retention and secondary caries. This connection highlights the significance of both material choice and maintenance for successful dental restorations [3].
Numerous factors can influence the properties of restorative materials, including cariogenic microorga- nisms, acidic foods and drinks, and salivary composition. The contemporary diet, with its high consumption of acidic beverages and foods, significantly impacts the longevity and effectiveness of these materials. Dietary awareness has become a significant concern in contemporary society, especially considering the widespread consumption of carbonated drinks among the youth, persisting into adulthood [4]. This habit poses a substantial risk as acidic beverages, such as soft drinks (like orange juice and cola), can cause erosion of resin composites. This erosion not only affects the structural integrity of the material but also compromises the aesthetic quality of restorations, leading to degradation and loss of both physical and mechanical properties. The mechanisms behind this erosion are multifaceted and linked to various factors, including filler content, distribution, matrix resin composition, and the impact of silane surface treatment on fillers. These factors can potentially alter the microhardness, a critical property affecting the physiochemical characteristics of restorations, including compressive strength and abrasion resistance [5, 6].
Furthermore, the mechanical properties of resin composites are heavily influenced by both the concen- tration and particle size of the filler materials used. Hybrid and micro hybrid resins are characterized by a wide range of particle sizes, which allows for high filler loading. This high filler content significantly enhances the overall strength and durability of the composite material. This emphasizes the intricate relationship between dietary habits, erosion of resin composites, and the material's micro-hardness, underlining the importance of addressing both dietary choices and the composition of restorative materials as they are essential for ensuring the success and longevity of dental restorations. This comprehensive approach is vital for maintaining oral health and the aesthetic quality of dental work over time [7]. In a previous study conducted by Aboulmagd et al. (2022), the impact of two acidic agents on the microhardness of nanofilled and microhybrid resin composite materials was investigated.The composites were immersed in different storage media: distilled water, boxed cola, and orange juice. The findings showed that orange juice caused the most significant reduction in hardness values. While the microhardness of both resin composites decreased over time, the microhybrid composite demonstrated greater resistance to degradation than the nanofilled composite [8].
The effects of acidic conditions on surface micro- hardness have been previously investigated in several studies. Poggio et al. (2018) experimented to evaluate how immersion in acidic beverages impacts the microhardness of various aesthetic restorative materials. Their findings revealed that acidic solutions significantly alter the microhardness of these materials, with varying effects depending on the specific material [7]. Similarly, Moyin et al. (2020) investigated the effect of acidic beverages on the microhardness of several aesthetic restorative mate- rials and observed that while some materials performed better than others, all exhibited surface degradation after repeated exposure [9]. These studies highlight the importance of understanding how different esthetic resto- rative materials respond to acidic conditions, emphasizing the need for careful consideration of material selection and dietary habits in maintaining the durability and performance of dental restorations.
Brushing is recommended to counteract the staining caused by acidic beverages to remove superficial stains and improve the color stability of dental resin composite restorations. However, toothbrush abrasion can lead to aesthetic and biological drawbacks over time. The mecha- nical action of brushing can degrade the polymer matrix of the composite resin, leading to changes in surface hardness and further promoting discoloration [10]. Previous studies investigated the idea that enamel surface hardness might be lowered by brief contact with acidic beverages and that noticeable enamel loss can occur when toothpaste is brushed afterward. Even after numerous exposures, noticeable enamel surface erosion may still result from subsequent brushing [11].
This study aimed to shed light on the complex relationships between exposure to acidic beverages, subsequent brushing, and their combined impact on the microhardness characteristics inherent in various compo- site materials. By documenting the microhardness progression at each stage of the experiment, the research aimed to provide comprehensive insights into how these materials respond to both chemical and mechanical challenges. This will contribute valuable knowledge to material selection in dental practice and enhance the longevity and effectiveness of dental restorations.
