All published articles of this journal are available on ScienceDirect.
Piecemeal Resection of a Large Complex Odontoma Obstructing Upper Canine Eruption: A Case Report
Abstract
Background
Odontomas are the most common odontogenic tumors that affect the oral cavity. They are asymptomatic bony lesions that vary in size and often lead to impaction or delayed eruption of associated teeth. The purpose of this study was to report a case of a large complex odontoma causing impaction of the maxillary left permanent canine with persistent pain, which was treated by piecemeal resection.
Case Presentation
A 32-year-old female reported persistent symptoms of pain and pressure on the left side of her face. Clinical examination revealed a small hard growth in the left canine region of the maxilla associated with an impacted permanent canine. Radiograph examination revealed a homogenous mass of calcified material lying just coronal to the impacted canine with similar radiodensity to the tooth structure and surrounded by a thin radiolucent rim, suggestive of an odontoma. The odontoma was accessed under local anesthesia via an intraoral approach and was surgically excised for future eruption of the impacted permanent canine.
Conclusion
Conservative surgical removal of odontomas is straightforward, but requires careful attention if the impacted tooth undergoes further orthodontic treatment. Early diagnosis and management are crucial to prevent eruption disturbances and cyst formation. The prognosis is generally good, and surgical excision is a reliable treatment.
1. INTRODUCTION
Odontomas are hamartomatous developmental malformations emerging from completely differentiated epithelial and mesenchymal cells fostering ameloblasts and odontoblasts activity. They are fundamentally charac- terized by their non-aggressive slowly growing nature and formed by the overgrowth of dental tissues including enamel, dentin, pulp, and cementum in variable amounts [1]. WHO further classified odontomas into compound odontomas with dental malformations organized anatomically similar to the tooth structure and complex odontomas with disorganized dental malformations lacking the resemblance to the anatomical tooth structure [2]. Odontomas are the most common odontogenic tumors and are frequently discovered incidentally during routine radiological examination because they are asymptomatic pathologies. However, some clinical signs, such as bony expansion, teeth displacement, retention of teeth, or delayed eruption, might speculate the presence of odontomas [3]. The etiology of odontomas remains unknown. However, it could be attributed to trauma, infections, and genetic mutations as it showed an association with Gardner’s syndrome, Hermann's syndrome, and basal cell nevus syndrome [1].
This report has introduced a case of a complex odontoma associated with an impacted upper canine. The study has focused on surgical intervention, highlighting the challenges associated with multiple problems encountered with this odontoma.
2. CASE PRESENTATION
A 32-year-old female patient reported to the oral surgery clinic of the University Dental Hospital of Sharjah (UDHS). The patient complained of pressure and severe unspecified pain, which resulted in a score of six on the Visual Analog Scale (VAS) in the left anterior region of the maxilla, as well as the left maxillary sinus and the orbital region. The pain onset was in conjunction with the menstrual cycle and associated with nausea and photophobia. The symptoms of the chief complaint started ten years ago. However, the patient consulted an Ear, Nose, and Throat (ENT) specialist five years after the onset of symptoms. The ENT specialist referred the patient to a general dentist, who referred her to an oral medicine specialist and, finally, she was referred to an oral surgeon. The patient visited the oral surgery teaching clinic at UDHS in 2023. Medical history was non-remarkable. Family history revealed a history of migraines paternally and hypertension maternally. The patient has been smoking water pipe for ten years at an average of an hour per day. Upon extraoral examination, no abnormalities were detected. Intraoral examination revealed a hard swelling in the labial cortical plate at the depth of the vestibule of the tooth's permanent upper left canine region, with no tenderness to palpation.
Panoramic radiograph and Cone Beam Computed Tomography (CBCT) exhibited a well-defined multiple homogenous radiopaque mass similar in density to tooth structure, surrounded by a thin radiolucent rim, on the path of eruption of an impacted permanent upper left canine. The CBCT was performed in order to determine the location of the mass, its relationship to the impacted permanent upper left canine, as well as the relationship between the impacted permanent upper left canine and the maxillary sinus and nasal cavity. The maximum dimensions of the mass were 11.68 mm, 14.09 mm, and 12.34 mm in the anterior-posterior direction, mediolateral direction, and superior-inferior direction, respectively. The impacted permanent upper left canine did not erode the walls of either the sinus cavity or the nasal cavity (Fig. 1). The coronal CT section of the left maxillary sinus showed almost full radio-opacification, with circumferential mucosal thickening (Fig. 2). On the basis of the clinical and radiographic examinations, a complex odontoma and chronic maxillary sinusitis have been diagnosed. Consequently, the treatment plan consisted of removing the odontoma while preserving the canine. This procedure was performed by a senior master's student at UDHS under the supervision of a maxillofacial surgeon. The surgical procedure was carried out under local anesthesia using labial and palatal infiltration with two anesthetic cartridges (2% Lidocaine with epinephrine 1:80,000). To gain intraoral access, a two-sided flap was raised with a sulcular incision from the upper left lateral incisor to the upper left second premolar, and one vertical release incision mesial to the upper left lateral incisor. Following the elevation of the full-thickness mucoperiosteal flap (Fig. 3), an osteotomy was performed to enable a clear view of the canine and the odontoma. A surgical round bur and chisel and mallet were used to perform piecemeal resection of the odontoma. During the removal of the fragments, care was taken to avoid damaging the impacted canine and alveolar bones, as well as to ensure that the fragments were removed completely. After total removal of the odontoma, the wound was irrigated with saline, and the incision was closed by simple interrupted suturing using a 4:0 non-resorbable nylon suture. Post-operative instructions had been given along with prescribing amoxicillin 500mg and ibuprofen 400mg, both three times a day for 5 days.
