All published articles of this journal are available on ScienceDirect.
Patient Perception of Patient-centeredness in Orthodontic Consultation of Patients from Saudi Arabia
Abstract
Background
Patient-centered care involves respecting patients' dignity and actively including them in decision-making processes. However, its assessment remains quite challenging. This study aimed to assess patients’ perception of patient-centered care in orthodontic diagnosis and treatment planning in Saudi Arabia.
Methods
A descriptive cross-sectional study was conducted among 430 patients seeking orthodontic care at different government and private clinics in Saudi Arabia. An online Revised Patient Perception of Patient-Centeredness (PPPC-R) questionnaire that consisted of 18 questions was filled in by the patient immediately after the initial or treatment planning consultation with an orthodontist and asked to rate the scores from 1 to 4. The final PPPC-R scores were calculated and compared between gender and age groups (adolescents and adults).
Results
A total of 270 responses were obtained with a response rate of 62.79%, and all responses were complete. The mean age of participants was 22.53 years (range 18 to 65 years), and among them, 132 were male. The average score for the questions ranged from 2.26 to 3.58, and the Mann-Whitney test showed no significant differences in the scores between gender (Z = -0.897, p-value 0.370) and age group (Z = -0.092, p-value 0.927). Similar insignificant differences were noted between gender and age group when compared at the level of three factors from the questionnaire.
Conclusion
Patients who are scheduled for orthodontic diagnosis and treatment planning perceived a high level of patient-centeredness. There were no significant differences in the PPPC-R scores between the age group and gender of the participants when measured across each factor level and in total.
1. INTRODUCTION
Patient-centered Care (PPC) in a healthcare setting can be defined as treating patients (and/or parents) with dignity and involving them in the process of clinical decision-making, considering their preferences, values, and needs [1]. PCC gives high priority to individual patient needs, preferences, and values by involving them in healthcare decisions and considering their perspectives on the healthcare process. It emphasizes making patient comprehend their condition, available treatment options, and possible outcomes with each plan, which enables them to make informed decisions about their health. PCC further provides an opportunity for patients to recognize their specific needs, preferences, and desires, acknow- ledging the uniqueness of each individual to facilitate individualized care [2]. However, PCC is poorly understood and practiced in the clinical medical field [3].
The major philosophy of PCC is the recognition of a patient as a person instead of a cluster of diseases [4]. The fundamental concept of PCC in treatment includes a collaborative partnership between the provider and consumer of the healthcare services that considers the emotional, mental, spiritual, and financial perspectives of patients besides the routine clinical perspective [5]. This underscores the importance of understanding patients’ feelings, establishing trust, and empowering the relationship between the patient and the healthcare provider. Moving ahead with patients’ beliefs and values is one of the principles of PCC.
PCC delivers holistic care, providing full autonomy to patients in contrast to the traditional paternalistic approach, and empowers healthcare professionals to deliver their service in the most effective way [6]. This leads to engaging patients in collaboration with mutual respect for each other and shared decision-making for every problem a patient presents to the healthcare provider. This approach has been found to provide greater satisfaction to healthcare workers and reduce the number of medical litigations [7]. PCC is quite relevant and practical in all types of clinical practice regardless of geographic and cultural differences [8, 9]. It is a widely accepted model in the healthcare delivery system and has been adopted by most countries across the globe [10].
PCC has now been introduced and practiced in the context of dentistry and its subspecialties [11]. Many people feel anxious about dental treatment [12], and PCC can play a significant role in mitigating the fear and anxiety among them, along with providing higher-quality treatment [13]. Most dental treatments require monitoring or maintenance or periodic adjustments over a long duration of time, during which a long-term relationship is built between the patient and the clinician, which should be based on trust and respect [14]. Patients trust their clinicians, relying on their opinion on the management of the disease condition based on their clinical experience and expertise. Similarly, patients expect some degree of respect toward them in the form of autonomy, choices, empathy, and professionalism [15]. PCC has been reported to have an improved dental experience and better health outcomes [16].
The UK General Dental Council (GDC) has set standards of care that all dentists should follow, and the basic principles of PCC are included [17]. Different models of PCC have been introduced in dentistry and developed based on patients' and dentists’ perspectives, a review of the literature, and interviews with the stakeholders [18]. There is no doubt regarding the benefits of incorporating PCC in routine dental care. However, assessment of its quality remains a challenge. To address this, patient-reported measures are developed that can reflect the quality of care and guide the aspects for improvement [19].
