All published articles of this journal are available on ScienceDirect.
Evaluation of the Adhesive Strength of Different Types of Fiberglass Posts in Flared and Unflared Canal Roots
Abstract
Introduction
Fiberglass posts are used in the rehabilitation of endodontically treated teeth, and adaptation to the canal is a determining factor.
Objective
This study aimed to evaluate the Push-out Bond Strength (PBS) and failure mode of different types of fiberglass posts, associated or not with a fiberglass sleeve (Exacto and Splendor SAP) in different types of canals (enlarged and non-enlarged canals).
Method and Materials
Forty bovine roots were used, and the samples were divided into four groups (n=10). The canals were instrumented in a standardized manner. The samples were cemented with dual self-adhesive resin cement. The roots were sectioned in the coronal, middle, and apical thirds with a thickness of 1 mm. The Push-out Bond Strength (PBS) test was performed in a universal testing machine (EMIC). Statistical analysis: PBS values were recorded, and data were analyzed using repeated measures, such as ANOVA and Tukey's test. To determine the failure mode, a stereomicroscope with 40× magnification and 2.5D analysis was used.
Results
SPrFl showed significantly higher bond strength in the coronal third than SPr and Exc. However, SPr, Exc, and ExcFl did not show any differences between them. Furthermore, similar bond strength was observed between SPrFl and ExcFl. The failure mode was not influenced by the post system (p=0.144) or root third (p=0.146). All experimental groups showed a prevalence of adhesive failures (Types I, II, and III).
Conclusion
The groups that used the Splendor system showed similar results to conventional posts anatomized with resin, but in the middle and apical thirds, there was no statistical difference in PBS.
Clinical Significance
The results of this laboratory test can help the dentist to answer which types of fiberglass can be used to rehabilitate endodontically treated teeth, ensuring good adhesive resistance and, consequently clinical success.
1. INTRODUCTION
Fiberglass Posts (FGP) have been recognized as popular in the dental field because of their benefits in terms of ease of handling, mechanical properties, and aesthetics [1]. They are materials that support the stress distribution in a uniform way on the root surface because they present an elasticity modulus like dentin [2, 3, 4].
The use of FGP in flared roots or wide canals is a challenge since these materials have a standardized size, making it difficult to fully adapt to the root canal walls, especially in the coronal third, requiring a thick layer of resin cement [5, 6]. The greater the thickness of the cement line, the greater the stress levels of polymerization shrinkage. Therefore, thick layers of resin cement can induce structural discontinuities at the adhesive interfaces and consequently increase the risk of failure after cementation [7, 8].
One way to reduce this effect is to anatomize the posts associated with composite resin, which are called anatomical posts, which reduce the volume of the luting cement and adapt better to the canal wall [9]. A limitation of the anatomization of the posts is the technical difficulty for their manufacture, so new types of posts and accessories are being developed to facilitate clinical application and guarantee satisfactory and successful long-term results such as FGP is associated with a fiber sleeve, which can be classified as “universal” [10, 11].
Fiberglass sleeves were introduced in the dental market to improve the adaptation of the FGP to the canal without the need for relining or other clinical steps. They are currently available through a new system of FGP called Splendor SAP, which has the advantage of not needing a specific preparation in relation to the configuration of the root of the canal because in situations where the post is not capable of adjusting to the conduit walls, a sleeve is used to improve this contact, making this system unique [12].
The FGP associated with fiber sleeve is presented as a low-cost alternative to simplify the use of intra-radicular posts, as it is a single diameter post that can be indicated for both narrow and wide canals, varying only the amount of sleeve insertion that varies according to the width of the root canal [13].
This study aimed to evaluate the performance of FGPs associated or not with a glass fiber sleeve in widened and non-widened canals in terms of bond strength to dentin. The two null hypotheses were: 1) no significant differences were found in the bond strength of the different types of FGP in different types of canals; 2) no significant differences were found in the bond strength of the different regions to the root canal walls.
