All published articles of this journal are available on ScienceDirect.
The Lingual Foramen Variations Detected on Cone Beam Computed Tomography (CBCT) Volumes: a Retrospective Radiographic Study
Abstract
Objective
This study aims to investigate the anatomical variations of lingual foramina detected on cone beam computed tomography (CBCT) volumes in a sample of the Palestinian population seeking dental implant treatment.
Methods
A retrospective radiographic study was conducted on patients’ CBCT volumes. The lingual foramina (LF) number, direction (e.g., superior median [SMLF], horizontal median [HMLF], and inferior superior median [IMLF]), height (LH), width (LW) and length (LL) were recorded on CBCT views. Distances from the buccal and lingual aspects of the lingual foramina to the superior and inferior aspects of the alveolar ridge were measured. Moreover, the presence of lateral lingual foramina was also examined. Statistical significance in the differences and relationships of the variables was tested using several statistical tests. The intraclass correlation coefficient (ICC) was used to analyze intra- and interobserver agreement.
Results
One hundred and nineteen patients were analyzed. 78.99% of patients presented with one lingual foramen,17.65% and 3.36% with two and three canals, respectively. The measurements LH, LW, and ML were, on average, 0.64mm,0.8mm, and 7.06mm, respectively. The LH, LL, and LW showed a statistical difference when compared for different lingual foramina directions.
Conclusion
Among the analyzed sample, the majority of the lingual canals were single and pointing upward. Few individuals had lateral lingual canals visible. A careful assessment utilizing cross-sectional views is strongly advised to analyze the lingual canal’s structure and rule out any potential anatomical variation.
1. INTRODUCTION
The incisor and premolar portions of the jaw frequently include lingual foramina, which are tiny pores on the lingual surface with their associated canals [1]. According to where they occur, lingual foramina are divided into two types: either laterally, i.e., lateral lingual foramen (e.g., found in premolar region) or at or just about the midline, i.e., median lingual foramen [1-3]. The lingual artery, sublingual artery, and branches of the mylohyoid nerve all contribute to the lingual canal contents [1, 2, 4, 5].
There is inconsistent evidence in the literature regarding the safety of surgical intervention in the inter-premolar region, as the key anatomical structures are generally thought to have a minimal risk of harm during surgeries performed on the mandibular anterior area [1, 5-9]. A safe intervention,therefore, necessitates a prior thorough analysis of the anatomy of the anterior mandi bular region [3, 5].
LFs have been described as tiny apertures in the mandibular lingual area, which may be detected on radiographs as tiny radiolucent structures that are approximately ten millimetres below the apices of the front teeth [10]. The size is varied, with a diameter that is typically between one and two millimetres but with possible alterations in position, number, and length, making it challenging to detect the LF with a traditional radiographic assessment [10-12].
The frequency of such anatomical structures is inconsistent between populations. The current study aims to evaluate the variable anatomy of the lingual canal of patients seeking dental implant treatment using CBCT sagittal views among a sample population in the West Bank, Palestine. In addition, not only the number and location of the lingual canals but their average dimensions were also recorded. According to a review of the literature, no similar studies have been performed on Palestinian residents in the West Bank.
2. MATERIALS & METHODS
A cross-sectional, retrospective study on the radiographic records of patients who visited the graduate teaching clinics of the Department of Dental Sciences, Faculty of Graduate Studies at Arab American University (Ramallah, Palestine) seeking dental implant treatments between January 2018 and March 2023 was conducted. The study was approved by the Helsinki Ethical Committee of the Palestinian Health Research Council (# PHRC/HC/1229/22). Patients’ radiographs meeting the inclusion criteria were selected after the initial analysis of all the available data for the study (non-randomized sampling).
The inclusion criteria included dentate and edentulous patients of either gender (over 18 years of age), as well as patients whose CBCT volumes were of diagnostic quality and depicted the lower anterior jaw region. Patients presented with jaw bone pathology in the region of interest and low-quality CBCT volumes were excluded. Patients' gender and age were recorded for further analysis.
