All published articles of this journal are available on ScienceDirect.
Wear Assessment of Novel PEEK Telescopic Attachment for Implant-Retained Mandibular Overdenture: A Clinical Trial Study
Abstract
Background
The wear of Zirconia-PEEK telescopic attachments can affect the retention of the implant-retained complete mandibular overdenture.
Aims
This study aimed to assess Zirconia-PEEK wear versus cobalt-chromium-PEEK telescopic attachments for the implant-retained complete mandibular overdenture.
Methods
Twelve completely edentulous patients were randomly chosen for implant-retained telescopic overdentures construction and divided into two groups, where group I was a patient with zirconia copies, and group II was with a cobalt-chromium CoCr copy. The PEEK was constructed for both groups as a secondary coping telescopic attachment for the denture. The wear measurements of PEEK were performed optically by using a USB digital microscope with a built-in camera connected to a compatible personal computer at different intervals of baseline, 3, 6, and 9 months. The data were statistically analyzed and compared using Student t-test, ANOVA, and Post Hoc Test.
Results
The statistical data revealed that groups II and I, in comparison, showed a non-significant difference in topographic features (RMS) of PEEK at different intervals of baseline, 3, 6, and 9 months.
Conclusion
Within the limitations of the study, there was no significant difference between combining Zirconia-PEEK or CoCr-PEEK for telescopic overdenture procedures. Therefore, it is advisable esthetically and biomechanically to apply Zirconia-PEEK procedures instead of CoCr-PEEK to produce metal-free dental telescopic overdenture.
1. INTRODUCTION
Telescopic attachments with overdentures were described as crown and sleeve coping or double crowns. The copy cemented to the abutment was identified as an inner or primary telescopic coping, and which, connected to a detachable prosthesis or dentures, was an outer or secondary coping. Many studies have recommended the application of telescopic attachments for retaining the overdentures due to the ability to transmit the occlusal load along the long axis of abutments and contribute guidance and protection against dislodging forces with improved support [1-3].
Regarding the material of copy construction, cast metal cobalt chromium (CoCr) restorations were commonly used with considerable success unless the demand for highly esthetic restorations requires applying metal-free restorations [4]. So, efforts were directed at developing high-strength ceramics with improved marginal quality, esthetics, and wear properties, such as Zirconia and PEEK [5-8].
The PEEK is an aromatic, polycyclic thermoplastic semi-crystalline high-performance polymer (HPP) with superior wear resistance, great processability, inertness, high strength, and modulus of elasticity [9, 10]. It was retained at high temperatures and is suitable as an alternative dental material for metal, zirconia, glass, and CoCr with ceramics [11-13].
In prosthetic dentistry, PEEK is used to fabricate temporary implant abutments, endo crowns, interim restorations, fixed dental prostheses, and removable dental partial prostheses by either using computer-aided design and computer-aided manufacturing (CAD-CAM) or pressing techniques [14-16]. These materials simplified clinical procedures in complex cases with loss of vertical dimension of occlusion that may affect the efficiency of neuromuscular esthetics and impair mastication [17-21].
The abrasive wear of the dental material is a damage caused by the change in temperature of the oral cavity. Therefore, the stress concentration that cyclic tempe- rature changes generated on the resin may cause the resin matrix to become exposed and the filler to dislodge, causing wear. The applied tests have shown that the PEEK material was resistant to up to 1200N of chewing force [22].
According to previous research, when Zirconium and PEEK abutments were compared, there was deformation in the PEEK abutments, while no breakage was encoun- tered in the Zirconium abutments [23]. Consequently, these problems in the denture prosthesis can be avoided because the PEEK abutment copy can easily change, and the same prosthesis is used again. The previous study stated that no breakage was determined in 40% of prostheses applied over PEEK abutments [24, 25].
The hypothesis of this clinical study suggests that the PEEK has a similar considerable wear resistance to zirconia and CoCr for fabricating double crown attachment for telescopic overdenture procedures due to its biocompatibility. Despite significant research efforts, it is still impossible to state that unique material exists to satisfy all the physicians' needs.
