All published articles of this journal are available on ScienceDirect.
The Influence of Different Factors on Shade-Taking Accuracy Using Digital Shade Guide
Abstract
Background
Despite developments in dental shade selection methods, shade selection is still a challenge affecting aesthetic outcomes. Accurate color evaluation is an important factor in dental restoration procedures. An accurate determination of tooth color is crucial for obtaining a definitive result.
Aim and Objective
This study aimed to evaluate the factors affecting the shade-taking accuracy of digital shade-taking devices. The objective was to evaluate the effect of distance, contact angle, moisture condition, and surrounding light on the shade-taking accuracy of two digital shade-taking devices.
Materials and Methods
Bovine teeth were used and thawed in running tap water. The soft tissue remnants are cleansed using a scalpel and polished using 1500 SiC. The shade and color parameters ∆E were recorded at different distances, angles, moisture, and surrounding light.
Results
One-way ANOVA showed a statistically significant color shifting at 2mm and 3mm measuring distance for both devices (p<0.05). A contact angulation of 150, 300, and 450 significantly shifted the color measurement by both devices(p<0.05). In the case of moisture, both devices showed color shifting in certain conditions, however, VITA5 was less affected by the moisture. In the case of surrounding lightness, adding dental unit light significantly shifted the color parameter for VITA5 (p= 0.004), however, it was statistically insignificant for VITA4 (p=0.537)
Conclusions
The distance, angulation, moisture, and surrounding light can affect the shade-taking accuracy of the digital shade guide. The clinician must maintain a standard condition to accurately take shade using a digital shade guide.
1. INTRODUCTION
The palette of tooth colors is a symphony of shades, ranging from the purest of whites to the subtlest ivory to undertones of yellows, grays, and sometimes even hints of blue. This variation is a result of numerous factors, both intrinsic and extrinsic, that interplay to create a unique signature within each person's smile [1]. Intrinsic factors encompass the innate composition of teeth. The dentin, the inner layer beneath the enamel, holds the primary influence on tooth color. Its varying thickness and inherent hues influence the overall appearance, peeking through the translucent enamel. Genetics plays a decisive role here, dictating the natural tint and translucency of one's teeth [2]. Extrinsic elements, however, are equally influential. Lifestyle choices, dietary habits, and oral hygiene practices leave their mark on tooth color. Consuming pigmented foods, such as berries or coffee, and indulging in habits like smoking or inadequate dental care gradually stain the enamel, altering the natural coloration. The accumulation of these external factors over time may lead to discoloration or changes in shade [3].
Achieving a restoration that seamlessly blends with the natural dentition involves a meticulous understanding of tooth color [4]. The challenge for restorative dentistry lies in replicating this diversity with precision and finesse. The importance of accurate tooth color matching transcends mere cosmetic appeal [5]. A restoration that mirrors the natural teeth not only enhances aesthetics but also contributes significantly to the patient's self-confidence and psychological well-being. A mismatched restoration can stand out conspicuously, causing discomfort and self-consciousness, diminishing the intended functional and aesthetic benefits [6]. Inadequate color matching can lead to visible discrepancies over time as restorative materials age or respond differently to environmental factors, compromising the overall appearance and integrity of the dental work [7]. The artistry of color matching, therefore, extends the life and efficacy of the restoration.
Technological advancements have revolutionized the field of tooth color matching in restorative dentistry. Spectrophotometers, digital imaging, and shade guides have become indispensable tools, aiding in the precise measurement and replication of tooth color. These tools, coupled with the expertise and artistry of the dental practitioner, enable a more accurate and consistent restoration process [8]. However, achieving a perfect match involves more than technological prowess. It demands a blend of scientific knowledge, artistic skill, and a nuanced understanding of the patient's expectations and desires [9]. It requires the dentist to consider not just the color but also the texture, translucency, and surface characteristics of the natural teeth.
Technological advancements have brought forth digital tools that revolutionize shade-taking. Devices such as spectrophotometers and intraoral cameras capture precise digital images of the teeth, allowing for objective color measurement [10]. The software analyzes these images and generates a digital shade map, enhancing accuracy and reducing human error [11]. Digital methods offer consistency and reproducibility, which are particularly beneficial in complex cases [12]. Despite being user-friendly and superior in shade-taking accuracy, digital shade-taking is not beyond an error.
In view of several previous studies on the accuracy of the digital shade-taking devices, the accuracy was reported between 67-93% [13]. The variation in shade-taking accuracy reported in different articles may be due to the technical differences among the devices used in those studies. However, it remains a mystery whether the shade-taking accuracy of the digital devices was influenced by the operator and environmental factors or not, which was the biggest limitation of the manual shade-matching technique. Considering this fact, it is essential to look back, and assess the possible influence of operator and environment-related factors on shade-taking accuracy using a digital shade guide.
