All published articles of this journal are available on ScienceDirect.
A Case Report on an Uncommon Complication Following the Extraction of Maxillary Molars: A Subconjunctival Hemorrhage
Abstract
Background
This case report presents a complication, subconjunctival hemorrhage, after extraction of maxillary first and second molar residual roots. This is a very rare complication, with only four reported cases of sub-conjunctival hemorrhage in the literature.
Case Presentation
In this case report, a 62-year-old woman who had an extraction of maxillary first and second molar residual roots developed sub-conjunctival hemorrhage the day after the extraction. The condition was asymptomatic, and the hemorrhage dispersed in five days without any medical intervention except regular monitoring.
Conclusion
Clinicians should keep this rare complication in mind and take necessary precautions during local anesthesia and extraction.
Practical Implications
Clinicians should consider the possibility of this post-operative complication and perform surgical procedures with the utmost care, starting from aspiration during local anesthetic injection to post-surgical management of the area to prevent hemorrhage.
1. INTRODUCTION
Subconjunctival hemorrhage or ecchymosis is a frequently occurring non-threatening eye condition with distinct characteristics. It is marked by the sudden and painless onset of well-defined redness caused by bleeding beneath the conjunctiva [1]. This condition is usually asymptomatic, and affected individuals may not be aware until they look in the mirror [2]. The most common causes of subconjunctival hemorrhage are straining, coughing, sneezing, trauma, and rubbing eyes very hard. Other less common reasons include diabetes, high blood pressure, and anti-coagulant therapy. This condition usually resolves on its own within a few days to weeks, depending on the size of the hemorrhagic spot [2].
Tooth extraction, especially maxillary third molar, is also a cause of subconjunctival hemorrhage in very rare instances. In the available literature, only four reported incidents of subconjunctival hemorrhage as a post-extraction complication are documented [3-6]. In all these reported cases, the condition was entirely asymptomatic and resolved within five days to two weeks.
In this report, we present the case of a 62-year-old woman who developed the rare complication of sub- conjunctival hemorrhage after extractions. The patient had an uneventful extraction of maxillary first and second molar residual roots and developed asymptomatic subconjunctival hemorrhage the next day. This case report followed CARE guidelines [7].
2. CASE REPRESENTATION
On November 9th, 2023, a 62-year-old woman presented to our clinic for a limited evaluation, complaining of broken teeth on the maxillary arch. The patient reported no symptoms during the appointment.
The medical history of the patient was significant for depression, type II diabetes mellitus, and hypertension. She was under regular medical care for these conditions and reported taking the following medications: Janumet 100/1000 (2 caps per day), Bisoprolol HCTZ (2 tabs per day), Trazodone 100 mg (1 tab per day), Sertraline 50 mg (1 tab per day), and Topiramate 25 mg (1 tab per day). The patient had no history of smoking or drug use. The recent HbA1C was 6.4, and her blood pressure during the appointment was 137/85 mmHg.
The clinical examination revealed shallow residual roots #1, 2, and #16 with no symptoms. Other findings included carious lesions, existing restorations, previous endodontically treated teeth, and missing teeth. Addi- tionally, bilateral lingual tori were present on the mandible. The patient was presented with a compre- hensive treatment plan, including the extraction of residual roots (Fig. 1), restoration of carious lesions, and replacement of missing teeth. The patient agreed to the treatment plan and presented for the extraction of teeth #1 and #2 on November 27th, 2023. There were no contraindications to the extraction.
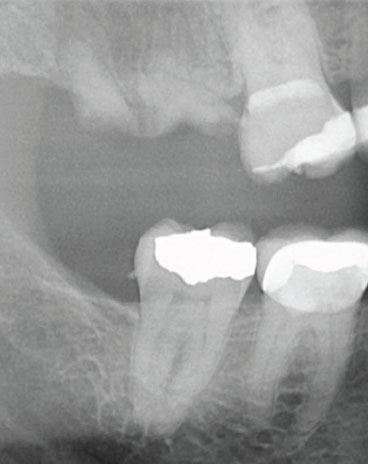
Pre-operative x-ray.
Local anesthesia was achieved with 1.5 capsules of 4% Articaine with 1:100,000 epinephrine through buccal infiltration and a right greater palatine nerve block. After objectively testing for adequate anesthesia, a periosteal elevator was used to reflect the gingiva around the root tips. After sufficient reflection of the gingiva, a 301 straight elevator was used to extract the root pieces. The sockets were gently curetted and irrigated with saline. A 3.0 chromic gut suture was used to approximate the socket margins using a single interrupted suture. Hemostasis was achieved, and the patient was instructed to bite on a gauze piece. The whole procedure was uneventful, and the patient was dismissed in good condition.
On November 30th, 2023, the patient presented for a hygiene appointment and exhibited red spots in the right eye (Fig. 2). The patient mentioned developing bright red spots in the eye the day after extraction and reported no discomfort or blurry vision. Upon examination, the extraction area was healing without any complications, and no other extraoral swelling was observed. With the extraction of the residual roots being uneventful, a tuberosity fracture was ruled out, and a CBCT was not recommended.