2. MATERIAL AND METHODS
2.1. Specimens Selection
This study was exempted from evaluation and approval by the Animal Use Ethics Committee - CEUA/UFU (Protocol 23117.043246/2024-40). Forty bovine teeth with a root length of 15 mm and similar anatomical size and shape (root volume within 10% of the mean) were selected. The specimens were then stored in distilled water at 4 °C until use.
The posts were randomized into four groups (n=10): a) Exacto + flared canal roots (ExcFl), b) Exact + unflared canal roots (Exc), c) Splendor Sap + flared canal roots (SPrFl), and d) Splendor Sap + unflared canal roots (Splr).
2.2. Root Canal Preparation
The crowns were sectioned perpendicularly to the long axis using a water-cooled diamond disk (No. 7020; KG Sorensen, Barueri, Brazil) up to 15.0 mm from the apical limit and removed. The root canals were endodontically instrumented using a 10 K file (Dentsply Malleifer; Petrópolis, RJ, Brazil), which was introduced into the root canal until it was visible in the apical foramen. Root canals were instrumented to their full length using No. Drills 2 and 3 Gates-Glidden (Dentsply Maillefer, Ballaigues, Switzer- land). Then, a number 4 Gates Glidden bur (Dentsply Malleifer) was used in the coronal and middle thirds of the root canal. Once this wasperformed, the specimens were stored in distilled water at 4 °C [14].

Preparation for placing the FGP. Fig. (A): Number 3 Exacto FGP system drill used for Exc and ExcFl groups. Fig. (B): Splendor Sap Post System Drill used for Splr and Splrfr groups. Fig. (C): Cylindrical diamond bur used to simulate widened flared canal root.
2.3. Preparation for Post-placement
Fifty percent of the specimens from the Exacto and Splendor Sap groups had their flared root using a cylindrical diamond bur so that the wall had a minimum dentin thickness of 1.5 mm. The space for cementing the posts into the roots was obtained using a specific drill for each post system following the manufacturer’s instructions with the same dimensions as the FGP selected. The root was cleaned with abundant irrigation with distilled water, and humidity control was performed using absorbent paper cones. The preparation with the specific drill for each post and the weakening of the roots of the enlarged canal are shown in Fig. (1).
2.4. Fiberglass Post Cementation
For the ExcFl group, the post was anatomized using composite resin (Z350, 3M ESPE, Sumaré, SP, Brazil) before the cementation. Therefore, the FGP was treated with 35% hydrogen peroxide for 1 min (Clariant, Angelus; Londrina, PR, Brazil), washed with distilled water, and then air-dried for 20 seconds. Subsequently, a silane agent was applied to the post for 1 min (Silano, Angelus; Londrina, PR, Brazil). Then, adhesive was applied in two layers to all surfaces, and light cured on each face for 20 seconds. After that, the composite resin was applied to the post, which was not light-cured. To prepare the canal of the anatomized FGPs, the water-soluble gel was applied, and the excess was removed with an absorbent paper cone. Then, the post anatomized with composite resin was inserted inside the root and light-cured for 3 seconds. The post was removed from the root and light-cured for 20 seconds on each side. Reanatomization of the FGPs of the Ext Fl group with composite resin is demonstratedin Fig. (2).
The FGP conditioning protocol was the same for all groups. The FGP and sleeves were treated with 35% hydrogen peroxide for 1 minute, washed with distilled water, and then air-dried. Subsequently, a silane agent was applied to the post for 1 min (Silane, Angelus; Londrina, PR, Brazil). The conditioning of FGPs and fiberglass sleeves is shown in Fig. (3).
Canal cleaning and conditioning were also standardized for all groups. Canals were cleaned by active irrigation with sodium hypochlorite for 1 minute, EDTA for 3 minutes, and distilled water for 1 minute. Humidity control was performed with absorbent paper cones.
Cleaning and treatment protocols were also performed for the cementation of all groups. Cementation was performed with dual self-adhesive resin cement (RelyXTM U200, 3M ESPE, Sumaré, SP, Brazil), which was inserted into the root canal using an Endotip (3M ESPE, Sumaré, SP, Brazil) to minimize the presence of bubbles [14]. The self-mixing tip was positioned as apically as possible, and as the cement was injected, the syringe slowly withdrawn.
