All published articles of this journal are available on ScienceDirect.
Rehabilitation of the Atrophic Maxillary Arch with Tilted Implants Protocol: A Proposed Classification of Various Situations
Abstract
Purpose
The majority of classifications for implant placement are based on the morphology of the available bone. The positions and angulations of implants in all forms of atrophy are not emphasized. Clinicians find it relatively difficult to insert the posterior tilted fixtures such that maximum anchorage of the bone can be obtained for enhanced primary stability, and there is unpredictability since the exit points (implant apex position) of these implants are not known and visualized prior to treatment. The purpose of this article is to classify the entry points, angulations, and exit points for 6 tilted maxillary implants in anterior-posterior distribution for prompt decision-making and ease of surgery as well as to capitalize on the available bone width.
Methods
The retrospective radiographic analysis was performed for 150 maxillary arch edentulous patients restored with fixed prosthesis supported by six tilted implants from April 2021 to April 2023. Post-operative Orthopantomograph (OPG) tracings were performed for maxillary sinus borders to classify the sinus pneumatization, and the entry and exit points of implants were noted with respect to the prosthetic teeth, basal anchoring bone, and implant angulations.
Results
Of the arches treated, 63 were SP1, 34 were SP2, and 16 were SP3 in the maxilla. Many combination arches were encountered as well, including 32 cases of SP1 + SP2 and 5 of SP2 + SP3 combinations. The common preferred entry points were canine, second premolar, and second molar areas.
Conclusions
A functional surgical classification aids in placing all 6 tilted bicortical implants for immediate function while being versatile enough to be used in delayed cases as well. The knowledge of this classification helps to visualize the entry/fixation points, minimizing unpredictable and morbid grafting surgical procedures. It also aids in efficiently delivering patient-centric, minimally-invasive, predictably stable, biomechanically sound, and fixed implant treatments without cantilever in complete edentulism.
1. INTRODUCTION
Dental implants are preferred over other conventional treatment options due to their ability to provide fixed teeth with better functional efficiency. However, despite their increasing popularity for the restoration of single or multiple teeth, full arch rehabilitations can still be challenging because of alveolar bone atrophy associated with tooth loss. This challenge is further exacerbated in the maxilla, which primarily consists of cancellous (porous) bone and undergoes dual resorption in the superior-posterior direction due to tooth loss-related non-use atrophy (according to Wolff’s law) [1] and the pneumatization of the maxillary sinuses [2]. Pneumati- zation is a physiological process occurring in all paranasal sinuses during growth, which causes them to increase in volume [3].
Extensive bone resorption and sinus pneumatization (SP) in many maxillary edentulous cases often preclude the insertion of implants without additional surgical procedures, such as sinus lifts and bone grafts. Literature has proven that tilting the implants parallel to the anterior maxillary sinus wall may represent a feasible treatment option [.4] Long tilted implants (≥ 13 mm) placed in residual bone have been advocated to obtain high levels of initial primary stability, avoiding bone-grafting procedures [5]. Examples of maxillary full-arch implant treatments that do not require sinus lifts and bone grafts include zygomatic implants [6], pterygomaxillary implants combined with zygomatic and conventional implants [7], the Marius bridge for the resorbed edentulous maxilla [8], the “All-on-4” technique with four immediately loaded implants [9], the “13-23-30” anatomic maxillary technique for implant distribution along the alveolar arch [10], the V-II-V technique for immediate placement and loading of implants into an edentulous maxilla without bone grafting [11], treatment of an atrophic maxilla with short implants using an osteotomy procedure [12], the optimal use of anatomic features of the maxillary arch with tilted implants, and others [13, 14].
The decision for selecting the implant technique depends on the amount of available bone, the anatomic factors, and the biomechanical factors of chewing and cantilever forces on the prosthesis. Most of the full arch graftless implant rehabilitation techniques provide a posterior cantilever in the prosthesis, restoring only up to the first molar [6-14]. Other techniques, like ptery- gomaxillary or zygomatic implants, are associated with increased surgical complexity [15].