Since limited data are available regarding the clinical evaluation of wear for PEEK as a material of telescopic attachment, the current study has been conducted to assess the surface topography of PEEK telescopic attach- ment over Zirconia and CoCr copies for the implant-retained complete mandibular overdenture.
2. MATERIALS AND METHODS
This study represents a randomized clinical trial approved ethically under the No. (EC Ref No.: FDAzUC-REC_740/306) from the Research Ethics Committee, Faculty of Dental Medicine, Al Azhar University, Egypt. The presentation of this clinical study has been registered and publicly figured at clinical trial.gov PRS for protocol registration and results system under ID NCT06434142 University and conducted following the CONSORT checklist.
Twelve completely edentulous male patients aged 55 to 65 years were randomly chosen. The patients with Angle`s class I maxillofacial relationship were included in the study and free from any systemic diseases that might affect implant placement and bone resorption. Patients with radiotherapy, chemotherapy, uncontrolled diabetes, Heavy smokers, and parafunctional habits, such as bruxism or clenching, were excluded. Furthermore, female patients were excluded from the study to avoid the effect of hormonal disturbance.
The sample size of 12 patients was divided into two groups (6 per group) obtained using a two-sample t-test for independent samples with calculated evidence for α=0.05 and a confidence power of 0.03%, assuming a normal distribution [26]. The patients were selected from the Removable Prosthodontics Department Clinic, Faculty of Dental Medicine. After clarification of the technique before study enrolment, informed consent was obtained from all participants.
For each patient, an acrylic complete denture was constructed according to the conventional steps of complete denture construction with bilateral balanced occlusion. The denture was placed in the patient's mouth, and the stability, retention, occlusion, high points, and any sharp or overextended areas that might cause discomfort were examined. Post-insertion instructions were given, follow-up visits were scheduled, and patients were advised to wear their dentures until they were comfortable with them. Cone beam computer tomography was used to assess the height of the mandibular alveolar ridge, the kind of bone, and the quality of the bone. Cross-sectional measurements were made between the mandible's most inferior point and the crest of the ridge's highest point [27].
Following the two-stage surgical protocol, two dental implant fixtures (Oxy, Italy) with a length of 10 mm and a diameter of 3.7 mm were inserted at the canine area of the mandibular alveolar ridge. Depending on the attachment used, patients were randomly divided into two groups, and each group included six patients in the study. Group I (study group) was the group of patients with zirconia as a primary coping that attaches to the abutment and PEEK as a secondary coping telescopic attachment attached to the fitting surface of the denture. Group II (control group) was the group of patients with cobalt chromium (CoCr) as primary copings attached to the abutment and PEEK as a secondary coping’s telescopic attachment attached to the fitting surface of the denture, as shown in Fig. (1).
For the primary telescopic crown construction that attaches to the abutment, the primary crowns were designed with special software after ensuring a common path of insertion, as shown in Fig. (2aand b). The primary crowns were designed with certain requirements for their 5mm height (2mm gingival height was parallel, and the occlusal 3mm was tapered 4°). The data of computer numeric control (CNC) were transmitted to the milling machine and connected to the CAD system for milling the primary crowns of semi-sintered zirconia (Zirconia Katana) in group I and from CoCr in group II. After milling, going through rounds, and polishing, the line angles of the primary crowns were performed to avoid the presence of any edges or sharp corners. Finally, the polishing of the primary crowns was done using a special polishing paste (Spofa Dental, A Kerr Company, 5704624, Czech Republic).
After the primary crowns were constructed, they were tried intraorally for Zirconia (Fig. 3a) and CoCr (Fig. 3b). Then, they were returned to the cast, and the outer surface of the cast and primary copings were sprayed with a thin layer of scan spray (Enamelite, Keystone Industries) before scanning the cast and each primary coping separately to improve the data quality. The parameters used for designing the secondary crowns had minimal wall thickness and parallel walls, and they were built between the primary and secondary crowns. Mechanical projections were integrated into the design of each secondary crown to allow the secondary copings to interface mechanically with the denture base material, as shown in Fig. (4a). The data were finally transferred to the milling machine to mill the secondary crowns from PEEK.
