All published articles of this journal are available on ScienceDirect.
Pulp Cavity Calcification in SLE Patient Associated with Long-term Use of Glucocorticoids: A Case Study with Endodontic Approaches
Abstract
Background
Calcification in the tooth pulp cavity occurs in response to various factors, including dental trauma and chronic irritation. Systemic lupus erythematosus (SLE) is the most common type of lupus, causing widespread inflammation and tissue damage in the affected organs. The SLE condition is generally managed by long-term use of drugs, including glucocorticoids (GCs).
Objective
This study aimed to assess the association of pulp cavity calcification in SLE patients with long-term use of GCs and to present endodontic perspectives on the issue.
Case Presentation
A female SLE patient with a history of long-term use of GCs visited our hospital for an oral surgery examination due to an accident. The crown of tooth 11 was visibly fractured. The tooth was sensitive to cold stimulus, while tooth 21 was mobile. Various examinations (including electric pulp test and panoramic radiography) pointed to the diagnosis of chronic pulpitis in the affected teeth (11 and 21), and cone beam computed tomography (CBCT) revealed that the pulp cavities in all teeth were almost completely calcified. Thus, the root canal treatment (RCT) was attempted and followed by crown restoration for the affected teeth. The involvement of GCs in the pulp cavity calcification was assessed.
Conclusion
According to this case and a series of related studies, long-term use of glucocorticoids is associated with the incidence of pulp cavity obliteration (PCO). More frequent dental examinations and appropriate adjustments in medication use (dose and duration) should be considered and implemented.
1. INTRODUCTION
Calcification in teeth is a process of mineral deposition within the dental tissues and contributes to tooth structure formation. Calcification occurs in specific stages during tooth development, and disruptions during this process can lead to dental disorders. One such disorder is pulp cavity calcification [1], where the pulp chamber and/or root canal of a tooth become filled with calcified tissues. This can arise as a response to dental trauma, caries, or other irritants (including medications) affecting the dental pulp.
To manage chronic health conditions (e.g., SLE), medications (drugs) are playing ever-increasing roles in this regard. However, being unnatural, medications are also considered as irritants that would affect tooth conditions. Glucocorticoids (GCs) are a class of steroid hormones produced by the body and play a crucial role in various physiological processes. Synthetic glucocorticoids, structurally similar to and therapeutically more potent than natural ones, are typically used to manage chronic conditions. However, when used in high doses or for extended periods of time, these GCs would have multiple side effects on the body as well as the teeth. Long-term use of GCs has been correlated with calcification of the dental pulp, and related clinical cases have been reported [2] and reviewed [3, 4]. A recent article [5] reported a case study on a patient taking GCs for the management of paroxysmal nocturnal haemoglobinuria, a blood disorder.
Systemic Lupus Erythematosus (SLE) is a chronic autoimmune disease where the immune system mistakenly attacks healthy tissues throughout the body. This can lead to inflammation and damage in various organs and systems. Treatment for SLE often involves medications to control inflammation and suppress the immune system. Common medications include nonsteroidal anti-inflammatory drugs (NSAIDs) and steroidal drugs, such as synthetic glucocorticoids (GCs). However, the use of such steroid hormones to treat chronic diseases may have adverse effects, including tooth damage and deterioration (e.g., rampant caries) [3, 6, 7].
This paper reports an interesting case of a young Chinese woman with an SLE condition whose tooth cavity calcification was associated with her long-term use of GCs. This paper also reviews related cases and provides endodontic perspectives on reducing and managing tooth cavity calcification.
2. CASE PRESENTATION
A 30-year-old female patient visited the hospital in July 2023 due to a broken upper anterior tooth for four months. The female was diagnosed with SLE at the age of 17 in 2010 and had been taking GC tablets (methyl- prednisolone / 4 mg twice a day) for 13 years. In addition, she had also been treated with other therapeutic agents (Belimumab, Cyclosporin A, or Telitacicept [8] for a short while).
During the initial examination, the crown of tooth 11 was visibly fractured (Fig. 1), and tissue defects were also noted. Neither pulp nor dentin was exposed, and no fistula was found at the apex of the root. The tooth was slightly sensitive to cold stimulus, with no obvious percussion pain. Tooth 21 was found to be slightly mobile (grade I) but had no obvious percussion pain. Electric pulp testing (EPT) was used for pulp sensitivity tests on the patient's anterior teeth. The maxillary central incisors’ EPT values [noted as 12: 6, 11: 5, 21: 7, and 22: 8] were all within the normal range [9]. The EPT values (5 and 7) for the affected teeth (11 and 21) were very similar to the values (6 and 8) of the unaffected teeth (12 and 22).

Preoperative image: Tooth 11 (as arrowed) was fractured.
An oral panoramic radiograph (Fig. 2) showed unclear root canal imaging and low-density shadows in the apical area, indicating root canal calcification in these teeth (11 and 21). The possibility of ghost images of the cervical vertebrae (spine) was ruled out by an anterior sagittal slice of the CBCT scan (see Fig. 3A-B).