There are limited studies investigating PCC in clinical orthodontics. An online survey was conducted among British orthodontists regarding the knowledge of shared decision-making, and the majority of them were found to have a good understanding. However, they were eager to receive more training in this context [20]. Amin et al. compared the perception of patients and orthodontists after initial consultation or treatment planning consul- tations and found high scores in patient-centeredness, although there were statistically significant differences between the scores reported by patients and clinicians [21]. Madhan et al. found that the attitudes of Indian orthodontic postgraduate students gradually changed to more patient-centric as they progressed through their academic courses [22].
Assessing patients’ perceptions is integral to providing quality healthcare, and this offers true feedback that indicates the areas that are satisfactory and areas that need immediate attention. This feedback process plays a vital role in transforming the healthcare delivery process, providing maximum satisfaction to the consumers and enhancing the overall quality of care [23]. There are no such studies in the context of Saudi Arabia that assess the perception of patient-centered care in orthodontics. Hence, this study was planned to assess the patient’s perception of patient-centered care in orthodontic diagnosis and treatment planning in Saudi Arabia. The secondary objective was to find out any differences in perception towards patient-centered care between different age groups and genders. The null hypotheses were:
1. There were no differences in the perception (measured with the PPPC-R questionnaire) between age groups and gender.
2. There were no differences in the perception between age groups and gender when measured across the three factors of the questionnaire.
2. MATERIALS AND METHODS
This was a descriptive cross-sectional study carried out from October 2023 to Feb 2024 after ethical approval from the Research Ethics Standing Committee of the University of Hail (H-2023-393). A total of 430 participants were approached from different government hospitals and private clinics.
A recent study that used revised Patient Perception of Patient-Centeredness in pregnant women found a mean total score of 62.2 (SD = 10.5) for all 18 items in the tool [24]. Considering the margin of error to be 1.3 of the mean at a 95% Confidence Interval, the required sample size would be:
 |
 |
 |
Considering a 40% non-response rate, the final sample size will be approximately 420.
A validated tool to assess patients’ perception, the “Revised Patient Perception of Patient-Centeredness (PPPC-R)” questionnaire devised by Ryan et al. [25] was used in this study after seeking permission from the original developers. This questionnaire consisted of 3 factors with 18 questions that record patients’ reflections after an encounter with a clinician. The factors were “Healthcare Process,” “Roles,” and “Context and relationship,” with 8, 2, and 8 questions in them, respectively. This was the modification of the original 9-item Patient Perception of Patient Centeredness question [26]. A Google Form was created to record responses from the participants.
The study participants consisted of 18-year-old or older patients seeking orthodontic care at different government and private clinics in the cities of Hail, Riyadh, Madinah, and Jeddah in Saudi Arabia. Informed consent was obtained from them prior to enrollment, and they were briefed on the questionnaire. Subsequently, they were asked to fill out the questionnaire after the initial consultation or treatment planning consultation with an orthodontist. For each item, there were four possible responses on a scale from 1 to 4, out of which one should be ticked. Score 4 indicated the most patient-centered- ness, and score 1, the least.
The information obtained from this online question- naire was obtained in the Excel sheet and this was subjected to further analysis with SPSS version 25 to explore the perception of patient-centeredness. The total score for each patient was obtained by adding individual scores from the 18 questions. The non-parametric Mann-Whitney test was used to compare the scores in total and also at different factor levels between the gender and the age group.
3. RESULTS
A total of 270 responses were obtained when 430 participants were approached, securing a response rate of 62.79%. Among the responses received, all forms were completely filled and included in the analysis. One hundred and thirty-eight (51.1%) respondents in this study were female and 132 (48.9%) were male. The mean age of the participants was 22.53 years (Standard deviation 5.67 years) with a range from 18 years to 65 years. Most of the respondents (70.7%) were adults (≥20 years), and adolescents comprised the remaining 29.3% (Table 1).
The mean scores of the questions ranged from 2.26 to 3.58 (Table 2). The distribution of each score across the questions shows that the majority of scores were 4 (Fig. 1). The lowest score was obtained for Q1 and the maximum for Q14. Similarly, mean scores across each factor were also calculated (Table 3).