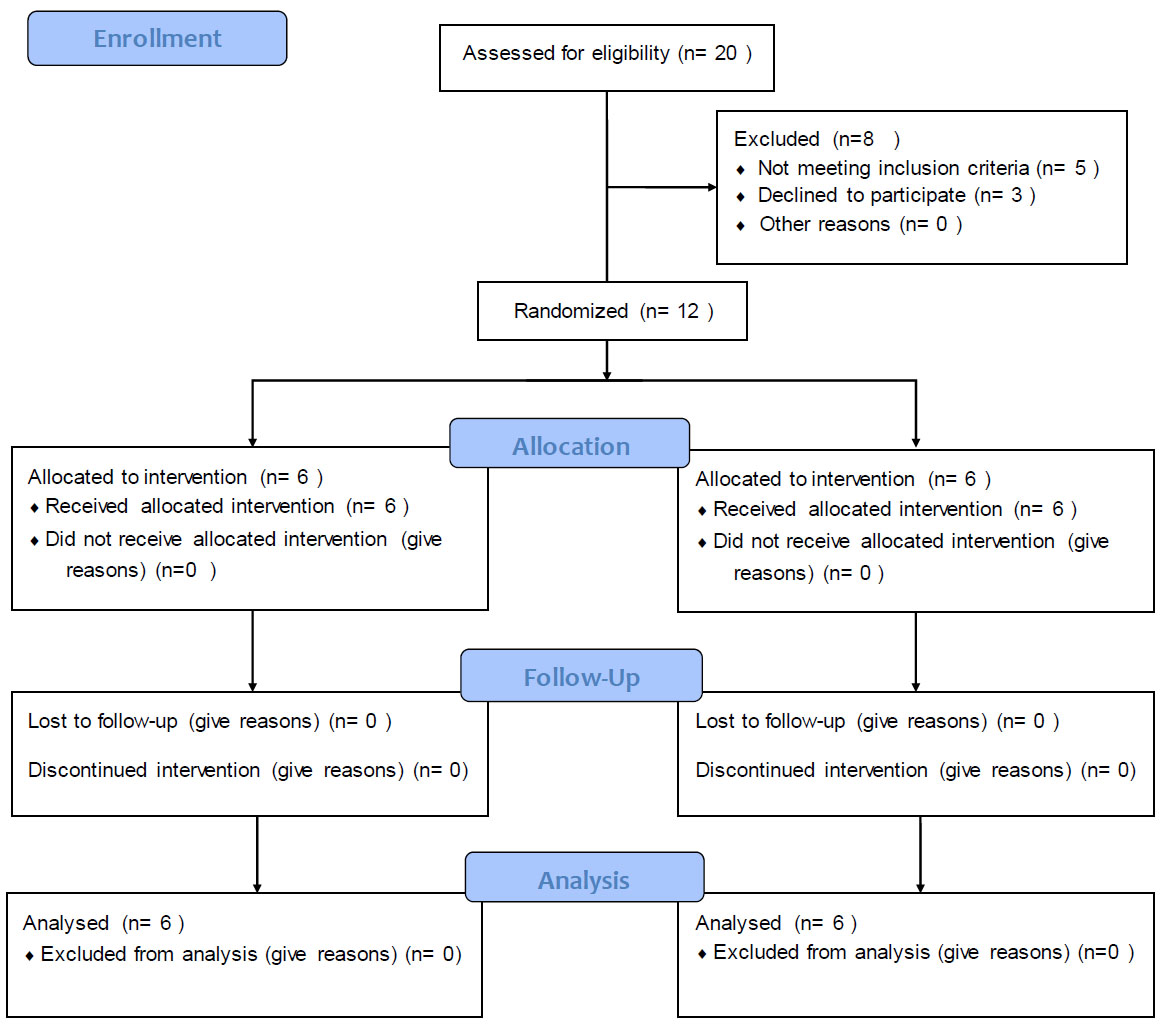
CONSORT flow chart of the study.