A periodic follow-up was planned two weeks following surgery, during which the patient reported no postoperative complications. An intraoral examination revealed no evidence of edema or hematoma formation. Four months following surgery, the VAS score decreased from six to four and the sensation of pressure has almost disappeared. CBCT imaging was performed eight months after surgery and it revealed no spontaneous eruption or movement of the impacted canine. Additionally, there was a relatively clearer left maxillary sinus (Fig. 2).
3. DISCUSSION
Odontomas are the most common odontogenic tumors. They are composed of odontogenic epithelium, ectomesenchyme, and dental tissue formation. The majority of them are associated with children and young adults, with a peak incidence in the second decade of life and no associated gender predilection [4]. Complex odontomas have a higher incidence in the posterior of the mandible compared to compound odontomas, which are more commonly present in the anterior maxilla. The morphology of the odontoma relies on the age of the lesion, as it shows more like a developing tooth in early lesions, unlike older lesions where the presence of tubular dentin and enamel matrix, and occasionally, traces of cementum are found [3].
Odontomas are frequently detected during routine radiological examinations. In most cases, they are asymptomatic and associated with an impacted tooth. However, they are reported to cause site-related symptoms. Bony expansion is seen with most odontomas, resulting in malpositioning of teeth and extraoral swelling [3]. In rare occurrences, the eruption of the odontoma could expose it to the oral cavity, causing infection, pain, localized inflammation, and even regional adenopathy [1]. In addition, odontomas may be associated with dentigerous cysts or nasopalatine cysts [4]. In the current case report, the patient visited the clinic complaining of unspecified pain and pressure. Clinically, a protruding bulge was seen on the labial surface without perforation of the cortex. The odontoma affected the normal eruption of the canine and led to its impaction.
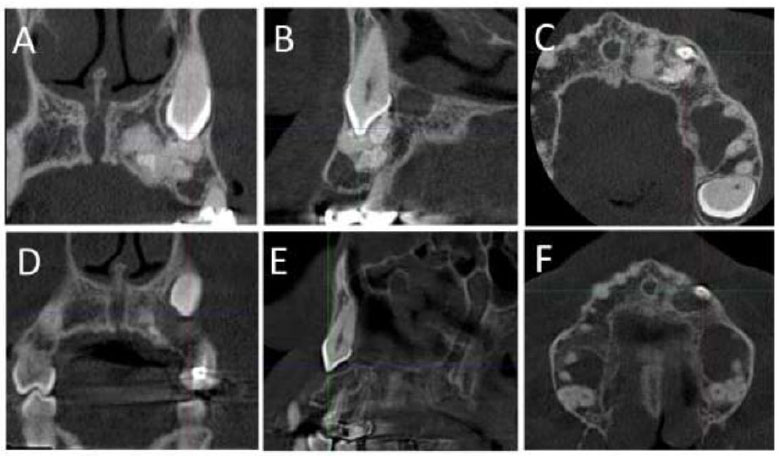
Preoperative and postoperative CBCT sections showing the relationship between the odontoma and the impacted tooth 23 in (A) preoperative coronal section, (B) preoperative sagittal section, (C) preoperative axial section, (D) postoperative coronal section, (E) postoperative sagittal section, and (F) postoperative axial section.
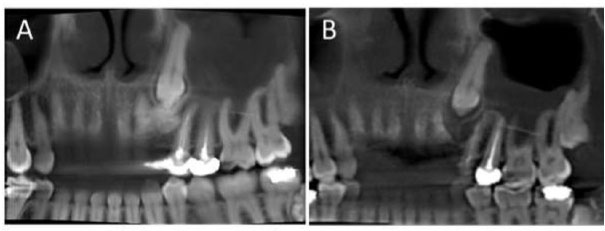
CBCT images illustrating the eruption rate of tooth 23 and the adjacent maxillary sinus in the present case. (A) Preoperatively and (B) eight months postoperatively, where the eruption condition of the left maxillary sinus has not changed and radiopacity in the left maxillary sinus has decreased.

The exposed surgical site following mucoperiosteal flap elevation. The bone protuberance at the site of the odontoma is evident (A), while the odontoma is clearly visible after osteotomy of the cortical bone (B).