The aim of this experimental study was to evaluate the influence of different operator and environment-related factors on shade-taking accuracy using digital shade guides. The specific objectives were to measure the color parameter alteration of the digital shade-taking device in different measuring distances, angulation, moisture, and surrounding light conditions. The null hypotheses tested in this study were: 1) There are no differences in color measurements following different measuring distances and angulation of the digital shade-taking devices. 2) There are no differences in color measurement following different moisture and surrounding light conditions using a digital shade-taking device
2. MATERIALS AND METHODS
2.1. Specimens and Device Preparation
This study protocol was reviewed and approved by the research and ethical committee of RAK Medical and Health Sciences University with the approval number RAKMHSU-REC-010-2022/23-UG-D. A total of 10 extracted bovine teeth free from cracks and unusual discoloration were used in this study. The teeth were thawed in running tap water and gently cleaned of soft tissue remnants using a scalpel. Enamel surfaces of the teeth were polished using 2000-grit silicon carbide paper to obtain a flat and smooth surface. The specimens were then mounted on a holder to keep them stable and parallel to the floor. Two digital shade-taking devices, VITA Easy Shade 4.0 and VITA Easy Shade 5.0, manufactured by VITA Zahnfabrik H. Rauter GmbH & Co.KG, were used in this study. The devices were fixed in a holder capable of precise angulation and distancing.
2.2. Data Curation
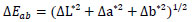
The devices were calibrated following manufacturer instructions. Furthermore, to evaluate the influence of measuring distance, the color parameters L*, C*, H*, a*, and b* of each specimen were recorded 3 times at 0mm, 1mm, 2mm, and 3mm distance from the specimen surface. Moreover, to evaluate the influence of measuring angulation, the color parameters of each specimen were recorded 3 times at 0-degree, 15-degrees, 30-degrees, and 45-degree angulation projecting incisally. In addition, to evaluate the influence of moisture condition of specimens, the color parameters were recorded 3 times in wet blot dry condition and after being air dried for 5 seconds and were kept inair dry conditions using a 3-way syringe maintaining constant distance and air pressure. Additionally, to evaluate the influence of surrounding light, the color parameters of each specimen were recorded 3 times in low light, daylight, and under dental unit light illumination conditions. Constant light intensity was maintained by measuring the light intensity adjacent to the specimen using a digital light measuring device (GAZELEE G9408). The test condition used in this study is shown in Fig. (1).
2.3. Color Alteration Measurement
The color parameters were inserted in Microsoft Excel. The color difference ΔEab was calculated using the following CIELab formula:
 |
Where ΔL* refers to the lightness difference in test condition (L*2- L*1), Δa* and Δb* refer to the chromaticity coordinates difference in test conditions (a*2- a*1) and (b*2- b*1).
2.4. Statistical Analysis
The color alteration data were analyzed using statistical software (SPSS 24.0, IBM, USA). The influence of each test condition was analyzed using One Way ANOVA, and multiple comparisons among the variables were analyzed using the Tukey post hoc test.