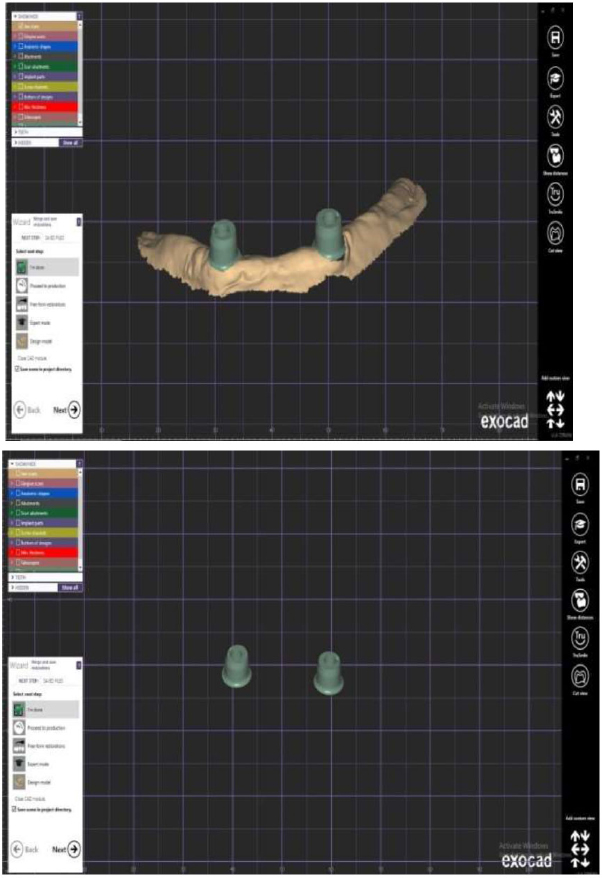
(a, b) The primary crowns were designed with special software.

Zirconia primary crown.

Cobalt chromium primary crown.
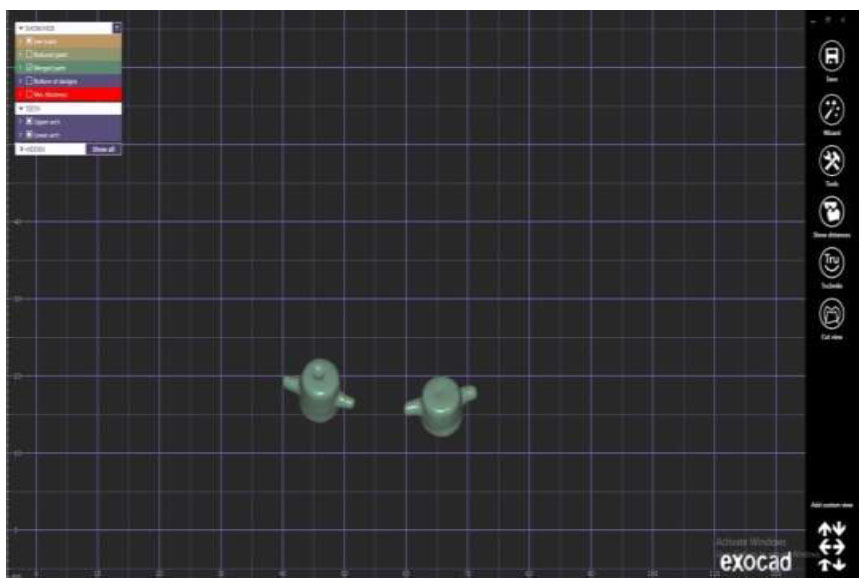
Designing of secondary crowns with mesial and distal projections.

Fitting of the secondary crowns over the primary ones.
The abutment of the implant was secured in the patient's mouth, with primary coping using cement. Then, secondary crowns were placed above the primary ones along the intended insertion path, as shown in Fig. (4b). For picking up the secondary copy, venting holes were prepared in the fitting surface of the mandibular overdentures, as shown in Fig. (5a). An auto-polymerized acrylic resin was used to pick up the secondary crowns and attach them to the overdenture's fitting surface as shown in Fig. (5b). Extra auto-polymerized acrylic resin material was removed using a diamond bur on a low-speed headpiece.