The TTPHIL: ALL TILT® (Tall Tilted Pin-Hole Immediate Loading) technique is a versatile protocol for all forms of maxillary ridge atrophy, employing six tilted implants for immediate function [16]. In full-mouth cases, superstructures supported by six implants have been found to have a more favorable bone response than those supported by four implants [17]. Further, optimal implant distribution in the anterior-posterior region results in significantly better outcomes compared to implant distribution concentrated in the anterior region [18]. Using anatomical bony features in the posterior regions can result in the restoration of second molars while completely eliminating the cantilever [16].
However, studies have shown that the inability to predict realistic treatment outcomes may lead to several problems during execution, increasing the risk of biological and technical complications, which can result in treatment failure [19]. Additionally, clinicians often find it challenging to insert posterior tilted fixtures in a manner that maximizes bone anchorage for enhanced primary stability [20].
Several authors have developed classifications of sinus pneumatization, focusing on specific aspects—either the anterior, posterior, or vertical dimensions [21-26]. However, treatment planning for implant placement must consider sinus pneumatization in all three dimensions to ensure proper biomechanical and functional outcomes [27-29].
Therefore, the aim of this study is to develop a classification system to simplify the entry points (position of the implant neck), angulations of the implant fixture, directions, and exit points (position of the implant apex) for tilted implants in various scenarios of maxillary bone atrophy. This system aims to bypass vital structures while achieving prosthetically-driven substantial primary stability with minimally invasive surgery, biomechanically sound principles, [30-33] making use of the maximum amount of available bone for immediate loading [34].
2. MATERIALS AND METHODS
2.1. Study Design
The following retrospective radiographic study was conducted according to the principles of the Declaration of Helsinki of 1975, as revised in 2000, and the research protocol was approved by the Institutional Ethics Committee (MADC/IEC/III/86/2023). An analysis of 150 randomly selected subjects with maxillary edentulous arches restored with six dental implants using the TTPHIL: ALL TILT® protocol at the Institute for Dental Implan- tology, Hyderabad, from April 2021 to 2023 was performed. The inclusion criteria were as follows:
1. All patients above 18 years of age.
2. Patients who have undergone maxillary full-arch implant rehabilitation with six tilted implants using the TTPHIL: ALL TILT® protocol.
3. All patients who received immediate prosthetic rehabilitation for a full-arch fixed implant-supported prosthesis no later than 48 hours after the surgery.
Postoperative orthopantomographs (OPGs) were obtained for each patient after the surgical procedure and after the completion of their prosthetic rehabilitation. OPG tracings were done to outline the maxillary sinus borders, classify the sinus pneumatization, and note the entry and exit points of implants in relation to the prosthetic teeth, basal anchoring bone, and implant angulations. A classification was then developed based on the obtained information and subjected to descriptive statistical analysis.
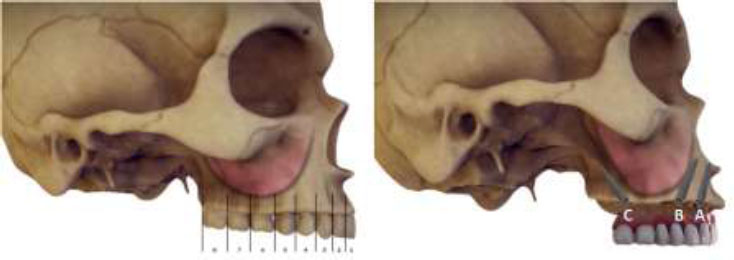
Site classification according to the teeth segments and numbering of the implants.
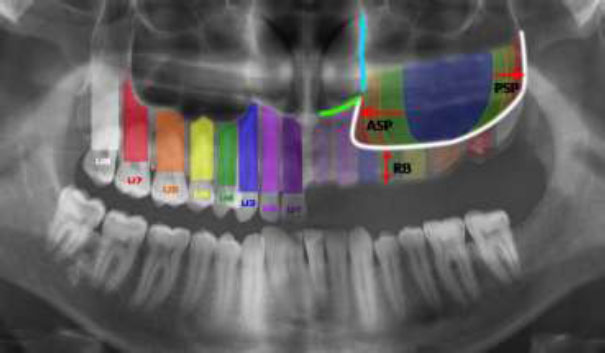
Pneumatization of maxillary sinus along the anterior border (ASP), posterior border (PSP), and supero-inferior direction remaining bone height (RB).