For the Exc and ExcFl groups, first, the self-adhesive cement was inserted with an endotip in the apical coronal direction, and then the FGP was positioned in the center of the canal with the aid of tweezers.
For the Splr and SPrFl groups, after insertion of the self-adhesive cement, the FGP was first placed with the aid of tweezers in the center of the canal, and then the sleeve was inserted, involving the previously placed post until it locked inside the canal.
Excess resin cement was removed after 1 minute, and 5 minutes were waited under load (500g) for chemical polymerization. Then, the resin cement was light cured on each coronal surface (occlusal, buccal, lingual, medial, distal) for 40s (Valo Cordless, Ultradent, Indaiatuba, SP, Brazi). The materials used are shown in Table 1.
2.5. Push-out Bond Strength Test (PBST)
Ten specimens from each group were prepared for the mechanical push-out bond strength test and stored for 7 days in distilled water at 37°C.
The roots were fixed in a 20 mm x 20 mm acrylic plate with a cutting edge (Lysanda, São Paulo, SP, Brazil) and sectioned with a water-cooled low-speed diamond disc on a precision mill (Isomet 1000; Buehler) to obtain two slices, 1.0 mm thick each, resulting in two slices for each third of the root (apical, middle and coronal).
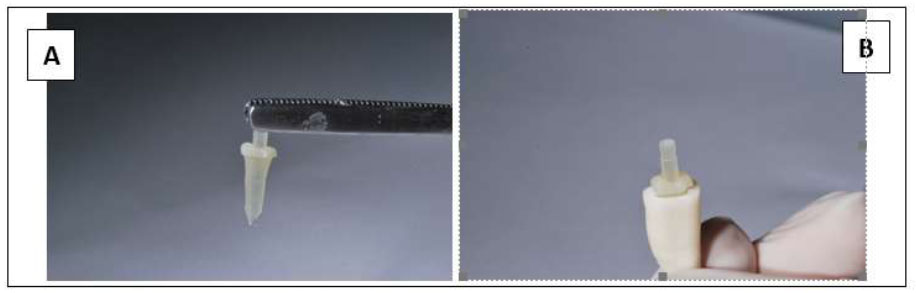
FGP anatomized: (A) Exacto post in a weakened root group with a composite resin before cementation, (B) FGP anatomized positioned at the root.
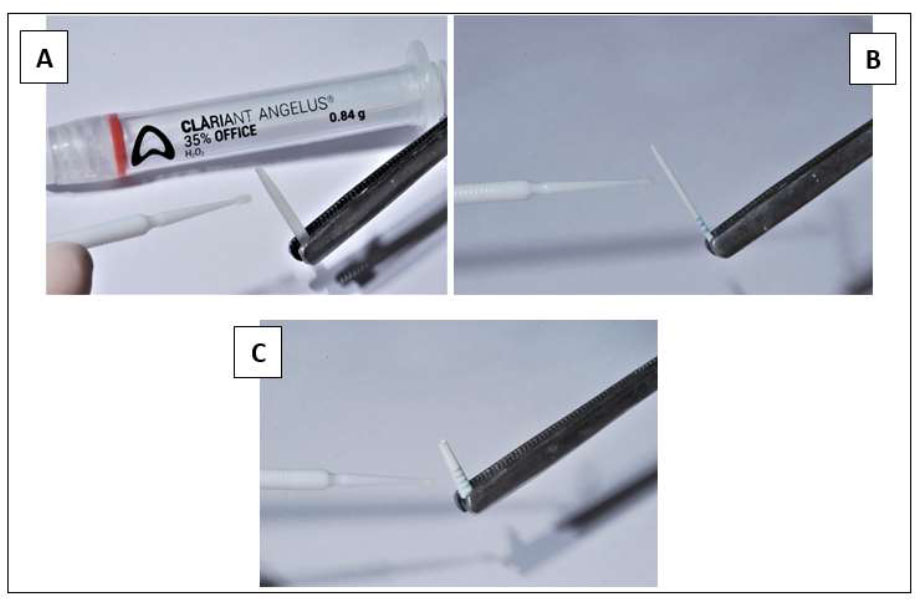
Surface treatment of FGP and sleeves. (A-C) FGP and sleeves were treated with 35% hydrogen peroxide for 1 min, washed with distilled water, and then air-dried. Subsequently, a silane agent was applied to the post for 1 minute.