The CBCT volumes were acquired using the i-CAT™ FLX 17 (DEXIS™, Pennsylvania, USA) with exposure parameters: 120 kVp, 5 mA, 4.8s- 26.9 seconds. The CBCT volumes were analyzed by two examiners (i.e., the principal investigator and a maxillofacial radiologist) using the OnDemand® 3D Software (CyberMed®, Seoul, South Korea). The study was performed and partially repeated (2 weeks after the primary analysis) by the primary investigator and independently by the other examiner. Before commencing the analysis, each examiner received individualized training to calibrate with the methodology. The radiographs were analyzed on a desktop-grade monitor.
The number and frequency of the median lingual foramina/canals and their maximum dimensions, i.e., height (LH), length (LL), and width (LW) of each lingual canal were recorded (Fig. 1A-C). The direction/ orientation of the median canals in reference to the horizontal mandibular plane, i.e., inferior (IMLF), horizontal (HMLF), and superior (SMLF) was identified (Fig. 2). Except for LW (which was conducted on CBCT axial views), the analysis was conducted on CBCT sagittal views. The LH was measured as three measures along the extent of the canal and an average of these values was recorded. For the median lingual canals, the distances (Superior distance buccal (SDB), Superior distance lingual (SDL), Inferior distance buccal (IDB), Inferior distance lingual (IDL) from the upper and lower borders of the alveolar bone to the buccal and lingual ends of each foramen/a were measured (Fig. 1B & D). In the case of more than one median lingual canal, these distances were recorded independently for each canal. The presence and location of any lateral lingual canal up to the 2nd mandibular molar were also checked. All the analyzed variables are summarized in Table 1.
All data were analyzed using SPSS (IBM Corp. Released 2019. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp). Normality tests were performed to ensure the normal distribution of the data set. The Kruskal-Wallis and Mann-Whitney U tests were used to examine differences across measures (e.g., LH, LL, and LW between the number and location of lingual foramina). Moreover, the same tests were used to assess the difference between LH, LL, LW, SDB, SDL, IDB, and IDL among different age groups and genders. Several statistical tests were used to check for a significant relationship between variables (e.g., number and location of lingual foramina, presence of lateral canal vs. gender and age), including Fisher's Exact and Chi-Square Tests. At a p-value of < 0.05, the tested factors were deemed statistically significant. Moreover, to measure intra- and interobserver reliability, the intraclass correlation coefficient (ICC) was utilized, with values more than 0.90 indicating excellent reliability and values between 0.75 and 0.9 indicating high reliability.
| Location | Variables Assessed | CBCT View |
|---|---|---|
| Median lingual foramina/canals | • Number and frequency. • Direction/orientation: inferior (IMLF), horizontal (HMLF), and superior (SMLF). • Maximum dimensions, i.e., height (LH), length (LL), and width (LW). • The distances (Superior distance buccal [SDB], Superior distance lingual [SDL], Inferior distance buccal [IDB], Inferior distance lingual [IDL]. |
Except for LW (which was conducted on CBCT axial views), all the other assessments were conducted on CBCT sagittal views. |
| Lateral lingual foramina/canals | • Number and frequency. | Axial and coronal |
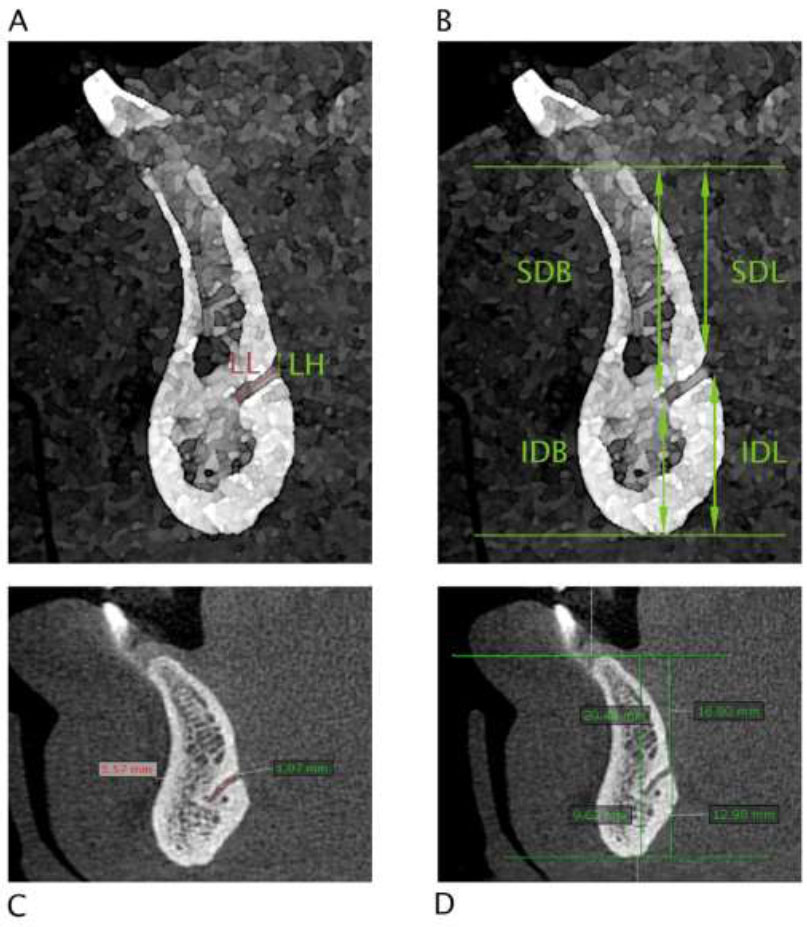
(A & B) illustration and (C & D) sagittal CBCT views showing the measurements performed on the lingual foramen structure.