The null hypotheses were (1) Acidic exposure does not cause significant changes in microhardness values of resin restorative materials, (2) Brushing does not lead to further significant alterations in microhardness measurements, and (3) There is no significant difference between the micro- hardness of the different materials used.
2. MATERIALS AND METHODS
Four types of resin restorative materials were used:
Charisma® Diamond (Kulzer South America) – Hybrid Nano Composite Resin; Charisma® Classic (Kulzer South America) – Micro Hybrid Composite Resin; Opus Bulk fill APS (FGM®) – Composite resin in bulk or filling; Vita Enamic® (Vita) – CAD/CAM Resin Block.
The sample size was calculated considering the microhardness values for calculating f (effect size). The G Power 3.1 software (Heinrich-Heine-Universität, Dussel- dorf, Germany) was used with a 95% significance level and 80% test power. The calculation obtained was 6 samples per group. A total of 48 samples (n=6) were distributed as follows:
Group 1: Hybrid Nano Composite Resin (Charisma® Diamond) control.
Group 2: Hybrid Nano Composite Resin (Charisma® Diamond) orange juice.
Group 3: Micro hybrid composite resin (Charisma® Classic) control.
Group 4: Micro hybrid composite resin (Charisma® Classic) orange juice.
Group 5: Composite resin in bulk or filling (Opus Bulk fill APS) control.
Group 6: Composite resin in bulk or filling (Opus Bulk fill APS) orange juice.
Group 7: CAD/CAM Resin Block (Vita Enamic®) control.
Group 8: CAD/CAM Resin Block (Vita Enamic®) orange juice.
In a metallic matrix with dimensions of 8.4 mm in diameter and 2.5 mm in height, samples of Charisma® Diamond and Charisma® Classic resin were made. First, the mold was cleaned, and a glass plate was placed as a base, and. With the aid of a micro brush, liquid vaseline was inserted throughout the inner part of the metallic matrix to facilitate the removal of the sample after its preparation. It was inserted in increments of 2 in 2mm with the resin spatulas, and a glass slide was placed on the matrix and light-cured until the entire mold was completed. In the case of the composite resin Bulk fill (Opus Bulk Fill APS), the procedure was almost the same; the only difference was that it was inserted in one increment, as this resin allows this type of procedure.
The CAD/CAM resin blocks (Vita Enamic®) were made in a different way. First, they were cut from their metallic base with the help of an IsoMet cutting machine (Buehler®); subsequently, they were sanded on the Aropol E polisher (Arotec®) with water sandpaper in 220 grammages under abundant irrigation until obtained a cylindrical shape that adapted to the internal part of the metallic mold. Then, with instant glue, the blocks were attached to their metallic bases again, and 3 mm high segments were cut in the IsoMet cutting machine (Buehler®).
Finally, all samples were polished with water sand- paper, in weights 600, 1200, and 2000, under abundant irrigation, and after all samples were ready, they were numbered and separated into 8 groups (n=6).
The microhardness of each sample was measured. Five measurements were made along the surface of samples under a load of 50g for 15s. Subsequently, the average surface microhardness was calculated in Knoop (KHN, kg/mm2). These first measurements were called imme- diate measurements.
Each material studied had both a control group (distilled water) and a group immersed in orange juice, which was immersed for two weeks and stored in an oven at 37°C, with these substances being changed every 48 hours. After a period of two weeks, the samples were washed with distilled water, and the surface micro- hardness tests were performed again using the same process mentioned above. These measurements were called initial measurements. Then, the samples were placed in the brushing machine (two samples of each material, totaling eight samples per brushing cycle). The brushing machine was programmed to perform 500 rpm (rotation per minute), with a cycle of one hour, thus, each brushing cycle had 30,000 rotations, which is equivalent to one year of brushing. For brushing, Colgate® dentifrice maximum anti-cavity protection was used, and 6 g of this dentifrice was diluted to 100 ml of water. After brushing, the samples were cleaned again with distilled water, and the surface microhardness tests were performed, the same as above. These measurements were called final measure- ments.