2.2. Site Classification
The sagittal section of the maxilla was divided into eight segments, modelled on the FDI tooth numbering system, with each segment numbered from 1 to 8 in a mesial-to-distal direction corresponding to the tooth numbers. Three tilted implants were placed on each side (right and left) of the maxilla, numbered from anterior to posterior as A, B, and C within the sagittal maxillary segments (Fig. 1). The entry and exit points of the implants were determined based on the anatomical limiting structures of the maxillary sinus.
The maxillary sinus pneumatization was considered from the anterior aspect, posterior aspect, and the supero-inferior aspect (Fig. 2).
The pneumatization of the sinus along its anterior border (ASP) was classified according to Tolstunav et al. [21, 22] as the distance of the anterior wall of the sinus from the midline into SP0 (>30 mm), SP1 (>25 mm), SP2 (21-25 mm), SP3 (16-20 mm), SP4 (<15 mm).
For pterygoid implants, Luis et al. [23, 24] proposed the classification of diagnostic prediction PARP (Pterygoid Anatomic Radiographic Prediction), which was used for posterior pneumatization extent of the maxillary sinus (PSP). It was based on the extent of maxillary sinus invasion and the consequently available width of bone in the pterygoid region, categorized as PARP 1 (>15 mm), PARP 2 (11-15 mm), PARP 3 (5-10 mm) and PARP 4 (<5 mm).
The inferior pneumatization of the sinus towards the alveolar ridge was classified according to Misch's subantral classification of remaining bone (RB) as RB 1 (>10 mm), RB 2 (5-9 mm), and RB 3 (<5 mm) [25, 26]. This was measured as the distance from the inferior border of the maxillary sinus to the alveolar ridge crest.
Utilizing these three classifications, the availability of bone in relation to the maxillary sinus was determined, which is a key factor in the decision-making. The ideal implant placement sites were considered to be 3-5-7 (canine region- second premolar- second molar) on either side of the midline for appropriate antero-posterior spread (AP spread) and elimination of cantilever. A minimum of 5 mm of supero-inferior bone height was desired at the proposed entry point of implant, an otherwise alternate entry point was used.
The TTPHIL: ALL TILT® protocol implants were used for immediate loading, therefore, achieving basal cortical anchorage was crucial. This was determined based on the extent of sinus pneumatization, which guided the selection of bone for anchorage and the angulation for the implant's exit point. A minimum implant length of 16 mm was used to ensure optimum Bone-Implant Contact (BIC), which further influenced the exit point of the proposed implant.
The major bones utilized for basal anchorage and exit points are as follows: the Nasal Floor (NF) for the anteriors; the Nasal Floor (NF) and the Lateral Wall of the Nose (LWN) for premolars; and the Pyramidal Process of the Palatine bone (PPP) for molars. If the residual alveolar bone height is less than 16 mm from the ridge crest to the planned basal bone, the entry point can be adjusted, and basal anchorage can be achieved from the Vomer (V) for anteriors, the Naso-Maxillary Buttress (NMB) and Zygomatic bone (Z) for premolars, and the medial pterygoid plate (MPP) and zygomatic bone (Z), with or without a Trans-Sinus (TS) implant, for the molars.
3. RESULTS
Radiographic data from 150 maxillary edentulous arches, consecutively treated with six tilted implants for immediate function between April 2021 and April 2023, were used for classification. Each arch had at least one year of follow-up and was classified based on the tilted implant site. All patients received six implants (Bioline I, Bioline Dental GmbH & Co. KG, Berlin, Germany), placed into immediate function within two days post-surgery. Of the treated arches, 63 were classified as SP1, 34 as SP2, and 16 as SP3 in the maxilla. Additionally, several combination arches were encountered, including 32 cases of SP1 + SP2 and 5 cases of SP2 + SP3 combinations. There were no surgical or prosthetic complications reported during the tenure of the study. This short-term retrospective analysis revealed that all arches could be rehabilitated to immediate function without grafting or sinus lifts while engaging basal cortical bone, with each implant exhibiting a minimum insertion torque of 50 Ncm. Furthermore, all patients received first and second molar occlusion without cantilevers, thus enhancing bio- mechanical stability. The primary focus of this classification is the prosthetic ability to load a transitional immediate prosthesis without any augmentation, using the TTPHIL ALL TILT® technique. This approach completely eliminates the posterior cantilever in complete edentulous maxillary arches.