The distribution of the mean scores at the level of three factors and in total were found to be non-normally distributed as demonstrated by Kolmogorov Smirnov test (p <0.001) and Shapiro Wilk test (p < 0.001). Hence, non-parametric tests were used to compare the scores across genders and age groups.
| - | Age Group | Total | ||
|---|---|---|---|---|
| Adolescents (<20 years) |
Adults (≥20 years) |
|||
| Gender | Female | 43 | 95 | 138 |
| Male | 36 | 96 | 132 | |
| Total | - | 79 | 191 | 270 |
| S.No. | - | Question | Mean Score | SD | Median | Interquartile Range |
|---|---|---|---|---|---|---|
| 1 | Healthcare process | To what extent was your main problem(s) discussed today? | 2.26 | 0.602 | 2 | 2 to 3 |
| 2 | How well do you think your provider understood you today? | 3.54 | 0.660 | 4 | 3 to 4 | |
| 3 | How satisfied were you with the discussion of your problem today? | 3.43 | 0.673 | 4 | 3 to 4 | |
| 4 | To what extent did your provider explain this problem to you? | 3.50 | 0.678 | 4 | 3 to 4 | |
| 5 | To what extent did you agree with your provider's opinion about the problem? | 3.50 | 0.672 | 4 | 3 to 4 | |
| 6 | To what extent did your provider ask about your goals for treatment? | 3.49 | 0.683 | 4 | 3 to 4 | |
| 7 | To what extent did your provider explain the treatment? | 3.50 | 0.710 | 4 | 3 to 4 | |
| 8 | To what extent did your provider explore how manageable this treatment would be for you? | 3.46 | 0.703 | 4 | 3 to 4 | |
| 9 | Roles | To what extent did you and your provider discuss your respective roles? | 3.45 | 0.681 | 4 | 3 to 4 |
| 10 | To what extent did your provider encourage you to take the role you wanted in your own care? | 3.51 | 0.683 | 4 | 3 to 4 | |
| 11 | Context and relationship | How much would you say that this provider cares about you as a person? | 3.50 | 0.720 | 4 | 3 to 4 |
| 12 | To what extent does your provider know about your family life? | 2.70 | 1.088 | 3 | 2 to 4 | |
| 13 | How comfortable are you discussing personal problems related to your health with your provider? | 3.31 | 0.812 | 4 | 3 to 4 | |
| 14 | To what extent does your provider respect your beliefs, values, and customs? | 3.58 | 0.662 | 4 | 3 to 4 | |
| 15 | To what extent does your provider consider your thoughts and feelings? | 3.34 | 0.764 | 4 | 3 to 4 | |
| 16 | To what extent does your provider show you compassion? | 3.23 | 0.861 | 3 | 3 to 4 | |
| 17 | To what extent does your provider really listen to you? | 3.44 | 0.767 | 4 | 3 to 4 | |
| 18 | To what extent do you trust your provider? | 3.44 | 0.728 | 4 | 3 to 4 |
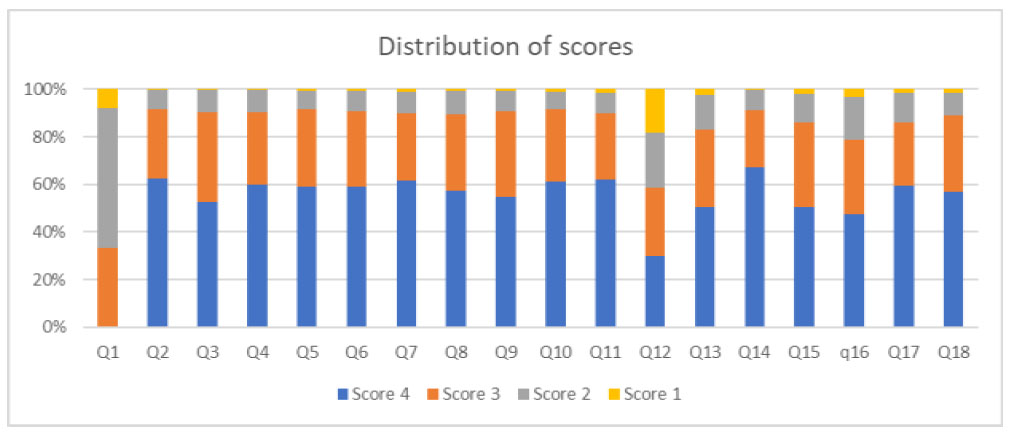
Distribution of scores for each question.