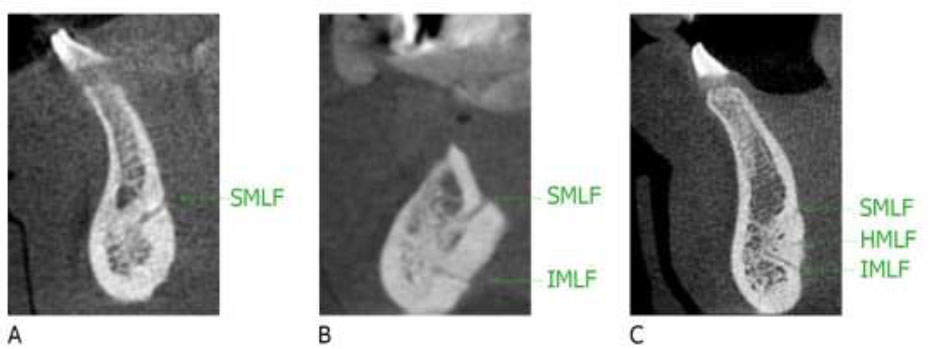
Sagittal CBCT views show (A) one canal, (B) two canals, and (C) three median lingual canals and their orientation (inferior [IMLF], horizontal [HMLF] and superior [SMLF]).
3. RESULTS
One hundred and nineteen patients (148 lingual canals) were analyzed with different age and gender groups, and their demographics are further demonstrated in Table 2. At the midline, 78.99% of the patients presented with one identifiable lingual canal, while 17.65% and 3.36% demonstrated two and three canals, respectively. Regarding the orientation, 80.41% (119 canals) were in the superior direction (SMLF), 6.76% (10), and 12.84% (19) in the horizontal (HMLF) and inferior (IMLF) directions, respectively.
| - | % (n) 119 PATIENTS |
|---|---|
| Age | - |
| Group I: 20-29 years | 6.7(8) |
| Group II: 30 – 39 years | 21.0(25) |
| Group III: 40 – 49 years | 28.6 (34) |
| Group IV: >=50 years | 43.7(52) |
| Gender | - |
| Male | 71.4 (85) |
| Female | 28.6 (34) |
| - |
LH Mean (± SD) |
LW Mean (± SD) | LL Mean (± SD) |
|---|---|---|---|
| Location | - | - | - |
| Superior (SMLF) | 0.65±0.14 | 0.84±0.38 | 7.68±1.78 |
| Horizontal median (HMLF) | 0.49±0.10 | 0.61±0.46 | 4.27±1.61 |
| Inferior (IMLF) | 0.61±0.21 | 0.68±0.42 | 4.76±1.39 |
p-value

|
0.001** | 0.049** | 0.000** |
| Number of foramina found | - | - | - |
| 1 | 0.65±0.14 | 0.82±0.40 | 7.49±1.77 |
| 2 | 0.65±0.12 | 0.88±0.31 | 8.45±1.72 |
| 3 | 0.64±0.11 | 0.90±0.14 | 8.00±1.78 |
p-value

|
0.995 | 0.659 | 0.099 |
 ) Kruskal-Wallis and (T) Mann–Whitney U test.