| Material | Manufacturer | Bath |
|---|---|---|
| RelyX TM U200 | 3M ESPE; Sumaré, SP, BRA | 2113200890 |
| Silane | Angelus; Londrina, PR, BRA | 56547 |
| Hydrogen Peroxide 35% | Angelus; Londrina, PR, BRA | 595105 |
| Composite Resin Z350 | 3M ESPE; Sumaré, SP, BRA | 2110200248 |
| Adper Single Bond Adhesive | 3M ESPE, Sumaré, SP, BRA | 080621 |
| Exacto No. 3 | Angelus; Londrina, PR, BRA | 52948 |
| Splendor Sap | Angelus; Londrina, PR, BRA | 102437 |
The diameter and thickness of the specimens were measured using a stereomicroscope digital camera at 40x magnification with a 2.5D analysis (Mitutoyo; Tokyo, Japan) and a digital micrometer with an accuracy of ± 0.01 mm.
Each slice was prepared and stored for 24 hours in distilled water at 37°C before being subjected to the bond strength test.
Load application tips with different sizes were used for the coronal, middle, and apical third. For the coronal third, a base of 2.5 and a tip of 1.3 was used. For the middle third, a base of 2.2 and a tip of 1.2 was used, and for the apical third, a base of 2,0 and a tip of 1.0 were used [15].
The push-out bond strength was performed using a Universal Testing Machine (EMIC DL 2000, São José dos Pinhais, Brazil) containing a load cell of 5 KgF. The slices were subjected to compression load with a constant velocity of 0.5 mm/min in the apex/crown direction until the failure.
The maximum load at failure was converted to MegaPascal (MPa) and calculated using the following formula:
F(N)/Area
The area was calculated using the following formula:
A=π(r1+R2) √r1-R2)2+h2;
where π is a constant value of 3.14, r and R are the smallest and largest radii, respectively, of the cross-section of the tapered post, and h is the section thickness.
2.7. Failure Mode Classification
The fractured specimens were analyzed under a stereoscopic magnifying glass at 40x magnification (Mitutoyo, Tokyo, Japan) with 2.5D analysis to investigate where the failure occurred. Failures were classified into 1 of 7 types: (Adhesive I) adhesive between post and cement resinous; (Adhesive II) adhesive between the resin cement and the root dentin; (Adhesive III) adhesive inside the FGP and sleeve; (Cohesive I) cohesive in dentin; (Cohesive II) cohesive in FGP; (Cohesive III) cohesive in cement and (Mixed) mixed, with resinous cement covering parts of the post surface.
2.8. Data Analysis
The push-out bond strength data were analyzed using Two-way repeated measures ANOVA and Tukey's tests were used to compare post systems. For normality and homoscedasticity, the Shapiro–Wilk and Levene tests were used. The failure modes were evaluated qualitatively, followed by the Chi-square test. Statistical analysis was performed using the Jamovi 2.2.5 statistical software package (dev.jamovi.org). The significance level was set at 0,05 for all the data analyses.