| Participant Groups |
Factor 1 Mean Healthcare Process Score (Q1 to Q8) |
Factor 2 Mean Roles Score (Q9 to Q10) |
Factor 3 Mean Context and Relationship Score (Q11 to Q18) |
Total Mean Score (Q1 to Q18) |
|---|---|---|---|---|
| Adolescent | - | - | - | - |
| Female | 27.14 | 7.07 | 26.12 | 60.33 |
| Male | 26.44 | 7.06 | 26.89 | 60.39 |
| Subtotal | 26.82 | 7.06 | 26.47 | 60.35 |
| Adult | - | - | - | - |
| Female | 26.44 | 6.83 | 26.21 | 59.48 |
| Male | 26.75 | 7.01 | 26.92 | 60.68 |
| Sub total | 26.60 | 6.92 | 26.57 | 60.08 |
| Grand Total | 26.66 | 6.96 | 26.54 | 60.16 |
| Scores | Mean Rank Male | Mean Rank Female | U | Z | p-value |
|---|---|---|---|---|---|
| Factor 1 Score | 137.18 | 133.89 | 9330 | 0.349 | 0.727 |
| Factor 2 Score | 138.27 | 132.85 | 9473.5 | 0.616 | 0.538 |
| Factor 3 Score | 142.28 | 128.81 | 10003.5 | 1.407 | 0.159 |
| Total Score | 139.85 | 131.34 | 9682.5 | 0.897 | 0.370 |
| Scores | Mean Rank Adolescent | Mean Rank Adult | U | Z | p-value |
|---|---|---|---|---|---|
| Factor 1 Score | 138.40 | 134.30 | 7315.5 | -0.395 | 0.693 |
| Factor 2 Score | 142.67 | 132.53 | 6978 | -1.048 | 0.295 |
| Factor 3 Score | 134.36 | 135.97 | 7634.5 | 0.155 | 0.877 |
| Total Score | 136.18 | 135.22 | 7491 | -0.092 | 0.927 |
A Mann-Whitney U test was performed to evaluate the difference in the scores between genders at both the factor levels and in total. The results indicated that gender did not influence the scores either at the factor level or in total (Table 4).
Similarly, no significant difference was noted in the scores at both the factor levels and in total when compared between the age groups, as demonstrated by the Mann-Whitney U test (Table 5).
4. DISCUSSION
This study was an online survey aimed to explore the patient's perception of patient-centered care in ortho- dontic diagnosis and treatment planning within the context of Saudi Arabia. The comprehensive analysis of the responses from this questionnaire revealed an overall mean score of PPPC-R to be satisfactory, indicating alignment with the principles of patient-centered care. Moreover, this study did not find any statistically significant differences in the perception of patient-centeredness between gender or age groups, and the null hypothesis 1 could not be rejected. Similarly, when evaluated at the level of three factors in this question- naire, no significant differences were found between gender and age group. Thus, the null hypothesis 2 also could not be rejected. This suggested equitable distribution of patient-centric ideals across orthodontic patients with diverse demographics.
The response rate to the online questionnaire in this study was 62.79%, and all responses were complete. Our study used a validated tool consisting of 18 short questions, and all the questions were made mandatory in the Google form. Similarly, there was a reminder for incomplete submission, and the subject were directed to the question that required a response. This might be the main reason for a complete response from the respondents. Typically, surveys assessing patient satis- faction often report a low response rate, with figures as low as 30% being reasonable and rates surpassing 80% considered remarkable [27]. A high non-response may indicate dissatisfaction among patients as they are less likely to respond to the questionnaire. Incomplete responses could stem from various factors, such as dissatisfaction, ambiguity in questions, or lengthy questions. Additionally, online surveys often produce low responses compared to face-to-face interviews. In a study using an online PPPC-R questionnaire for pregnant ladies, a response rate of 75.3% was obtained with few incomplete responses [24].