) Kruskal-Wallis and (T) Mann–Whitney U test.
| - | Age Groups | Gender | ||||||
|---|---|---|---|---|---|---|---|---|
| Group I %(count) | Group II %(count) | Group III %(count) | Group IV %(count) | Statistical Significance |
Male %(count) |
Female %(count) |
Statistical Significance | |
| # Foramen | - | - | - | - | 0.959

|
- | - | 0.546

|
| 1 | 87.5(7) | 76.0(19) | 76.5(26) | 80.8(42) | - | 81.2(69) | 73.6(94) | - |
| 2 | 12.5(1) | 20.0(5) | 17.6(6) | 17.3(9) | - | 15.3(13) | 23.5(21) | - |
| 3 | 0.0(0) | 4.0(1) | 5.9(2) | 1.9(1) | - | 3.5(3) | 2.9(4) | - |
| Direction | - | - | - | - | 0.737

|
- | - | 0.382

|
| Superior (SMLF) | 88.9(8) | 78.1(25) | 77.3(34) | 82.5(52) | - | 81.7(85) | 77.3(34) | - |
| Horizontal median (HMLF) | 0.0(0) | 12.5(4) | 4.5(2) | 6.3(4) | - | 7.7(8) | 4.5(2) | - |
| Inferior (IMLF) | 11.1(1) | 9.4(3) | 18.2(8) | 11.2(7) | - | 10.6(11) | 18.2(8) | - |
| Lateral canals | - | - | - | - | 0.233

|
- | - | 1.000

|
| Yes | 12.5(1) | 4.0(1) | 0.0(0) | 3.8(2) | - | 3.5(3) | 2.9(1) | - |
| No | 87.5(7) | 96.0(24) | 100(34) | 96.2(50) | - | 96.5(82) | 97.1(33) | - |
 ) Fisher's Exact Test. (
) Fisher's Exact Test. (
 ) Chi-Square Test. (**) Statistically significant (p-value < 0.05). Age groups: Group I (20-29 years), Group II (30-39 years), Group III (40-49 years), Group IV (>=50 years).
) Chi-Square Test. (**) Statistically significant (p-value < 0.05). Age groups: Group I (20-29 years), Group II (30-39 years), Group III (40-49 years), Group IV (>=50 years).
| - | Age Groups | Gender | ||||||
|---|---|---|---|---|---|---|---|---|
|
Group I Mean (± SD) |
Group II Mean (± SD) |
Group III Mean (± SD) |
Group IV Mean (± SD) |
Statistical Significance | Male Mean (± SD) | Female Mean (± SD) | Statistical Significance | |
| LH (mm) | 0.73±0.17 | 0.63±0.15 | 0.62±0.16 | 0.64±0.14 | 0.122∫ | 0.64±0.15 | 0.63±0.16 | 0.676

|
| LW (mm) | 0.86±0.33 | 0.81±0.38 | 0.84±0.36 | 0.76±0.43 | 0.740∫ | 0.78±0.41 | 0.84±0.35 | 0.480T |
| LL (mm) | 7.51±1.79 | 7.10±2.18 | 6.97±2.05 | 7.07±2.20 | 0.761∫ | 7.09±2.08 | 7.03±2.21 | 0.748T |
| SDB (mm) | 21.25±3.36 | 20.27±4.30 | 20.98±4.21 | 20.41±3.74 | 0.800

|
21.01±4.02 | 19.63±3.69 | 0.052

|
| SDL (mm) | 18.21±3.65 | 17.28±4.87 | 18.23±5.31 | 17.08±4.97 | 0.602∫ | 17.80±5.01 | 16.90±4.86 | 0.319

|
| IDB (mm) | 10.49±1.68 | 9.24±2.48 | 9.99±2.51 | 9.91±2.51 | 0.212∫ | 9.99±2.44 | 9.44±2.50 | 0.228T |
| IDL (mm) | 13.74±3.79 | 12.07±3.97 | 12.91±4.60 | 12.90±4.04 | 0.302∫ | 13.06±4.04 | 12.09±4.43 | 0.150T |
 ): Independent sample t-test, (
): Independent sample t-test, (
 ): One-way analysis of variance test, (∫) Kruskal-Wallis test, and (T): Mann–Whitney U test. (**) Statistically significant (p-value < 0.05). Age groups: Group I (20-29 years), Group II (30-39 years), Group III (40-49 years), Group IV (>=50 years). LH, LW, LL: Lingual canal height, width, and length, respectively. SDB: superior distance buccal, SDL: superior distance lingual, IDB: inferior distance buccal, IDL: inferior distance lingual. Normality tests were performed to ensure the normal distribution of the data set.