According to previous literature studies, different treatment approaches for odontomas have been proposed, ranging from surveillance to surgical excision, depending on their location, size, and proximity to adjacent structures. With the Lefort 1 down fracture osteotomy approach, large lesions that extend into the maxillary sinus in the posterior maxilla have been treated with superior access and with occlusion correction [5]. Conservative treatment options for impacted teeth, following the removal of surgical obstructions, include three modalities. The first involves doing nothing and leaving the tooth in place. The second modality includes surgery with immediate traction, which involves the cementation of an active orthodontic brace during surgery. The third option involves surgery with delayed traction, in which the removal of the obstruction is followed by monitoring for spontaneous eruption. However, if the tooth remains impacted, delayed traction ensues [6]. In addition, non-conservative treatment includes removal of the odontoma and extraction of the impacted teeth [6]. Late diagnosis of an odontoma has been attributed to the displacement or transmigration of the impacted tooth to an unfavourable position, further complicating orthodontic treatment [7]. In the present case, the treatment was performed by removing the odontoma and preserving the canine, being crucial to maintaining the integrity of the dental arch and the patient's aesthetics, and enabling future orthodontic treatment.
The spontaneous eruption of impacted teeth may be preferable to surgical orthodontic treatment. However, predicting whether spontaneous eruption will occur and determining the timeframe for emergence can be challenging [8]. If the impacted tooth does not emerge during this timeframe, the recommended course of action after surgical exposure is delayed orthodontic traction, mirroring the approach taken in the current case. However, the time frame may be affected by the patient's age, the position of the impacted canine, the shape of the root, along with other factors [6]. For young patients with alveolar impaction and adequate space for eruption, conservative surgical treatment is recommended. Nevertheless, it is essential to note that spontaneous movement of the impacted tooth is least expected when the root is mature or when the tooth is not well aligned. Indeed, early removal of an odontoma may result in spontaneous eruption of impacted teeth if root development is incomplete [9]. However, in the present case, no spontaneous eruption was observed during the follow-up visit, which took place about eight months after surgery. This may be attributed to the patient's age since the tooth passed the usual eruption period. Moreover, it has been suggested that the presence of dilaceration in the root contributed to the non-eruption of the affected tooth. The altered root morphology has been found to pose a mechanical challenge, creating obstacles in the tooth's path towards proper eruption [10].
In the present case, the odontoma was removed using a combination of bone bur and chisel during piecemeal resection. A large round surgical bone bur with a straight surgical handpiece allowed for precise and controlled bone removal, while the chisel facilitated the separation and extraction of the odontoma fragments. The same approach was used in a previous study to remove large odontoma [11]. This approach has reflected a comprehensive treatment strategy aimed at achieving favorable long-term outcomes for the patient in terms of both oral health and aesthetics.
In the current case, we opted not to use a bone graft, allowing the defect to heal naturally through blood clot formation, as the defect was manageable. Additionally, we aimed to utilize the available space to promote eruption or support future orthodontic traction. Indeed, bone grafts might be indicated after odontoma excision depending on the specific treatment needs and the odontoma's size and location [12].
About 35% to 54% of females experience menstrual-related migraines prior to menopause mainly due to hormonal fluctuations [13]. The current patient showed an onset of severe unilateral unspecified pain in the left anterior region radiating to the sinus and orbital region, nausea, and photophobia two days prior to the menstrual cycle. According to the international classification of headache disorders, these symptoms are classified as pure menstrual migraine without aura [14]. Chisa et al. recommended patients to keep a headache diary to link between the menstrual cycle and migraine episodes. Treatment of migraines is challenging as patients respond differently to the same treatment [15]. Treatment targets the symptoms of migraines, aiming to improve the patients’ quality of life with options, including migraine-specific and nonspecific acute and prevention treatments [13]. The removal of the odontoma alleviated the unspecified pain. Her other related symptoms, however, remained unchanged, and she was referred to her physician for treatment of the menstrual migraine.
CONCLUSION
This report has presented the case of a large complex odontoma in a 32-year-old patient, who presented with a feeling of unspecific pain and pressure in the relevant area. Conservative surgical removal of odontomas is a simple procedure. However, attentive care is necessary when an impacted tooth is planned for further orthodontic treatment. Diagnosis and surgical management at an early age are the key to preventing eruption disturbances or cyst formation. It generally has a good prognosis, and careful surgical excision is a predictable treatment.
AUTHORS’ CONTRIBUTION
Mohammed Amjed Alsaegh, Ahmed Zaki, and Aisha Abdalla Alowais contributed to the study concept and design; Dua’a Hamed Abuzayed and Aya Mustafa Razouk collected the data; Ahmad Mohammad Wahbeh Ibrahim, Asmaa Khaled Abdulkarim, and Asia Muatasim Alkubaisy wrote the paper. All authors have reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| WHO | = World Health Organisation |
| UDHS | = University Dental Hospital of Sharjah |
| CBCT | = Cone beam computed tomography |
| ENT | = Ear, nose, and throat |
| VAS | = Visual analog scale |