3.1. Decision-making for Sinus Pneumatization
The anterior, posterior, and inferior extents of sinus pneumatization were assessed to determine the possible options for implant entry and exit. The authors identified eight different scenarios that could accommodate most permutations and combinations of maxillary sinus pneumatization (Tables 1 and 2).
| - | PARP1 no bone invasion |
PARP2 sinus invasion but bone(y=) > 10mm |
PARP3 sinus invasion but bone between (y=) 5-9mm (till 2nd molar) |
PARP4 sinus invasion bone (y=) < 5mm (till 8) |
|---|---|---|---|---|
|
SP0 X= Greater than 30mm (no pneumatization) |
Situation 1 | Situation 5 | ||
|
SP1 X= Greater than 25 mm (till 2ndpre-molar) |
||||
|
SP2 X=21-25mm (till 1st pre-molar) |
Situation 2 | Situation 6 | ||
|
SP3 X=16-20mm (till canine) |
Situation 3 | Situation 7 | ||
| SP4 X=Less than 15mm (extreme) |
Situation 4 | Situation 8 | ||
| Situation No. | Entry points | Exit points | Alternate option when RB<5mm at the preferred site | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Implant A | Implant B | Implant C | ||
| 1 | - | - | √ | - | √ | - | √ | - | NF | NF | PPP | 2NF - 5NF- 7PPP |
| 2 | - | √ | - | √ | - | - | √ | - | NF/V | NF | PPP | 1NF - 4NF- 7PPP |
| 3 | - | - | √ | - | √ | - | √ | - | NF/V | Z | PPP | 2V - 5Z - 7PPP |
| 4 | - | √ | - | √ | - | - | √ | - | NF/V | Z | PPP | 3Z - 5Z- 7PPP |
| 5 | - | - | √ | - | √ | - | - | √ | NF | LWN/NF | PPP/TS | 2NF - 5LWN - 8PPP |
| 6 | - | √ | - | √ | - | - | √ | √ | NF | NF/Z | TS/PPP | 3NF - 5Z - 7TS - 8PPP |
| 7 | - | - | √ | - | √ | - | - | √ | NF/V | Z | PPP/TS | 2NF- 5Z - 7TS - 8PPP |
| 8 | - | √ | - | √ | - | - | √ | √ | NF/V | Z | PPP/TS/MPP | 3NF - 5Z - 7TS - 8PPP or Quad Zygoma |
3.1.1. Situation 1
If the distance between the anterior extent of sinus pneumatization and midline exceeds >25mm i.e. SP1 or SP 0, along with minimal or no posterior pneumatization, then the point of entry of implant B is segment 5. Segment 3 is used for implant A, and segment 7 for implant C. (Fig. 2) . If RB in segment 3 is less than 5 mm, then the anterior implant can be shifted to segment 2 to engage the vomer. In rare cases, it might be necessary to put an implant in segment 1 while engaging the nasal floor. The implants are angulated disto-mesially, bucco-palatally, and axially, with angulations ranging between 15-450 exiting at the medial wall of the maxillary sinus / lateral wall of the nose (Fig. 3).