): One-way analysis of variance test, (∫) Kruskal-Wallis test, and (T): Mann–Whitney U test. (**) Statistically significant (p-value < 0.05). Age groups: Group I (20-29 years), Group II (30-39 years), Group III (40-49 years), Group IV (>=50 years). LH, LW, LL: Lingual canal height, width, and length, respectively. SDB: superior distance buccal, SDL: superior distance lingual, IDB: inferior distance buccal, IDL: inferior distance lingual. Normality tests were performed to ensure the normal distribution of the data set.
The diameter of the lingual canal (LH) was, on average, 0.64mm [0.285mm(min.) - 1.85mm(max.)], width 0.8 mm (Avg.) [0.29mm (min.) -1.69mm (max.)], and length (ML) 7.06 mm (Avg.) [ 2.49mm(min.) - 11.58mm(max.)]. The distances SDB, SDL, IDB, and IDL were 20.61mm (Avg.) [11.86 mm(min.) - 29.11 mm(max.)], 17.53mm (Avg.) [7.29 mm(min.) - 32.18mm (max.)], 9.81 mm (Avg.) [ 2.04 mm(min.) - 16.03mm (max.)], and 12.77mm (Avg.) [ 1.08 mm(min.) - 18.65mm (max.)], respectively.
The differences across measures LH, LL, and LW compared for different numbers and locations of lingual foramina exhibited a significance with different lingual foramina directions only (e.g., SMLF, HMLF, and IMLF), as shown in Table 3. A significant relationship between variables, including the number and location of lingual foramina and the presence of lateral canal vs. gender and age, was not evident, as shown in Table 4.
The differences between LH, LL, LW, SDB, SDL, IDB, and IDL differences in different age groups and genders were not statistically significant, as shown in Table 5.
Only 3.36% (4 patients) showed a lateral lingual canal, two on the left side and two on the right side, all in the premolar regions.
The intraclass correlation coefficient (ICC) showed excellent intra- and interobserver agreement. The inter-observer ICC determined for the measure score was 0.999 (95% CI: 0.999 to 1.000), while the intra-observer ICC for the measure was 0.999 (95% CI: 0.998 to 0.999).
4. DISCUSSION
Significant variations in lingual foramina (median and lateral) in terms of numbers and distribution were reported [5]. This indicates the necessity to thoroughly identify the present vascular channels along the surfaces of the surgical site, particularly the lingual surface prior to any surgical procedure.
Complications such as hemorrhage and neurosensory abnormalities may occur if the lingual foramen and its canal contents are compromised [2]. The blood vessels that were typically engaged in lingual hemorrhage occurrences are terminal branches of the sublingual artery (originating from the lingual artery) and a branch of the submental artery originating from the facial artery [13]. Encroachment of the lingual canals and lingual plates would have a detrimental effect, which could result in serious life-threatening bleeding [14-20]. The main concern of such bleeding is airway blockage produced by hematoma development in the mouth floor, which causes swelling that presses the tongue against the palate [21]. A study using ultrasonography of the blood supply of the anterior mandible reported a blood flow rate of the artery going through the lingual foramen as 0.7-3.7 mL/min [22]. The risk of hemorrhage is classified in the literature according to the diameter of the lingual foramen being above and equal to or less than 1 mm, estimating the risk of severe bleeding [2, 23, 24]. When addressing the problem of potential bleeding and its management, modern techniques such as laser tissue welding and nanoparticle glue are utilized to effectively control excessive bleeding [25, 26].
In the current study, although the average diameter of the lingual canal (LH) was 0.64mm, there were diameter readings exceeding 1 mm [0.285mm(min.) - 1.85mm(max.)]. This highlights the importance of identifying these structures and avoiding jeopardizing their extent.