Panoramic radiograph showing unclear root canal imaging and low-density shadows in the apical area, suggesting root canal calcification in the affected teeth (11 and 21).
Taken together, the affected teeth were tentatively diagnosed with chronic pulpitis. Thus, the patient was initially advised to undergo RCT first, followed by crown restoration in consideration of her age (30 years old).
With the patient’s informed consent, a pulpotomy was performed on teeth 11 and 21 under local infiltration anesthesia (4% articaine hydrochloride containing 1/100 000 adrenaline) at our department. A stainless-steel K file (size 10) was used to explore the root canals, and the black shadows (as arrowed in Fig. 3C1) resulted from the file. However, due to calcification, full access to the root apex could not be established, and the RCT ended. Thus, 17% ethylenediaminetetraacetic acid (EDTA) gel was applied, and zinc oxide eugenol oil cement was then used for the temporary seal. To better determine the root canal condition, dental cone beam computed tomography (CBCT) was taken. The images (Fig. 3) clearly showed calcification in the pulp chambers as well as in the root canals, not only with the affected teeth (11 and 21) but also with other teeth.
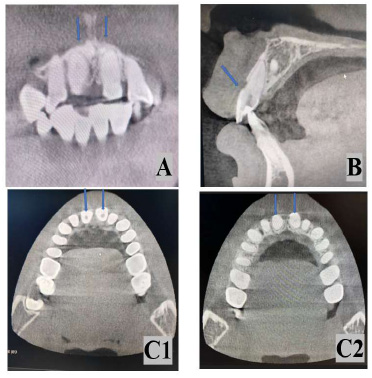
CBCT scans clearly show the calcification in the pulp cavities not only with the affected teeth (11 and 21), but also with all other teeth. The upper left image (A) is a coronal view (with teeth 11 and 21 arrowed), and the upper right image (B) is a sagittal view (with tooth 11 arrowed). The lower images (C1 and C2) are both axial views. The left image (C1) shows the presence of shadow areas (as arrowed in teeth 11 and 21) that were a result of initial drilling in an attempt to open the pulp cavity. The shadow areas are not visible from the right image (C2) as the latter scan is further towards the roots.
The patient returned for a follow-up visit 12 days later and reported no postoperative discomfort. There was no percussion pain, and no red or swollen fistula in the gums was noted. After removing the temporary sealing material and clearing teeth 11 and 21, further examination with the K file discovered that the root canals were substantially blocked (cf. Fig. 3). Thus, light-cured calcium hydroxide was used as the base and filled with composite resin (3M Espe Filtek™ Z350 XT). One week after the completion of filling treatment, the patient underwent dental crown preparation for teeth 11 and 21. A mould (with a colour ratio of 3L1.5) was taken, and temporary crowns on the teeth were made and bonded. Finally, the temporary crowns were replaced with the full crowns (Fig. 4).
The patient was followed up a year later, and there was no report of discomfort or inflammation in the teeth. Although the affected teeth were treated and repaired, the calcification within all teeth remained a concern. In fact, pulp cavity calcification is a significant challenge for all patients taking GC medication for various health conditions. However, there are few reported cases of SLE patients, so it is worth further discussing.

Postoperative photo showing fractured teeth 11 and 21 are fully repaired.
3. DISCUSSION
3.1. Calcification in the Pulp Cavity
Dental pulp calcification is relatively common, with a reported incidence rate as high as 64% [10]. The aetiology of the pulp calcification is not fully understood; however, the major causes are generally accepted as follows: 1) Normal Physiological Changes: As teeth age, the coronal and root areas of the pulp cavity undergo dentin mineralization [11]. The pulp cavity tends to gradually shrink, accompanied by a decrease in sensory and compressive strength. 2) Defensive stress response: When teeth are injured, infected, or decayed, the odontoblasts in the pulp cavity will correspondingly proliferate, forming new reparative dentin, leading to narrowing or even complete disappearance due to calcification in the pulp cavity (for review, see [12]).
In addition, as our lifespan extends, more and more medications are being used to manage chronic health conditions, which can also bring unexpected problems to the body, including the teeth. For instance, radiographic examinations revealed narrowing of the pulp cavity in 51 patients who had long-term use of glucocorticoids to treat kidney disease [13]. Therefore, adverse effects of therapeutic agents on the teeth should be considered and minimised.
3.2. Effect of GCs on Pulpal Narrowing
Glucocorticoids (GCs) are a type of steroids that bind to glucocorticoid receptors and play pivotal roles in regulating glucose metabolism, reducing inflammation, and suppressing the immune system of the body. The most used GCs are prednisone (1) and prednisolone (2), structurally similar to their natural ones [i.e., cortisone (3) and cortisol (4)], as shown in Fig. (5). Prednisone is converted in the body to prednisolone, which mediates its medical effects. Methylprednisolone (2a) is a thera- peutically stronger version of prednisolone.
As these GCs can prevent the release of inflammation-causing substances in the body, they are widely used to manage chronic health conditions, including arthritis, chronic asthma, allergies, autoimmune diseases, and subsequent organ transplants [14]. However, long-term use of GCs would increase the risk of infection, osteoporosis, growth retardation in children, and trauma disorders for healing [15]. The incidence of adverse effects of GCs depends largely on the dose and duration of treatment [16]. A common adverse effect on the teeth is the narrowing of the pulp cavity [17].
3.3. SLE Patients taking GCs and with Calcification in the Pulp Cavity
SLE is an immune system disease characterized by autoantibodies. The use of GCs has good therapeutic results on SLE patients [7], but it is also accompanied by underlying dental problems [18, 19]. Chigono et al. [17] reported a case of an SLE patient taking oral GCs for a long time. They examined the patient’s premolar stumps histopathologically and found that the dental pulp cavity was narrowed in nearly all samples, and odontoblasts became invisible. In our case, the patient has been taking methylprednisolone (a steroidal drug) for over 10 years to manage her SLE condition. The cavities of the patient’s teeth are found to be almost completely blocked (Fig. 3). As the patient is still relatively young (30 years of age), the aging factor is unlikely to be the main cause of her pulp cavity calcification. Instead, the long-term use of GCs is likely associated with widespread calcification of the entire dental pulp cavity in the patient.
To assess the association of GCs taken by the SLE patient with her pulp cavity calcification, we surveyed the literature and compared our case with some related cases (Table 1) on the key aspects, including health condition, age, sex, type of glucocorticoids and its dose and duration. It is impossible to impute the pulp cavity calcification with the use of GCs; however, the long-term use of GCs in the SLE patient does have a clear correlation with calcification in her teeth.