Venting holes in the fitting surface.

Direct incorporation of outer PEEK coping in the overdenture.
For wear measurements, the optical methods tend to fulfill the need for quantitative characterization of surface topography without contact with easier access, afford- ability, and reduced time [28]. Optical imaging of the samples was taken using a USB digital microscope with a built-in camera connected to a compatible personal computer at a fixed magnification power of 75X. This was done at baseline (before use) and then after 37500, 75000, and 150000 chewing cycles. In addition, the insertion removal test was done after 360, 720, and 1440 cycles. These chewing cycles corresponded to 3 months, 6 months, and 9 months of use, respectively, as shown in Fig. (6).
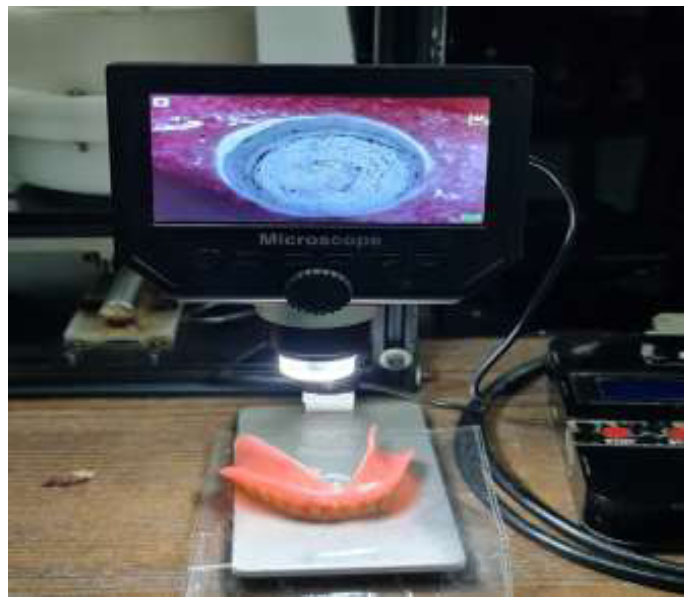
Evaluation of wear by USB digital microscope.
The image acquisition system was used to capture the pictures with a digital camera (U500x Digital Microscope, Guangdong, China) with 3 Mega Pixels of resolution, placed vertically at a distance of 2.5 cm from the samples. The angle between the lens axis and the illumination source was approximately 90°. Illumination was achieved with eight LED lamps (Adjustable by Control Wheel), with a color index close to 95%. The images were taken at a maximum resolution of 1280x1024 pixels per image and connected to an IBM-compatible personal computer using a fixed magnification of 120X.
Microsoft Office Picture Manager was used to trim digital microscope pictures to 350x400 pixels to specify and standardize the area of roughness assessment. The cropped images were analyzed using WSxM software [29]. All limits, sizes, frames, and measured characteristics were represented in pixels inside the WSxM program. Consequently, system calibration was carried out to translate the pixels into precise real-world units. Calibration was made by comparing an object of known size (a ruler in this study) with a scale generated by the software. Subsequently, a 3D picture of the object's surface profile was created. Three-dimensional images were collected for each sample in the clip area and the sides at an area of 10x10µm. This area was chosen based on the dimension of the typical bacteria expected to adhere to the restoration surface in vivo [30]. WSxM software was used to determine topographic features expressed by root mean square (RMS) and peak-to-peak measured in μm, which can be assumed as reliable indices of surface wear [31].
The Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp). The Shapiro-Wilk test was used to verify the normality of the distribution, and quantitative data were described using range (minimum and maximum), mean, and standard deviation. The significance of the obtained results was judged at the 5% level.
The statistical data were analyzed using the Student t-test for normally distributed quantitative variables to compare between two studied groups, the ANOVA test with repeated measurements for normally distributed quantitative variables to compare between more than two periods or stages, and the Post Hoc test (adjusted Bonferroni) for pairwise comparisons. The significance level was set at P ≤ 0.05.