The median lingual foramen may also act as an entrance for a branch of the mylohyoid nerve, supplementary innervating the lower incisor teeth [2, 27]. This potential additional innervation might explain why inferior alveolar or mental injections fail to provide profound anaesthesia of the mandibular incisor teeth in many cases [27].
A study in Italy [5] showed that 32.3% of the sample presented with two lingual foramina, while 27% and 17.7% had three and four foramina, respectively, with directions mostly superior and inferior to the genial tubercles. In addition, 37.3% of patients presented with one lateral canal [5].
Fifty-threepercent of thTurkish population sample showed more than two lingual foramina, an average lingual canal width of 0.89mm, a lingual canal height of 1.16mm, a distance to the crest of 12.04mm, and a distance to the base of the mandible of 18.63mm [13]. The premolar sites (13.4–15.1%) had lateral lingual foramina more frequently than anterior and molar sites [13].
A study reported that the majority of an Indian sample had mostly two lingual foramina with mean diameters of 0.9mm-1.12mm with a substantial number of observed canals (61%) exceeding 1mm (in diameter) [28]. The majority of canals (45%) were inferior to the genial tubercles, and 54% had a downward trajectory. The mean length was 6.37 (SD 1.99) mm [28].
The number of lingual foramina was reported to be mostly three and four in a Chinese sample [0-8 canals], with only 14.93% as lateral canals [2]. The canals were, in majority, equal or submillimeter in diameter (78.77%) and mostly inclined to the horizontal plane, i.e., in direction [2]. The distances measured from the LF to the alveolar crest and inferior mandibular cortex were, on average, 4.28 mm and 27.4mm, respectively [2].
Midline (MLF) and lateral (LLF) lingual foramina were identified in 88%and 75.53% of 278 CBCT volumes, respectively, in a study among Brazilians [29]. The average diameter and distance (to the mandibular inferior cortex) of MLF and LLF were 0.9mm, 9.7mm, and 0.8mm, 8.7mm, respectively [29].
In another study in Saudi Arabia [30], the authors found the most frequent LF to present as two canals (54.7%) followed by one canal (30.9%) and three canals (14.7%), with 97.7% pointing superiorly. The IDB, IDL, LL, and diameter (at buccal and lingual ends) means ranged from 0.53-17.75 mm, 0.58-20.05 mm, 1.35-12.33 mm, and 0.13-2.06 mm, respectively, depending on the position i.e. supra, inter, and infra-spinosum [30]. In a study on a Lebanese sample [31], the lingual canals were identified in 93.33% of the sample. The mean range of the distances between the lingual canal and the ridge crest was 16.24-25.49 mm, and to the base of the mandible, it was 14 mm. The mean length of the canals (superior and inferior) ranged from 4.25-5.81 mm [31]. Gender was not found to be an affecting factor on the number or location of the LF [31].
A summary of the main findings reported in other studies is found in Table 6. Compared to the current study, all the studied canals (148 lingual canals) were radiographically identifiable, with the majority of patients presenting with only one lingual canal and mostly in a superior direction. Interestingly, the percentage of patients who showed lateral lingual canals/foramina was very low (3.36%), which was not in line with other studies [2, 5, 13, 29]. Interestingly, all the variables studied, including the number and location of foramina, presence of lateral foramen, and all the dimensions measured, were not impacted by gender or age. According to our analysis, the detection of the median lingual canal was straightforward on sagittal views, and any other lateral lingual foramina was easily detected on axial and coronal views.