In this survey, the PPPC-R questionnaire was used as a tool to measure the patient’s perception of patient-centeredness after initial consultation appointments for orthodontic diagnosis and treatment planning. Houden et al. conducted a systematic review of the instruments to assess patient-centered care. They found that the Patient Perception of Patient Patient-Centeredness (PPPC) and Consultation Care Measure (CCM) questionnaires were specifically designed for this purpose, offering accurate measurement of health outcomes in the short term [28]. Acknowledging the importance of patients’ insight into patient-centeredness, PPPC was revised by Ryan et al. to record a broader spectrum of participant experiences. The revision expanded the original set of 14 questions to a more comprehensive set of 18 questions and included an additional component of enhancing the patient-clinician relationship, which explores the dynamics of current healthcare delivery [25]. Citing the value of this questionnaire, the original English version of this questionnaire has been translated into different languages [29] and contexts [30-32].
The age of the samples in this study ranged from 18 to 65 years, indicating a wide patient population repre- senting diverse life stages. To facilitate data analysis and interpretation, the participants were divided into two distinct groups: adolescents (under 20 years) and adults (20 years or older). This categorization aligns with the established and well-accepted conventions in the field of orthodontics, as mentioned by Proffit et al. [33]. Similar criteria for separating adolescents from the rest of the population are also done by King and Vallis [24]. By following consistent division of different age groups, coherence in methodologies was ensured to facilitate easy comparison between the results from other studies.
The first eight questions comprised factor 1 which explored the patient’s chief complaint and disease experiences. For all these eight questions, the mean scores were greater than 3, except for the first one, where the average score was 2.26. The first question was about the discussion of the main problem presented by the patient. Several factors may account for this low score. Limited consultation time, use of medical terminologies beyond the patient’s comprehension, and lack of empathy from orthodontists may make patients feel that their main issues are not acknowledged. Additionally, a compre- hensive examination of all components of oral and facial structures may have inadvertently led the patient to feel that their chief problems were not given much importance.
The next two questions discussed the roles that the patient and clinician play in the treatment and comprised factor 2. In our study, the scores for these questions were 3.45 and 3.51. In the study by Amin et al. using the PPPC questionnaire, the question discussing this role received the highest non-response rate and lowest score [21]. The final eight questions of factor 3 were related to understanding the patient and enhancing the relationship. The mean scores for all questions surpassed 3, except for Q12, which was 2.5. This particular question aimed to assess the extent to which the clinician is acquainted with the patient’s family life. The low score for this question is quite understandable given the nature of orthodontic practice, and it is not essential to explore the family life of the patient.
Overall, the participants of this study highly rated their clinicians with the PPPC-R questionnaire, and this aligns closely with the findings reported from similar studies [24, 32]. On further analysis, no significant correlation was found with the gender and age group of the patient. Similar to our research, using the PPPC-R questionnaire, King and Vallis found an average score of 62.2 from the patients, which did not significantly differ with the age, education, or race of the patients [24]. Similarly, in the study by Amin et al. that aimed to assess patient-centered care in orthodontics, the scores of the PPPC questionnaire did not vary significantly with the demographic details of the patient [21].
The study had a few limitations that warrant acknowledgment. Using a close-ended questionnaire constrains patients from expressing their feelings within the given set of predefined options, potentially neglecting their views and emotions. The study was confined to an urban setting within Saudia Arabia at Hail, Riyadh, Madinah, and Jeddah and didnot represent the reflections of the whole orthodontic population of Saudia Arabia. The long-term nature of the orthodontic treatment and regular interaction with patients can maintain a good relationship over a period of time. However, this study considered patients' perceptions only at the initial case discussion appointment, and this may not reflect the level of care they received over the course of the treatment. Despite these limitations, to our knowledge, this was the first survey to explore patient perception of patient-centeredness in orthodontic patients in Saudi Arabia and thus adds meaningful information to the existing literature. Exploring similar perceptions of the treating clinician and comparing them with the patient’s perception will provide useful insight for comparison and can be the direction for future research.
CONCLUSION
Within the limitations of the study, it can be concluded that:
• There was a high level of patient-centeredness as perceived by patients scheduled for orthodontic diagnosis and treatment planning.
• The scores for PPPC-R did not significantly vary with the age group and gender of the patient.
AUTHORS’ CONTRIBUTION
NHDAS: Conceptualization, Design, Data acquisition, Analysis, Interpretation, Drafting the final manuscript, Approval of the final version
LIST OF ABBREVIATIONS
| PPC | = Patient Centered Care |
| PPPC | = Patient Perception of Patient-Centeredness |
| PPPC-R | = Revised Patient Perception of Patient-Centeredness |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The ethical approval was obtained from the Research Ethics Standing Committee of the University of Hail (H-2023-393).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.