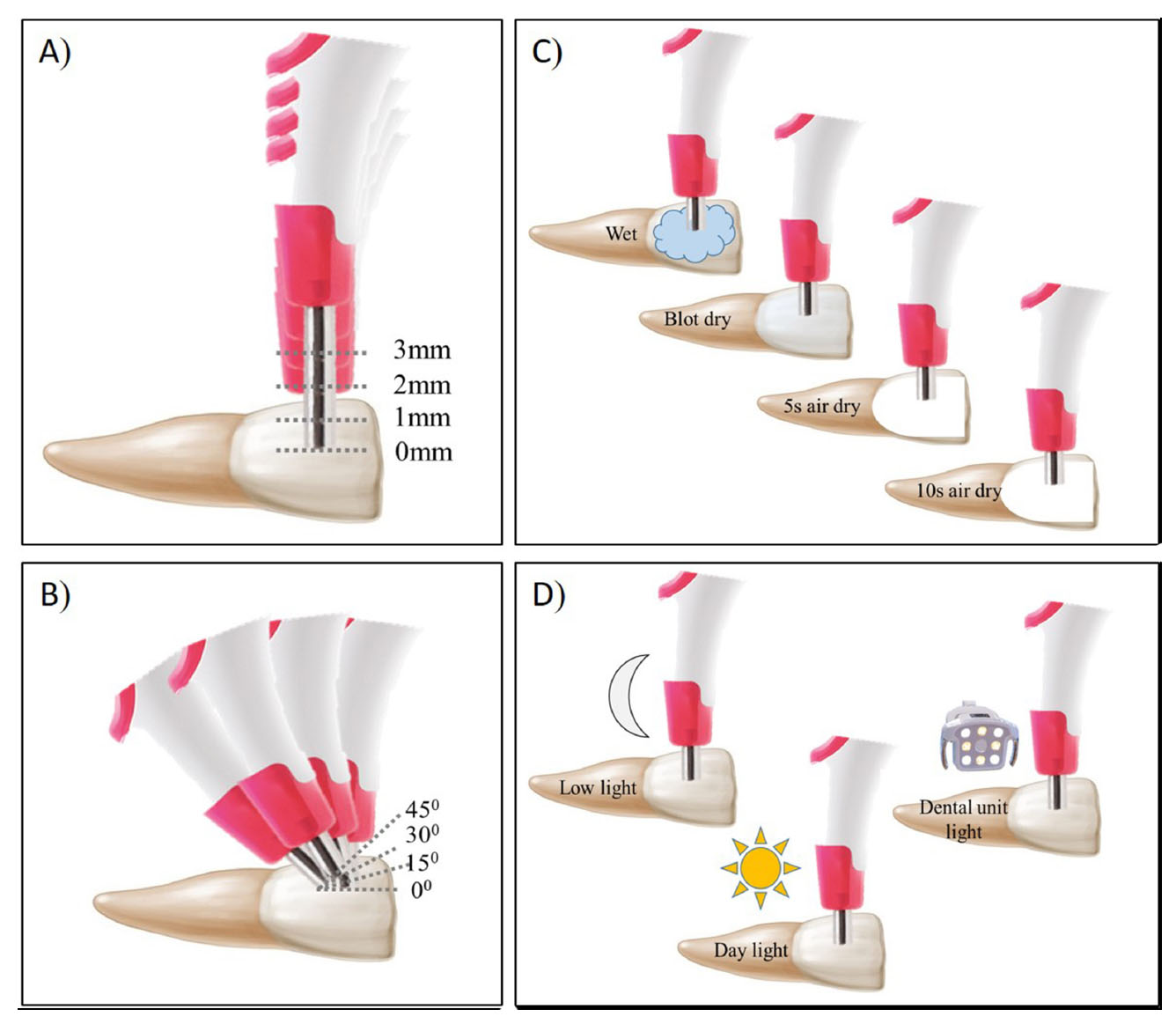
Illustration of different test condition; A) distances B) angulations C) moisture conditions D) Illuminations.
3. RESULTS
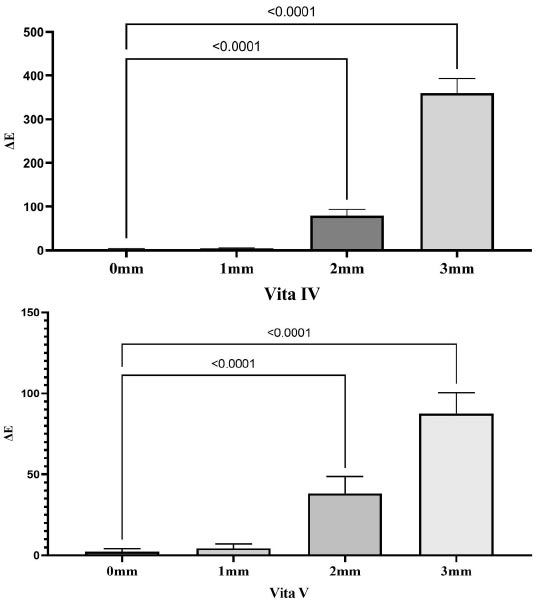
One-way ANOVA showed a significant effect of measuring distance on tooth color shifting using VITA 4.0 and VITA 5.0 devices (p<0.0001). Post hoc tests showed statistically significant color shifting in case of measuring a distance more than 1mm from the specimen for both devices (p<0.0001). The color-shifting value of both devices in different measuring distances is shown in Fig. (2). Similar to measuring distance, a significant effect of measuring angulation was observed on tooth color shifting using VITA 4.0 and VITA 5.0 devices (p<0.0001). Post hoc tests showed statistically significant color shifting in 15, 30, and 45-degree contact angle conditions for both devices (p<0.0001). The color-shifting value of both devices in different contact angles is shown in Fig. (3). With concern to the moisture condition, a significant effect of tooth moisture condition was observed on tooth color shifting using both the VITA 4.0 and VITA 5.0 devices (p<0.0001). Post hoc tests showed statistically significant color shifting in 5 seconds and 10 seconds air-dried groups compared to wet and blot dry conditions (p<0.05). A statistically significant color shifting was in wet and blotted dry conditions in the case of the VITA 4.0 device (p<0.001). The color-shifting value of both devices in different moisture conditions is shown in Fig. (4). The tooth color shifting was significantly influenced by the surrounding light condition for both devices (p<0.005). In the case of VITA 4.0, a statistically significant color shifting was observed between low light and daylight conditions (p= 0.004), however, the addition of dental unit light had an insignificant effect (p=0.537). On the contrary, color shifting was statistically significant between daylight and dental unit light conditions for VITA 5.0 (p=0.004), however, there was no significant difference between low light and daylight conditions (p=0.455). The color-shifting value of both devices in different surrounding light conditions is shown in Fig. (5). The ΔE value of all the test conditions is shown in Table 1.