3. RESULTS
The mean and standard deviation values of bond strength for the groups according to post system and root third are shown in Table 2. Two-way repeated measures ANOVA showed a significant interaction between both factors (p = 0.042). Post system presented differences on µSBS only at the coronal root third. SPrFl had significantly higher bond strength at the coronal third than Splr and Exc. However, Splr, Exc, and ExcFl showed no differences from one another. Also, similar push-out bond strength was observed between SPrFl and ExcFl.
| Fiberglass Post Group | Cervical Third | Middle Third | Apical Third |
|---|---|---|---|
| Splendor weakened - SPrFl | 11,7 ± [1,06] Aa | 11,8 ± 1,43 Aa | 9,11 ± 2,59 Aa |
| Splendor- Splr | 7,88 ± 1,75 BCa | 8,14 ± 2,29 Aa | 9,01 ± 3,45 Aa |
| Exacto - Exc | 7,61 ± 2,97 Ca | 8,3 ± 2,02 Aa | 7,74 ± 3,1 Aa |
| Exacto weakened - ExcFl | 11,1 ± 2,73 ABa | 12,2 ± 4,22 Aa | 9,69 ± 4,95 Aa |
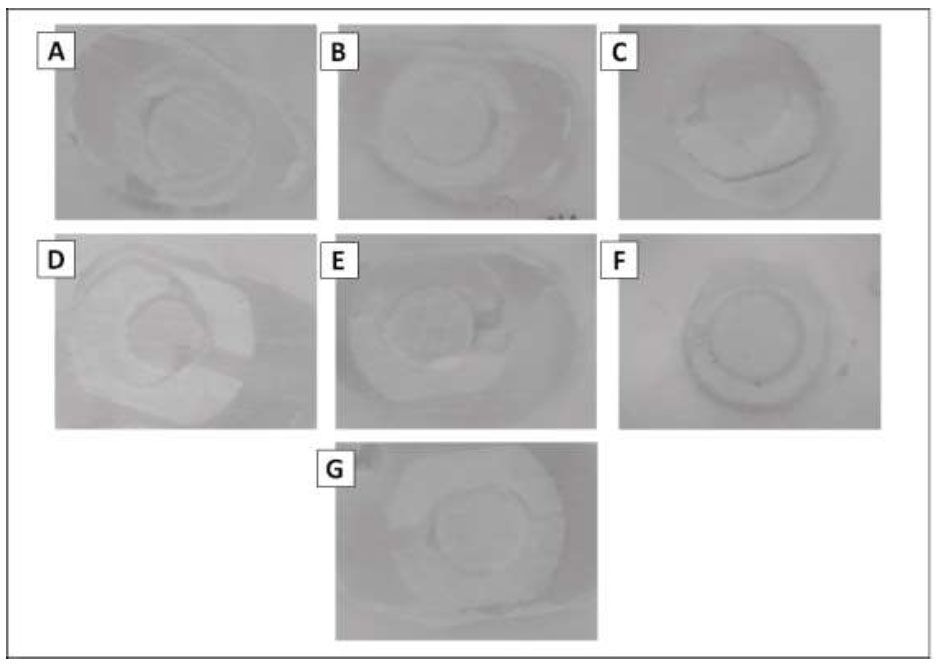
Failure pattern analysis. (A) Type I adhesive failure; (B) Type II adhesive failure; (C) Type III adhesive failure; (D) Type I cohesive failure; (E) Type II cohesive failure; (F) Type III cohesive failure; (G) Mixed failure.
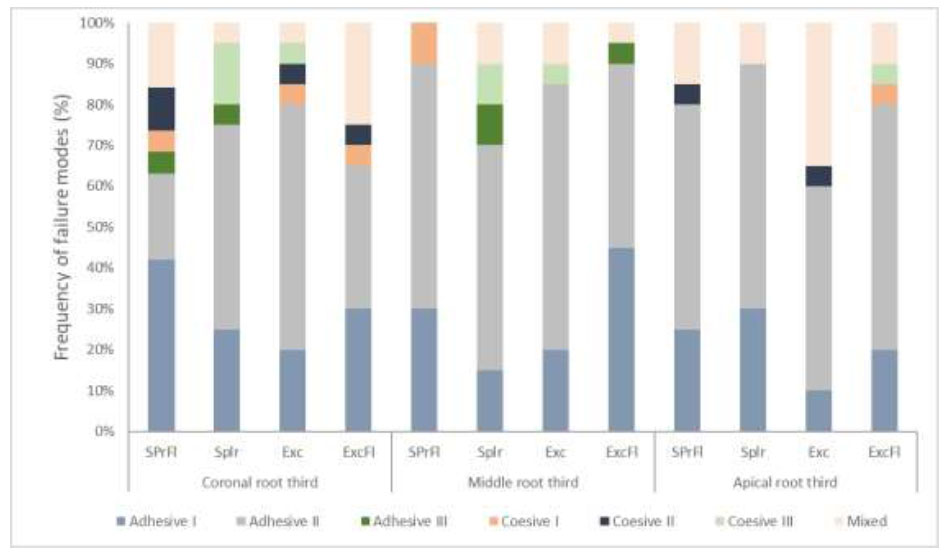
Frequency of failure modes (%). Different cores aloud indicate which type of failure occurred in each group.