2.1. Clinical Relevance
The wear of complete overdenture telescopic copies is the main factor of prosthesis retention loss, so it is important to distinguish the appropriate material with minimal wear. The wear resistance of the telescopic copies of the implant retained mandibular overdenture can be enhanced by incorporating Zirconia-PEEK copies.
3. RESULTS
The statistical data were analyzed, as shown in Table 1 (Fig. 7), which showed the mean wear values for the two groups. Throughout each of the follow-up periods, there was no statistically significant difference between the two groups. In topographic features, the Root Mean Square (RMS) for intragroup comparison, the CoCr group showed a non-significant difference in topographic features (RMS) at baseline during 3, 6, and 9 months (0.290 ± 0.001, 0.291 ± 0.001, 0.291 ± 0.001 and 0.291 ± 0.0), respectively with p=0.113. In addition, the Zirconia group showed a non-significant difference in topographic features (RMS) at baseline, during 3, 6, and 9 months (0.290 ± 0.001, 0.292 ± 0.001, 0.291 ± 0.001 and 0.291 ± 0.001), respectively with p=0.061. (Fig. 7)
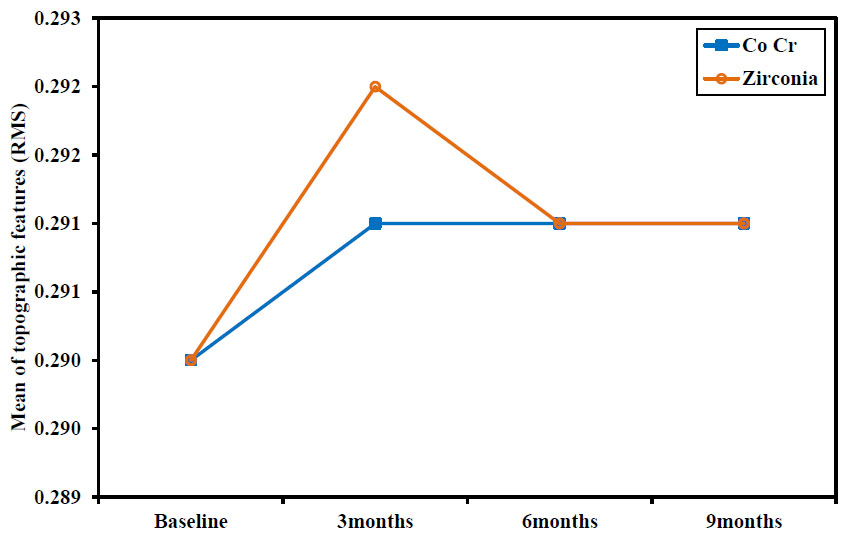
Comparison between the different studied periods according to RMS.
| Topographic features (RMS) | Baseline | 3 Months | 6 Months | 9 Months | F | P |
|---|---|---|---|---|---|---|
| Co Cr (n = 6) | - | - | - | - | - | - |
| Min. – Max. | 0.288 – 0.291 | 0.290 – 0.293 | 0.290 – 0.292 | 0.291 – 0.292 | 2.356 | 0.113 |
| Mean ± SD. | 0.290 ± 0.001 | 0.291 ± 0.001 | 0.291 ± 0.001 | 0.291 ± 0.0 | ||
| Zirconia (n = 6) | - | - | - | - | - | - |
| Min. – Max. | 0.288 – 0.291 | 0.290 – 0.293 | 0.290 – 0.292 | 0.290 – 0.292 | 3.447 | 0.061 |
| Mean ± SD. | 0.290 ± 0.001 | 0.292 ± 0.001 | 0.291 ± 0.001 | 0.291 ± 0.001 |
SD: Standard deviation.
F: F test (ANOVA) with repeated measures.
P: p-value for comparing between the studied periods.