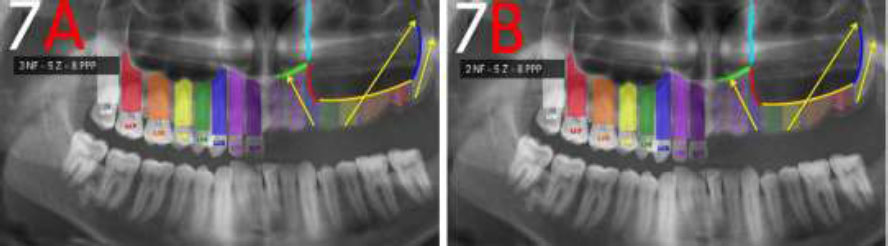
Variations: 1A: 3 NF - 5 NF - 7 PPP, 1B: 2 NF - 5 NF - 7 PPP, 1C: 2 V - 5 NF - 7 PPP, 1D: 2 P - 5 NF - 7 PPP, 1E: 1 NF - 5 NF - 7 PP
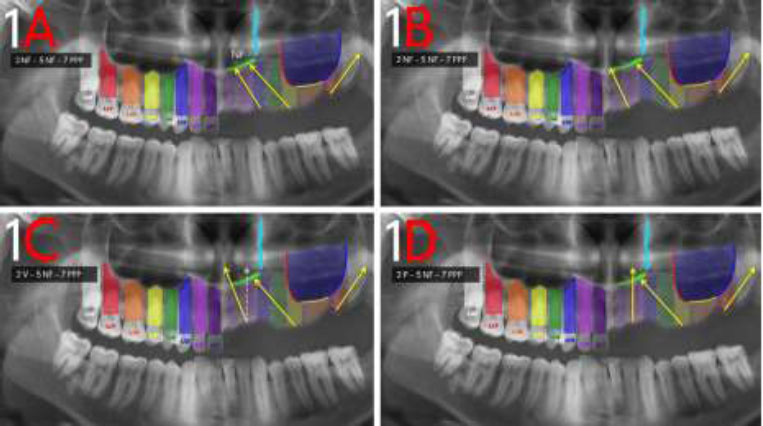
Possibilities of situation 1 with SP0 or SP1 and PARP1 or PARP2.
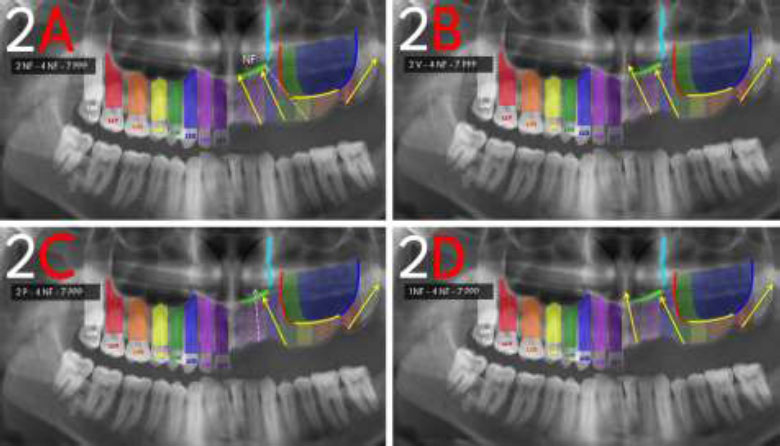
Possibilities of situation 2 with SP2 and PARP1 or PARP2.
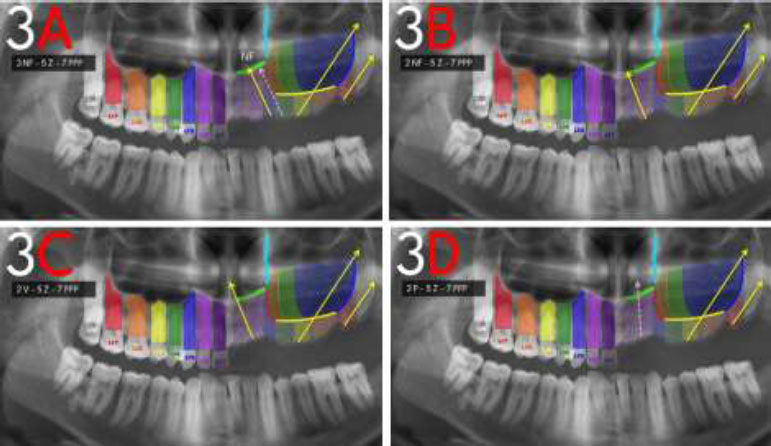
Possibilities of situation 3 with SP3 and PARP1 or PARP2.
3.1.2. Situation 2
If the anterior extent of sinus pneumatization and midline ranges between 21-25mm, i.e SP2, with minimal or no PSP, segment 5 does not have the required RB, then segment 4 becomes the point of entry for implant B, segment 2 for implant A and implant C is the same as in situation 1. If RB is less for segment 2, the exit point can be changed to vomer through the same entry, or segment 1 can be used to engage the nasal floor. The implant angulations are similar to situation 1 (Fig. 4).