The different types of failures observed in the specimens after the µSBS test are illustrated in Fig. (4), and the failure mode distribution (%) for each group is shown in Fig. (5).
The failure mode wasn’t influenced by the post system (p=0.144) or root third (p = 0.146). All experimental groups exhibited a prevalence of adhesive failures (Types I, II, and III).
4. DISCUSSION
This study analyzed the effects of two types of Fiberglass Posts (FGPs) associated with a fiberglass sleeve (SPr and SPrlFl), without relining or fiberglass sleeve (Exc) and relined with composite resin (Exct Fl), in enlarged and non-enlarged canals on the bond strength by the push-out test.
The evolution of dental materials and techniques promotes the possibility of clinical interventions that simplify the technique to be applied, reducing the error rate and ensuring better results in rehabilitation techniques. The adaptation of the FGP to the root canal is a critical factor that can interfere with adhesion, especially in enlarged or oval canals [1, 16]. The fiberglass sleeve emerges as a possibility for relining FGPs that dispenses with the conventional technique with composite resin, which is difficult to apply and requires more clinical time, ensuring better adaptation to the root canal and reducing adhesive failures.
The SPr group showed significantly higher bond strength when compared to the Exc and SPrFl groups. Therefore, the first null hypothesis that no significant differences would be found in the bond strength of the different types of FGP in the different types of canals was rejected. The post system showed differences in µSBS only in the coronal third of the root. SPrFl showed significantly higher bond strength in the coronal third than SPr and Exc; that is, the second null hypothesis that no significant differences would be found in the bond strength of the different regions to the root canal walls was also rejected.
The push-out test offers bond strength values from different locations of the root canal and was used in the present study because it is the most reliable test to evaluate the bond strength of the FGP posts to dentin [3, 16]. It is necessary to consider criteria that influence the results of bond strength to push-out, such as the diameter of the loading tip and the base orifice of the device used, besides the thickness of the specimen, which must be standardized [17-20]
The PBS results obtained in this study showed that there was no statistical difference about the thirds, and this can be attributed to the type of cement and light curing agent used during the cementation process as well as the technique performed. Since self-adhesive cement shows considerably higher values in the literature about adhesive strength, and this is closely related to the number of clinical steps and, consequently to the degree of difficulty in cementation moments, which is reduced when this type of cement is used in the cementation of FGP [8, 16].
A previous systematic review adopted a statistical approach to assess the influence of resin cement and adhesives on FGP retention and demonstrated that self-adhesive types of cement perform better [20, 21]. It is known that adhesive failure of FGP has been described as the most recurrent complication of cemented posts [16, 22, 23].
The fact that there were no statistical differences between the thirds can be considered the care that was taken during the execution of the cementation technique [24]. According to Silva et al. 2019, the use of dual automatic self-adhesive cement associated with an endo tip is capable of promoting a thicker and more continuous cementation line, as it facilitates the correct insertion of the cement, considerably reduces the number of bubbles (mainly in the apical thirds) and consequently increases the area real adhesive and the values of adhesive strength, and this factor can be used to justify the fact that there is no statistical difference between the groups [16].