2.1. Statistical Analysis
The statistical analysis for this study involved comparing mean microhardness values between control and experimental groups using appropriate tests. The data was analyzed using SPSS 20, initially checking for normality, and then two-way ANOVA followed by Tukey’s post hoc tests were applied for comparison at the significance level of 95%.
3. RESULTS
Looking at the data, Charisma® Diamond and Charisma® Classic both show statistically significant changes in their properties from the immediate to the final stage, as indicated by the p-values < 0.05. On the other hand, Opus Bulk fill APS (FGM®) demonstrates no statistically significant difference between the immediate, initial, and final stages, with p-values > 0.05. Vita Enamic® displays significant changes similar to Charisma materials, with notably higher mean values < 0.05 (Tables 1 and 2).
3.1. Charisma® Diamond
Both groups experienced a significant decrease in hardness at the initial stage (p<0.05). The reduction was slightly more pronounced in the orange juice group compared to the control group.
| Material | Immediate | Initial | Final | Valor-P |
|---|---|---|---|---|
| Charisma® Diamond | 87.6 ± 23.75 | 67.5 ±16.85 | 73 ± 17.12 | < 0.05 |
| Charisma® Classic | 96.2 ± 33.5 | 62.9 ± 22.01 | 68.5 ± 20.22 | < 0.05 |
| Opus Bulk fill APS (FGM®) | 48.8 ± 19.5 | 46.1 ± 14.56 | 44.5 ± 20.58 | > 0.05 |
| VitaEnamic® | 305.5 ±184.3 | 223.5±115.82 | 250.5 ±77.28 | < 0.05 |
| Material | Immediate | Initial | Final | Valor-P |
|---|---|---|---|---|
| Charisma® Diamond | 102 ± 34.7 | 79.25±26.77 | 77 ± 17.98 | < 0.05 |
| Charisma® Classic | 92.2 ± 32.2 | 76.55± 25.98 | 77.5 ± 14 | < 0.05 |
| Opus Bulk fill APS (FGM®) | 67.4 ± 43.6 | 50.7 ± 9.77 | 50.3 ± 18.76 | < 0.05 |
| VitaEnamic® | 303 ± 97 | 251 ±72.95 | 268.5 ± 51.99 | < 0.05 |
The control group showed a slight increase in hardness between the initial stage (67,5±16,85) and the final stage (73 ± 17,12) (Fig. 1). On the other hand, the orange juice group experienced a modest decrease in hardness (Fig. 2).
Over the entire period, the orange juice group exhibited a greater overall reduction in hardness than the control group (Table 3).
3.2. Charisma® Classic
Both groups had the same immediate measurement (92.2 MPa), showing later a reduction in microhardness at the initial stage, with the control group experiencing a more significant decrease than the orange juice group (Figs. 1 and 2). Throughout the progression from the initial stage to the final stage, both groups exhibited marginally elevated measurements, with the control group showing a slightly greater increase.
Overall, the measurements at the end indicate a statistically significant decrease in hardness in both groups (p<0.05). However, the samples exposed to orange juice experienced a lower reduction than those in the control group (Table 3).