3.1.3. Situation 3
In the event of the distance between the anterior extent of sinus pneumatization and midline ranging between 16-20 mm i.e. SP3, with minimal or no PSP, implying no bone in segments 4 and 5, engagement of zygomatic cortical bone is necessary with a point of entry being segment 5. The implants are angulated mesio-distally, engaging the cortical zygoma, which becomes the exit point of implant B. The anterior implant A and posterior implant C are placed similarly to situations 1 and 2 (Fig. 5).
3.1.4. Situation 4
When the distance between the extent of sinus pneumatisation and the midline is less than 15mm, i.e., SP 4, with minimal or no PSP, for anterior implant A entry point segment will be 2, implant B will be a zygomatic implant with an entry point at segment 5 and implant C is the same as in previous situations. Implant A is directed disto-mesially and bucco-palatally with angulations ranging between 9-300 exiting at the floor of the nasal cavity. In some cases where RB is very low, a quad zygoma approach can be used with implants A and B, and the angulation for implant A becomes similar to B (Fig. 6).
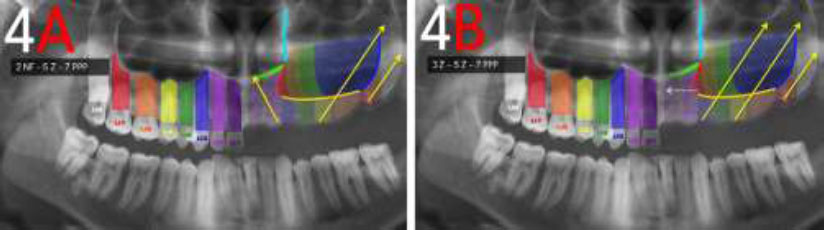
Possibilities of situation 4 with SP4 and PARP1 or PARP2.
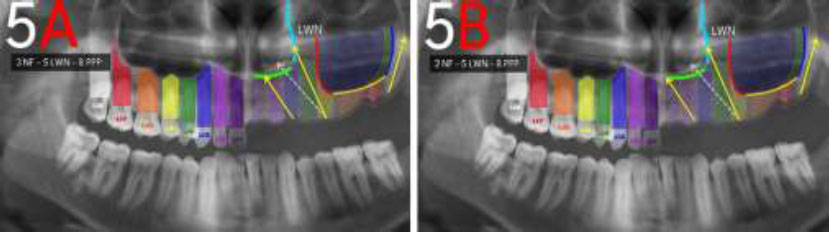
Possibilities of situation 5 with SP0 or SP1 and PARP3 or PARP4.
3.1.5. Situation 5
In the event of pneumatisation extending posteriorly, for implant C, the limiting structure is the junction between the posterior wall and floor of the maxillary sinus. Implying the 3mm bone height availability in the distal maxilla, implant C would enter through segment 7. In addition, a trans-sinus pterygoid implant with a segment 7 entry point is another feasible option for implant C. For implants A and B, the placement can be planned as per situation 1 since ASP is minimal. All implants are directed mesio-distally, bucco-palatally following an angulation ranging between 30-600 degrees in the sagittal section and 15–250 in the axial section to exit at the pterygoid cortex depending on the degree of maxillary tuberosity resorption and sinus pneumatization (Fig. 7).
In the event of pneumatization extending posteriorly, segment 8 becomes the point of entry as long as Misch's rule of two pontics is followed, whereby the adjacent implant could have an entry point at segment 5 [27]. If this possibility is limited by the absence of bone in segment 5, a zygomatic implant has to be introduced.
3.1.6. Situation 6
With moderate ASP and extreme PSP, the preferred configuration for optimum implant and prosthetic support and stability is achieved through an additional trans-sinus implant in segment 7 exiting at the medial pterygoid plate (MPP). The implants A, B and C are similar to those in situation 5 (Fig. 8).