4. DISCUSSION
This study was conducted to evaluate the wear measurement for Zirconia-PEEK and cobalt chromium-PEEK telescopic attachment systems for two implant-retained complete mandibular overdentures with the optical method. The results have justified the hypothesis that the Zirconia-PEEK crowns initially have lower wear values than cobalt-chromium-PEEK crowns, with differences not considered statistical significance. This may explain the different coefficients of thermal expansion and surface roughness of zirconia and PEEK, which cause changes in the fit and friction between the crowns.
The implant-retained mandibular overdenture was used in this study, and the telescopic attachment was selected because it provided support and retention and allowed the prosthesis to be restored without necessitating the reconstruction of the entire superstructure. The primary and secondary crowns form a telescoping unit, and the secondary crown acts as an anchor for the rest of the dentition [32-35].
In this present study, Zirconia was used as the primary crown material in group I due to its good biocompatibility, mimic tooth color, wear resistance, and lower thermal conductivity than metal [3]. In comparison, group II, formed from CoCr, was used as a primary crown, which is very well suited for the double crown technique due to its precise, high elastic modulus and mechanical strength. CoCr has a lower density, excellent biocompatibility, and corrosion resistance, and it may be cast or machined using CAD/CAM [36].
The wear is one of the major side effects of attachment techniques for implant overdenture that may occur after a usage period with subsequent reduction of prosthesis retention values. Detecting the wear of different dental materials and measuring its rate either in clinical or laboratory conditions are important to distinguish inappropriate material that may lead to rapid retention and loss of the implant overdenture [37].
Consequentially, the suggested optical technique of wear measurement by using a USB digital microscope often meets the demand for non-contact quantitative surface topography characterization [38-40]. According to this suggested measure, the results of the present study have revealed that the wear of the CoCr group at baseline, 3 months, 6 months, and 9 months was 0.291 ± 0.000, but for the Zirconia group, it was was 0.291 ± 0.001. Therefore, the difference was statistically non-significant. These results are in agreement with the findings of Fischer et al. [41], who stated that the retention forces in the telescopic systems where the primary crowns were made of zirconia registered the highest values compared to those with CoCr primary crowns. Additionally, for the zirconia telescopic primary crowns, the development of the retention forces and wear resistance throughout the 360 cycles (equated to one year of system operation) was favorable, as shown in Fig. (6).
Emera et al. [26, 35] investigated and compared the wear of telescopic attachments constructed from all zirconia, all-PEEK, and zirconia-PEEK telescopic attach- ments by evaluating surface changes using a Scanning Electron Microscope (SEM), and they concluded that significant wear in all groups after simulating six months with lesser surface topography changes for all-PEEK and all-Zircon attachments. The finding is that the group of Zirconia primary crowns and PEEK secondary crowns recorded the least stress values offered by PEEK secondary coping in combination with the harder ZrO2 primary one. This effect is explained by the cushioning effect and elastic modulus, which absorb occlusal forces and wear like a natural tooth.
Furthermore, the limitations and clinical implications of the study were related to two reasons; first includes the oral environment factors that affect the eligibility of the results, such as the saliva and temperature of the mouth effect. The second is the eligibility for intraoral measuring directly from the mouth of the patient. Therefore, these measurements were performed after removing the denture from the patient's mouth and then were submitted for an optical illusion measure with the microscope for PEEK copy.
CONCLUSION
Within the limitations of the current study, there was no significant difference in wear resistance between combining Zirconia-PEEK or CoCr-PEEK for telescopic overdenture procedures. Therefore, it is advisable esthetically and biomechanically to apply Zirconia-PEEK procedures instead of CoCr-PEEK to produce more successful implants with metal-free dental telescopic overdenture.
AUTHORS’ CONTRIBUTIONS
M.Q: Study conception and design; W.B: Data collection; MM: Data analysis and interpretation of results; HM: Draft manuscript preparation.
LIST OF ABBREVIATIONS
| CoCr | = Cobalt chromium |
| HPP | = High-performance Polymer |
| CNC | = Computer numeric control |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study represents a randomized clinical trial approved ethically under the No. (EC Ref No.: FDAzUC-REC_740/306) from the Research Ethics Committee, Faculty of Dental Medicine, Al Azhar University, Egypt.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.