| Study | Country | Sample # | Methodology | Frequency | Number of Lingual Canals | Diameter (in mm) | Length (in mm) | Orientation |
|---|---|---|---|---|---|---|---|---|
| Taschieri et al. 2022 [5] | Italy | 300 | CBCT | 0→ 0.7% 1→ 10% 2→ 32.3% 3→ 27% 4→ 17.7% |
0-8 | - | - | - |
| Sekerci et al. 2014 [13] | turkey | 500 | CBCT | 0→ 1.8% 1→ 14.6% 2→ 28.2% >2→ 53%) |
0-6 | HD 0.89 ± 0.32 VD 1.16 ± 0.39 |
- | - |
| Kumar G, 2017 [28] | India | 100 | CBCT | 0→ 0% 1→ 58% 2→ 42% |
1-2 | 1.07 | 6.37 | 54% →descending 14% → solely anterior 32% → ascending |
| Babiuc et al. (2011) [32] | Romania | 36 | CBCT | 0→ 0% 1→ 71.9% 2→ 9.4% 3→ 15.6% 4→ 3.1% |
1-4 | 0.84 mm | - | 62% →descending 17.3% → solely anterior 20.7% → ascending |
| Locks et al. 2018 [29] | Brazil | 278 | CBCT | “Out of 246 CBCT (88%), 408 lingual midline foramina were identified” |
- | 0.93 | - | - |
| Alqutaibi et al. 2022 [30] | Saudi Arabia | 320 | CBCT | 0→ 0% 1→ 30.9% 2→ 54.7% 3→ 14.7% |
1-3 | 0.87 ± 0.30 | 5.81 ± 2.08 | Supraspinosum 97.7% → directed upward. Interspinosum → 48.9% straight infra-spinosum 71.7% → downward |
| Sheikhi et al. 2012 [33] | Iran | 102 | CBCT | 0→ 0% 1→ 24.5% 2→ 52.9% 3→ 19.6% 4→ 2.9% |
1-4 | 1.12 | 7.83 |
Superior lingual canals 96% → downward to the labial side. 3% → horizontally. 1% → upward to the labial side. Inferior lingual canals 21.47% → downward to the labial side. 2.68% → horizontally. 77.8% → upward to the labial side. |
| Aoun et al. 2017 [31] | Lebanon | 90 | CBCT | 0→ 6.7% 1→ 68.9% 2→ 23.3% 3→ 1.1% |
- | - | 5.81 | - |
| Silvestri et al.,2022 [24] | France | 100 | CBCT | 0→ 0% 1→ 10% 2→ 24% 3→ 30% 4→23% 5→ 10% |
1-7 | 0.87 | 6.15 | 37.4% → Downward 53.1% →Upwards 6.9% → Horizontal 2.6% → Vertical |
| He et al. 2016 [2] | China | 200 | CBCT | 0→ 0.50% 3→ 24.5% 4→23.5% |
0 to 8 | (of 683 foramina) 78.77% ≤1 mm and 21.23% >1 mm |
- | (of 683 foramina) 15.67% → vertical 8.20% → horizontal 76.13% → were inclined |
A recent systematic review and meta-analysis by Barbosa et al., 2022, found that no matterwhich population was investigated, the presence of at least a single LF was the most frequent feature. In addition, the authors discussed the reasons behind the variability of the distances reported (e.g., distances from LF to the alveolar crest or inferior mandibular cortex) as multiple reports utilize different measurement methodologies [10].
This study was conducted with both dentate and edentulous patients. This would impact the distances from the lingual canal to the alveolar crest, particularly superior distance buccal [SDB] and superior distance lingual [SDL] due to bone resorption. Such a distinction was not highlighted in this analysis. Another limitation was the sample size therefore, we recommend that future research should be conducted using a sample size and with consideration of the presence/absence of teeth.
CONCLUSION
The majority of the median lingual canals/foramina among the studied Palestinian sample were in solitary (78.99%: one foramen/canal) and oriented superiorly. Only a handful of patients (3.36%) showed lateral lingual canals. None of the variables studied were affected by different age groups or genders. A thorough examination of the lingual surfaces (particularly at the midline) of the mandible prior to surgical interventions in their vicinity using cross-sectional views is highly recommended to rule out any anatomical variations that could exist.
AUTHOR’S CONTRIBUTION
Study conception and design: M. Abu-Ta’a, K. Beshtawi; data collection: M. Abu-Ta’a, K. Beshtawi; analysis and interpretation of results: K. Beshtawi; draft manuscript: K. Beshtawi. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| LF | Lingual foramina |
| LH | Lingual foramina height |
| LL | Lingual foramina length |
| LW | Lingual foramina width |
| IMLF | Inferior median lingual foramina |
| HMLF | Horizontal median lingual foramina |
| SMLF | Superior median lingual foramina |
| MLF | Midline lingual foramina |
| LLF | Lateral lingual foramina |
| SDB | Superior distance buccal |
| SDL | Superior distance lingual |
| IDB | Inferior distance buccal |
| IDL | Inferior distance lingual |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Helsinki Ethical Committee of the Palestinian Health Research Council (# PHRC/HC/1229/22).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.