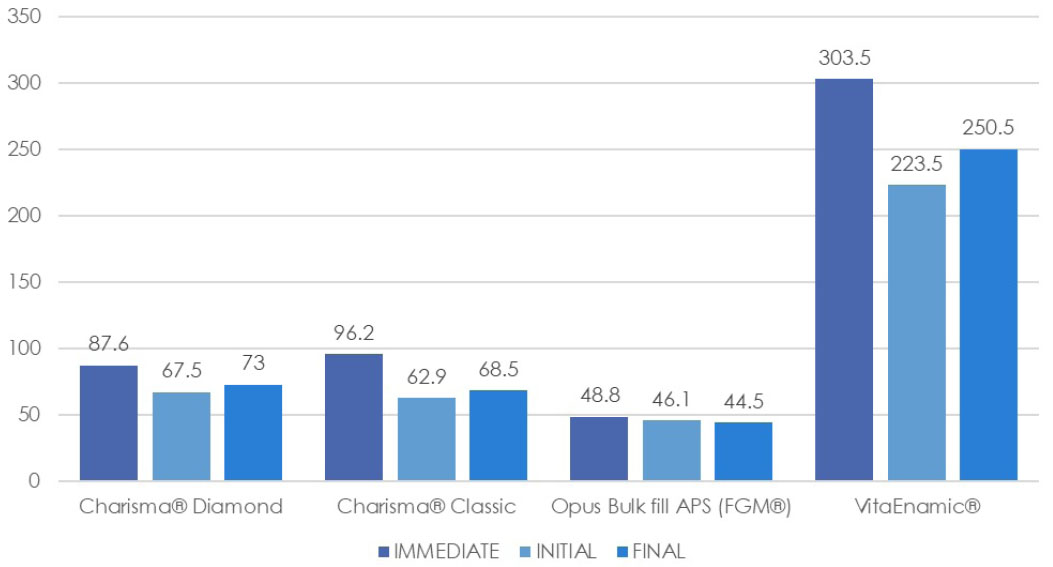
Mean surface micro hardness (MPa) within the control group.
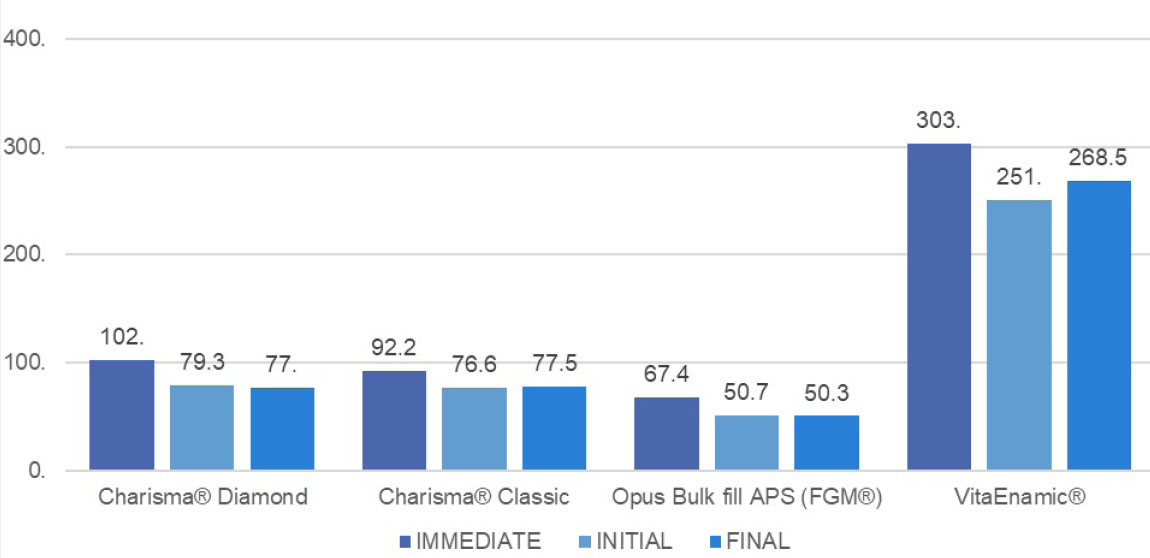
Mean surface microhardness (MPa) within the orange juice group.