Although the lower values were obtained by the Exacto + unflared roots group, it is important to emphasize that these results show the advantage of posts with better adaptation to the walls of the roots since, in situations where the FGP are not well adapted to the walls, the bond strength may present lower results, once it is known that greater the thickness of the cement layers, greater risk of bond failures, especially in the coronal third, where the posts, mainly less caliber, probably need a thick layer of resin cement [25-27].
Well-fitting posts and thin layers of resin cement are essential to provide a better luting to root dentin [4, 16], as thick layers of cement decrease the bond strength, as a greater volume of cement leads to greater volume shrinkage, generating greater stress at the adhesive interface and causing the greater formation of cracks and bubbles inside the root canal [1].
The filling obtained with the anatomization using composite resin was an important factor for the bond strength in the coronal third since the intimate contact between the anatomized post associated with the obtaining of a thin layer of cement is an important factor in the adhesive strength [9, 11, 27, 28]. For the weakened Exacto group, the technique of composite resin anatomization- FGP was applied, which resulted in higher bond strength results.
For both the weakened Splendor group and the non-weakened Splendor group, the presence of the post associated with the sleeve, both made with fiberglass, luted with the dual self-adhesive resin cement promoted excellent results for the bond strength in the coronal third, as the sleeve is inserted into the canal until there is micromechanical retention, allowing the root can be filled desirably.
In this study, the type of FGP, type of root canal, and type of third did not influence the failure mode, and the result of the experiment shows a prevalence of adhesive failures, so it is important to emphasize the importance of being more concerned with the cementation stage, mainly improving the adaptation of the post to the canal, using FGP reanatomization techniques with composite resins or the use of devices such as posts and sleeves.
A limitation of the Splendor Sap system may be associated with the number of interfaces, which is higher when compared to conventional posts since its design has a post associated with a fiberglass sleeve. Bubbles that can be introduced into the cement layer as a result of technical insertion, causing inadequate cement insertion, are contributing factors that can affect the quality of the luting [23]. Therefore, tests that allow the evaluation of adhesive interfaces, such as studies on the analysis of the interface using the micro-computed tomography (micro-CT) technique, proved to be an option to be used in future studies, as it enables visualization of three-dimensional and high-resolution images, through the digital union of hundreds of cross-sections.
This study has limitations in its application and design. Although the results show that the Splendor system presents relevant bond strength values when compared to the other FGP systems tested, the increase in an adhesive interface between the post and the fiberglass sleeve may lead to greater bubble formation and influence long-term bond strength. The use of bovine teeth was chosen for this study because it facilitates the standardization of samples, limiting the influence of factors other than those under study on the results.
CONCLUSION
Based on the results of this study, it was concluded that:
• The posts associated with the sleeve were effective, as they presented levels of adhesive strength like the conventional anatomization of the FGP, which may be associated with a better adaptation created in the coronal third, reducing the cementation line.
• This study suggests that, in relation to bond strength, the use of this new FGP system may be clinically useful for the rehabilitation of endodontically treated teeth.
• The fiberglass posts associated with the fiberglass sleeve can be applied in wide or narrow canals and are a good option to facilitate the clinical application of fiberglass posts.
AUTHOR'S CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| PBS | = Push-out Bond Strength |
| FGP | = Fiberglass Posts |
ETHICAL STATEMENT
We declare for due purposes, that the project entitled "Evaluation of the bond strength and interfacial characteristics of conventional fiberglass pins and associated with fiberglass gloves, in enlarged and non-enlarged roots", does not directly manipulate live animals for the collection of biological samples. Thus, because it does not violate the ethics related to animal experimentation and, being in accordance with federal legislation, Law No. 11,794, of October 8, 2008, there is no need for appreciation and approval by the Ethics Committee on the Use of Animals CEUA.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
FUNDING
This study was funded by Coordination for the Improvement of Higher Education Personnel – Brazil (CAPES) under Finance code 001, with additional support from the National Council for Scientific and Technological Development – Brazil (CNPq; National Institutes of Science and Technology (INCT) – Oral Health and Dentistry, Goias', Brazil (Grant number: #406840/2022-9).