3.1.7. Situations 7 and 8
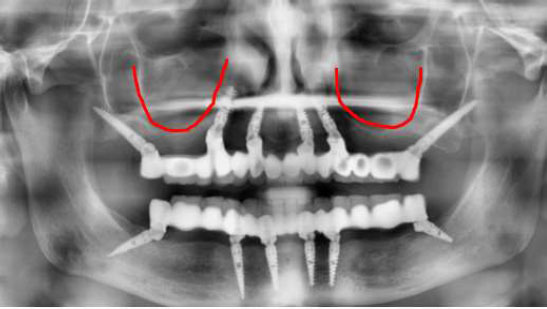
ASP precludes anchorage from anterior anatomic landmarks, and hence, zygomatic anchorage is received from implant B in such situations. For implant A, segments 2 or 3 can be used as is available from the clinical situation. Implant C is similar to situation 6. In the absence of available bone height in Segment 1,2,3,4,5,6, use of pterygoid implants with entry points in Segment 7, and two zygomatic implants with entry points in Segments 3 and 5 on each side of the maxilla can be used for complete fixed rehabilitation. For cases presenting with extreme sinus pneumatization from all three aspects of anterior, posterior, and inferior, a quad zygoma approach may be utilized (Figs. 9 and 10).
3.2. Clinical Application
This classification has been devised for clinical decision-making after assessing sinus pneumatization. The authors propose classifying sinus pneumatization from the anterior and posterior aspects to identify the specific situation of each case. Subsequently, the vertical height of the sinus should be measured to further subclassify based on the current findings. Below are cases where the anterior pneumatization of the sinus is at different levels, and the corresponding situations have been used (Figs. 11-13).
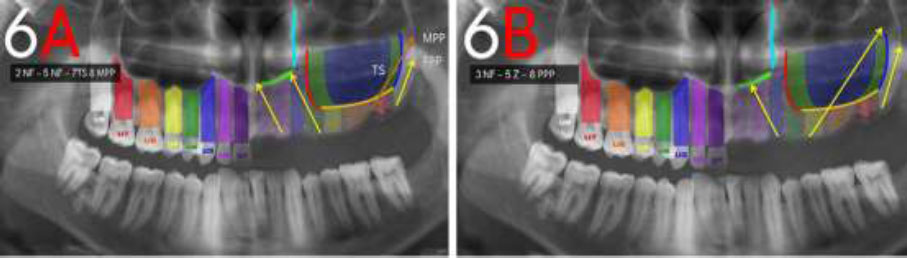
Possibilities of situation 6 with SP2 and PARP3 or PARP4.
Possibilities of situation 7 with SP3 and PARP3 or PARP4.
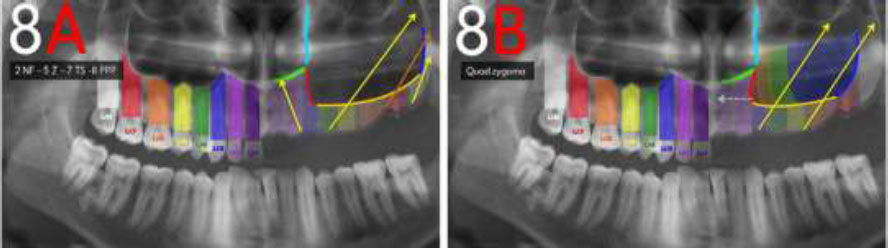
Possibilities of situation 8 with SP4 and PARP3 or PARP4.

Clinical case depicting sinus pneumatization for Situation 1 and its corresponding entry and exit points of implants as 3NF-5NF-7PPP.
4. DISCUSSION
Presurgical treatment planning is imperative for the successful outcome of implant therapy. A classification that embraces all forms of atrophy with immediate function in mind is proposed throughout this study. All traditional classifications in implantology are circum- scribed by morphology and availability of bone. They fail to focus on the implant placement areas that encompass the entry and fixation/exit points. This retrospective study has helped devise a type of classification that holds ground, as it can guide even an inexperienced implantologist in implant placement. With the rise of many full-arch implant rehabilitations, a prompt classification of fixture entry and exit points can contribute to the ease of treatment planning and surgical technique. Even if maxillary sinus pneumatization is not the same bilaterally in any patient, a combination of two different situations from this classification can be conveniently applied to each case.
Clinical case depicting sinus pneumatization for Situation 2 and its corresponding entry and exit points of implants as 2NF-4NF-7PPP.