| - | Immediate | Initial | Final | |||
|---|---|---|---|---|---|---|
| - | Control | Orange | Control | Orange | Control | Orange |
| Charisma® Diamond | 87.6 ± 23.75 | 102 ± 34.7 | 67.5±16.85 | 79.25 ± 26.77 | 73 ± 17.12 | 77 ± 17.98 |
| Charisma® Classic | 92.2 ± 33.5 | 92.2± 32.2 | 62.9± 22.01 | 76.55 ± 25.98 | 68.5 ± 20.22 | 77.5 ± 14 |
| Opus Bulk fill APS (FGM®) | 48.8 ± 19.5 | 67.4 ± 43.6 | 46.01 ± 14.56 | 50.7 ± 9.77 | 44.5 ± 20.58 | 50.3 ± 18.76 |
| VitaEnamic® | 305.5 ± 184.3 | 303 ± 97 | 223.5± 115.82 | 251± 72.95 | 250.5± 77.28 | 268.5 ± 51.99 |
3.3. Opus Bulk fill APS (FGM®)
After two weeks of immersion in both beverages, the control group exhibited a statistically insignificant decrease (p>0.05) (Fig. 1), in contrast to the significant decrease observed in the orange juice group (p<0.05) (Fig. 2). This indicates that Opus Bulk Fill APS is more affected by the acidic environment.
Following brushing, the reduction in microhardness was minimally exacerbated, with the control group being slightly more affected than the orange juice group.
The overall reduction in hardness was much greater in the orange juice group (p<0.05) compared to the control group (p>0.05) (Table 3), highlighting the material's high vulnerability to acidic conditions.
3.4. Vita Enamic®
Both the control and the orange juice groups displayed high immediate measurements (305.5 ± 184.3 and 303 ± 97, respectively) (Figs. 1 and 2). After the two-week immersion period, both groups showed a significant decrease (p< 0.05), with a more notable reduction in the control group.
After the initial reduction in measurements, both groups experienced an increase in hardness following brushing, with final measurements of (250.5 ± 77.28) for the control group and (268.5 ± 51.99) for the orange juice group (Table 3).
Despite the increase in microhardness after brushing, the final microhardness values were still significantly lower than the immediate values for both groups (p<0.05).
4. DISCUSSION
In this study, the microhardness progression of four different resin restorative materials was investigated to assess their durability and resistance to both chemical and mechanical factors. The results demonstrated that exposure to an acidic environment significantly decreased the microhardness of all tested materials, leading to the rejection of the first null hypothesis. However, brushing did not cause a further significant reduction in micro- hardness; thus, the second null hypothesis was accepted. The four materials exhibited varying responses to the effects of orange juice and brushing, which led to significant differences in their microhardness values. Consequently, the third null hypothesis was rejected.
The significant difference in microhardness values observed in our study after two weeks of immersion in orange juice is consistent with an in-vitro study by Fatima et al. (2013), which reported a significant decrease (P < 0.05) in the microhardness of direct tooth-colored restorative materials after seven days of exposure to both apple and orange juice [12]. Another study has also supported our results, showing significant differences in the microhardness of various materials. These differences were influenced by the immersion solutions used and the distinct compositions of the resin matrices and filler particles in the composite resin materials tested [13]. However, a study by Alencar et al. (2020) presented findings contrary to our results. This in-vitro study examined the effects of extrinsic and intrinsic acids on nanofilled and bulk-fill resin materials and concluded that these materials are resistant to degradation by hydrochloric and citric acids. Their surface roughness and microhardness did not significantly change after a 7-day immersion period [14]. The discrepancies in results across studies on the microhardness of composite materials can be attributed to several methodological differences. Factors such as the chemical composition of the restorative material, the type of immersion solution used, the duration of immersion, and the polishing techniques employed can significantly affect the outcomes [15].
The results of the present study suggest that both micro-hybrid composite (Charisma Classic) and nano-hybrid composite (Charisma Diamond) exhibit similar performance under the same conditions. Both composites experienced a significant reduction in hardness (P<0.05), with the nanohybrid composite showing a slightly greater reduction. Nano hybrid and Micro hybrid composites share many similarities, including the type of resin system, type of filler, and manufacturer. Consistent with our findings, Erdemir et al. (2013) observed that the surface hardness of a nanohybrid composite (Premise) was more significantly reduced than that of a microhybridcomposite (Z250) when exposed to beverages [16]. However, in contrast to these results, Poggio et al. (2018) found that the surface microhardness of a micro hybrid composite (Gradia Direct) decreased more than that of a nanohybrid composite (Admira Fusion) after one week of immersion in beverages [7]. This discrepancy may be attributed to differences in the compositions of the two composites.