Photograph showing sub-conjunctival hemorrhage.
The patient was advised to visit her ophthalmologist for an evaluation and scheduled a follow-up visit after five days. The patient presented for a follow-up appointment on December 4th, 2023, showing a marked reduction in the size of the red spot (Fig. 3). The patient mentioned that she could not secure even a virtual appointment with her ophthalmologist. Consequently, the patient went to urgent care for an evaluation and was told that they could not do anything for her. The redness in the eye resolved completely after ten days without any medical inter- vention. The patient had no subjective or objective symptoms throughout the time period. No ethical clearance was obtained as it does not involve any intervention.

Photograph showing resolution of sub-conjunctival hemorrhage.
3. DISCUSSION
This case report presents a very rare complication of subconjunctival hemorrhage after the extraction of maxillary first and second molar residual roots. The condition was completely asymptomatic, and the hemor- rhagic spot diminished significantly in size after five days.
Complications associated with maxillary molar extraction include oro-antral communication, displacement of roots into the sinus, alveolar fracture, maxillary tuberosity fracture, subconjunctival hemorrhage, and retrobulbar hematoma [8]. Sub-conjunctival hemorrhage is a very rare complication after extraction of maxillary third molars. In the majority of previously reported cases, subconjunctival hemorrhage after maxillary molar extraction occurred secondary to tuberosity fracture. In contrast, a case report by Dhiman et al. [4] presented a case of subconjunctival ecchymosis after the extraction of a maxillary canine.
The fracture of the tuberosity offers an explanation for the hemorrhage pathway, where the rupture of blood vessels in proximity to tuberosity, pterygoid plexus, and posterior superior alveolar arteries causes bleeding into pterygomaxillary and infra-temporal spaces. These spaces communicate with the orbital compartment through an infraorbital fissure. This communication can cause bleeding in the infra-temporal region to end up in the form of subconjunctival hemorrhage. Previous case reports also mentioned the possibility of damage to the pterygoid plexus during local anesthetic injections and subsequent hemorrhage ending up in the orbit. Another explanation provided in the literature [3] was the seepage of blood from the maxillary molar extraction site into the infra-temporal space and ultimately into the orbit. All the abovementioned reasons, including tuberosity fracture, flap reflection, and local anesthetic injection, could cause blood leaks into the fascial spaces, which can ultimately enter the orbital space through inferior orbital fissures. Fig. (4) illustrates the proximity of the inferior orbital fissure to the maxillary posterior teeth. Another rare complication of maxillary third molar extraction is retrobulbar hematoma. While this condition has the same causal pathway as subconjunctival hemorrhage, the implications are severe, including loss of vision. There are only three reported cases of retrobulbar hematoma after uneventful extraction of maxillary third molars.

Diagram showing inferior orbital fissure (source: IMAIOS).
There is no standard treatment protocol for subconjunctival hemorrhage. In the previously published reports [1, 3-6], three cases were managed with antibiotic eye drops and benzalkonium chloride, and one case was just followed up without any medical intervention. The patient, in this case report, received no medical intervention due to lack of access to care, and the hemorrhagic spot diminished significantly in size after five days. Even though the hemorrhagic spot faded by itself, appropriate evaluation and management by an ophthalmologist is recommended to avoid any complications.
The incidence of bleeding, intra and post-operative, after third molar extraction ranges from 0.2% to 5.8% [9]. This hemorrhage is more common after extraction of mandibular third molars than maxillary third molars. The maxillary third molar is in close proximity to important anatomical structures, including the pterygoid plexus, posterior superior alveolar artery, and deep facial vein. Damage to these vessels can cause complications ranging from minor subconjunctival hemorrhage to debilitating retrobulbar hemorrhage [10-12].
In this present case, the reason for subconjunctival hemorrhage is unclear. The extraction of the residual root tips was minimally invasive and atraumatic. During local anesthesia, the initial aspiration was negative, which ruled out the intra-arterial injection of lidocaine. Uckan et al. [12] reported that there is a possibility of intra-arterial injections even after locating anatomical landmarks and negative aspiration before injecting a local anesthetic. In people aged 50 and over, systemic conditions, such as hypertension and diabetes mellitus, are risk factors for subconjunctival hemorrhage [1]. This patient had both conditions; however, they are well-controlled with medication, and the patient had no history of spontaneous subconjunctival hemorrhage. The idiopathic nature of this condition will make it hard for it to be attributed to any particular etiology.
CONCLUSION
In summary, this case report highlights a rare occurrence of subconjunctival hemorrhage after the extraction of residual roots from the maxillary first and second molars. The hemorrhagic spot resolved spon- taneously without any medical intervention within five days.
AUTHORS’ CONTRIBUTION
S.M. and A.K.: Contributed to the conception and design of the study; S.M.: Collected the data; S.M., A.K., and H.R.: Carried out the analysis and interpretation of the results; S.M., A.K., and H.R.: Drafted the manuscript.