Chemical structures of commonly used medicines of glucocorticoids.
| Condition | Age | Sex | Glucocorticoids | Daily Dose / Duration | Source |
|---|---|---|---|---|---|
| SLE | 30 | F | Methylprednisolone | 8 mg / 13 years | This case |
| - | - | - | - | - | - |
| SLE | 30 | F | Prednisone | 10 mg / 8 years | [20] |
| ACAH | 42 | M | Prednisone | 10-40 mg / 19 years | [21] |
| ACAH | 36 | F | Prednisone | 6-16 mg /10 years | [21] |
| KT | 17 | M | Prednisolone | 12mg / 6 years | [21] |
| RA/SLE | 25 | F | Corticosteroids | NA* / >15 years | [17] |
| PNH | 41 | F | Methylprednisolone | 24-50 mg / 20 years | [5] |

Flowchart of diagnosis and treatment for dental pulp calcification.
3.4. Endodontic Perspectives on Reducing the Adverse Effects
The calcification in the oral pulp cavity caused by long-term use of GCs can bring additional difficulties to the dental treatment of these patients. The most common clinical strategy for such patients would be to wait with prudence, as illustrated in Fig. (6).
When clinical symptoms and radiographs of pulp calcification are clearly presented and root canal access can be established, RCT is recommended. If the root canals are only partially accessible, then it is worth further unclogging the root canals. RCT is effective in dealing with pulpal calcification; however, it should not be used as a preventive measure or as a first-line treatment for discoloured teeth or asymptomatic pulp cavity calcification [20]. When RCT is required, it is important to be careful not to damage the bottom of the pulp chamber or cause lateral or bottom penetration of the pulp chamber.
If the root canal access can only be partially established, the next step is to check for apical periodontitis in the teeth. If the teeth indeed suffer from periapical inflammation, it is recommended to see a specialist who can adopt appropriate techniques, such as guided endodontic access [21] or computer-aided navigation techniques [22]. If unsuccessful, it is recommended to undergo dental pulp microsurgery [23] or even intentional reimplantation [24]. In our case, the pulp cavity calcification affected all teeth. As it would not be most beneficial to carry out RCT for all teeth, the observation/follow-up approach (Fig. 6) was adopted.
In clinical practice, dentists should be more prudent towards patients who have been taking GCs for a long time, pay attention to timely oral hygiene education for patients, and help them prevent and manage corres- ponding oral diseases. It is also necessary to consult with relevant disciplines to discuss the pharmacokinetics and adverse reactions of glucocorticoids and to seek alternative medications (e.g., non-steroidal drugs) or reduce the dosage of glucocorticoids to minimise the occurrence of any adverse reactions associated with GCs.
CONCLUSION
From the patient's history of using GCs and related studies, it can be concluded that long-term use of GCs has significant impacts on calcification in the entire dental pulp cavity. When all teeth are affected, the RCT approach would become impractical. Therefore, a multidisciplinary treatment should be considered for the patients taking GCs to manage their SLE or other chronic conditions.
AUTHORS’ CONTRIBUTIONS
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| GCs | = Glucocorticoids |
| SLE | = Systemic lupus erythematosus |
| CBCT | = Cone beam computed tomography |
| RCT | = Root canal treatment |
| PCO | = Pulp cavity obliteration |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ehical Review Approval was obtained from the Human Research Ethics Committee of the Second Affiliated Hospital, School of Medicine, Zhejiang University; China, Approval number: (20.24) Lunshenyan No. (0872).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
The participant involved in this study provided her written informed consent.