Clinical case depicting sinus pneumatization for Situation 3 and its corresponding entry and exit points of implants as 3NF-5Z-7PPP.
The proposed classification of situations is based on the key rules established by Misch [28]. The implants used for full-arch rehabilitation are placed in all key zones of the arch, including anteriors, premolars, and molars. The entry points are such that no more than three adjacent pontics are designed between two implants, thus eliminating the increased flexural strength that can cause screw loosening, prosthesis fracture, or even implant failure in the long run [28]. The Canine-Molar rule is followed, with the first preference for implant entry points in the anterior region being the canine on both sides. Posterior molars are used for implant placement to completely eliminate the cantilever on the prosthesis while restoring the occlusion up to the second molars [29].
The TTPHIL: ALL TILT® protocol is aimed at simplifying the implant surgical procedure, making it prosthetically driven and minimally invasive to achieve predictable primary stability for immediate loading while avoiding grafting procedures through the bypassing of vital structures [23, 29]. These tilted implants permit the placement of longer fixtures in the residual bone, which increases the surface area of bone-to-implant contact (BIC) and allows for the achievement of high torques by providing anchorage to more than one cortical plate.4 The sharp engagement of the implant apex with the basal bone reduces micromovement, so even when trans-sinus implants are used, the implant apex does not protrude into the sinus cavity. Other benefits include the elimination of cantilever length, stress reduction in both cancellous and cortical bone, and better distribution of occlusal forces [4]. This tilted implant configuration also provides better anterior-posterior stress distribution, which prevents angulated torque moments on the implants that frequently result in resorption of the cortical bone around the distal implant neck [30].
The TTPHIL: ALL TILT® technique recommends a single-drill osteotomy, which decreases time and heat to the bone tissue and enables the under-preparation of the implant bed site, thus increasing implant stability[.31] Immediate loading with platform-switched, micro-grooved abutments after the single-stage surgery reduces horizontal bone remodeling around the subcrestally placed implants [32]. Baggi et al. [33] found that the platform-switching concept, along with subcrestal positioning, demonstrates better stress distribution in bone and a lower risk of bone overload.
With the use of six tilted implants for severe atrophic jaw rehabilitations becoming the norm due to its biological and biomechanical advantages [34], it is pertinent to provide an implant entry/exit point classification that acknowledges anatomical limitations and anterior-posterior implant spread. Further studies with a larger sample size and the use of three-dimensional radiographic imaging, such as CBCT, are required to substantiate these findings. Proper knowledge and prompt decision-making for planning implants in atrophic arches can help the clinician minimize human error and achieve predictable results.
CONCLUSION
The advantage of tilting implants is to promote the optimal use of available bone. This functional surgical classification, derived from the retrospective data of patients with a minimum one-year follow-up period, facilitates the placement of six tilted bicortical implants for immediate function and is adaptable for use in delayed cases as well. It was concluded that atrophic maxillary arches could be rehabilitated to immediate function without grafting or sinus lifts while engaging basal cortical bone and achieving high primary stability. The approach used by the authors enables the provision of patient-centered treatments that are predictably stable, biomechanically sound, and fixed, eliminating cantilever effects in cases of complete edentulism.
AUTHORS' CONTRIBUTIONS
V., M.: Conceptualization; V., S., B., M. Formal Analyses; V., S., B.: Investigation; Dr. Venkat, S., B., M.: Methodology; V., S., B., M.: Project Administration; V., B.: Writing – Original Draft; V., S., B., M.: Writing – Review & Editing.
LIST OF ABBREVIATIONS
| PARP | = Pterygoid Anatomic Radiographic Prediction |
| NF | = Nasal Floor |
| PPP | = Pyramidal Process of the Palatine bone |
| BIC | = Bone-Implant Contact |
| LWN | = Lateral Wall of the Nose |
| V | = Vomer |
| NMB | = Naso-Maxillary Buttress |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The research protocol was approved by the Meenakshi Academy of Higher Education and Research, Chennai, India (MADC/IEC/III/86/2023).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2000.
CONSENT FOR PUBLICATION
This is a reterospective study and does not include any identifying information of any patient.