Recently developed bulk-fill materials have emerged with the goal of enhancing their properties. Research has demonstrated that their composition, enabling a single insertion of increments, notably reduces polymerization shrinkage, working time, and the number of required clinical steps [17]. However, factors related to compo- sition, such as filler particle mass fractions, size, and distribution, were noted to significantly influence the surface hardness of composite resin restorative materials [18-20]. In the present study, Opus Bulk Fill APS repeatedly displayed the lowest microhardness values, demonstrating a significant difference from the other groups (P<0.05). Similarly, Elsherbeny et al. (2020) conducted an in-vitro study comparing the physical properties and hardness of bulk fill versus incremental composite resin materials. They found that FiltekTM Z350 XT (the incremental type) had the highest hardness values, whereas FiltekTM Bulk-Fill demonstrated lower values [21].
The findings of this research indicate that CAD/CAM resin blocks, such as Vita Enamic, consistently demons- trated the highest microhardness levels across all stages despite the notable decrease after exposure to acidic substances. The elevated microhardness of these blocks can be attributed to their unique combination of ceramic and polymer properties [22]. Previous studies have shown that acids, like those found in cola drinks, can erode the surface microhardness of CAD/CAM materials used in dental restorations. Nevertheless, ceramics still exhibit superior mechanical properties, especially concerning microhardness, compared to resin composites [23].
In the last phase of this in-vitro study, additional microhardness tests were performed on all experimental groups after simulated brushing. The outcomes showed minor fluctuations, with some groups exhibiting slight increases or decreases, but overall, these changes were not statistically significant (P>0.05). This aligns with the conclusions drawn by Çimen et al. (2023) in their prior study, which also found that brushing had no discernible impact on any of the tested groups [24]. Another study by Nima et al. (2021) examined the effects of tooth brushing on different mechanical properties of four esthetic restorative materials. They found that brushing caused surface alterations in all tested materials except for feldspathic ceramic. The changes were more noticeable in resin-based materials. Their results indicated that microhardness did not change significantly after tooth brushing for any of the indirect restorative materials (P > .05), with the exception of one CAD/CAM material, Lava Ultimate (LAV), which showed a significant decrease in microhardness after brushing (P = .002). The study concluded that surface roughness, gloss, and micro- hardness were significantly affected by the material composition, with resin-based materials being more susceptible to surface alterations [25].
CONCLUSION
Based on the findings of this study, the following conclusions were drawn:
1. Overall, all materials experienced a significant decrease in microhardness when immersed in orange juice, which highlights the erosive effects of acidic environments on resin restorative materials.
2. Vita Enamic experienced the most significant decrease in microhardness yet still maintained the highest values overall, indicating strong mechanical properties.
3. Opus Bulk Fill APS showed the lowest values among the tested materials.
4. Charisma Classic exhibited the slightest decrease in hardness values, suggesting good resistance to chemical erosion.
5. Simulated brushing after acid exposure had minimal impact on the results.
Further research is required to explore additional factors that may influence the durability and performance of different restorative materials, with the aim of developing more resilient materials that enhance the longevity of restorations in both functional and aesthetic aspects.
AUTHORS’ CONTRIBUTIONS
K.B.: Study Concept or Design, contributed to the study’s concept and design; Md.S.I.: analyzed the data and interpreted the results; F.A.: contributed to the methodology; A.B., C.S. and Z.E.H.: collected the data; P.P.M. wrote the original draft, and L.R.da S.C. and M.A.: wrote, reviewed and edited the manuscript.
AVAILABILITY OF DATA AND MATERIALS
The data sets used and/or analysed during this study are available from the corresponding author [K.B.] upon request.