Color alteration in different measuring distances.
Color alteration in different measuring angles.
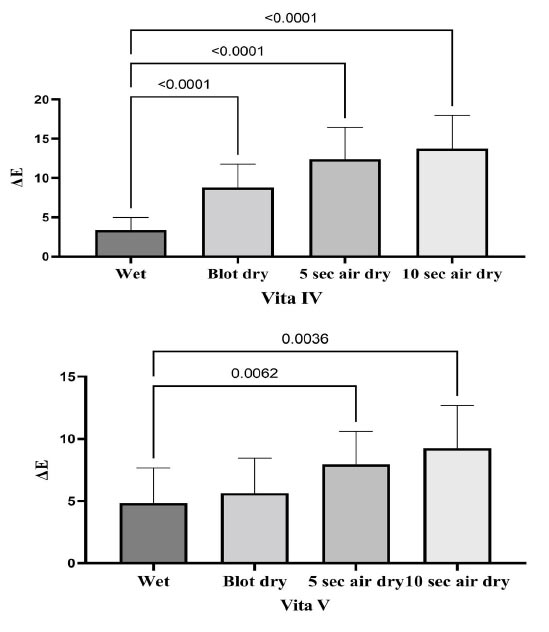
Color alteration in different moisture conditions.
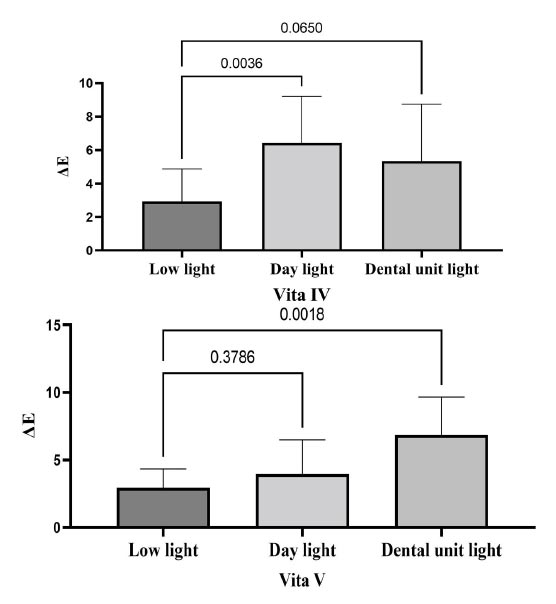
Color alteration in different light conditions.
| Distance | 0 mm | 1 mm | 2 mm | 3 mm | |
|---|---|---|---|---|---|
| ΔΕ | VITA 4 | 2.84 ± 1.5 a | 4.44 ± 1.2 a | 79.92 ±13.5 b | 359.82 ± 33.5 c |
| VITA 5 | 2.28 ± 2.1 a | 4.57 ± 2.5 a | 38.28 ±10.4 b | 87.69 ± 12.8 c | |
| Angulation | 0 degree | 15 degree | 30 degree | 45 degree | |
| ΔΕ | VITA 4 | 2.26 ± 2.1 a | 80.43 ± 15.1 b | 115.79 ± 18.4 c | 342.25 ±29.2 d |
| VITA 5 | 3.5 ± 1.5 a | 355 ± 32.9 b | 724.96 ± 39.6 c | 1213.3 ± 79.1 d | |
| Moisture | Wet | Blot dry | 5 Sec air dry | 10 sec air dry | |
| ΔΕ | VITA 4 | 3.41 ± 1.5 a | 8.77 ± 2.9 b | 12.35 ± 4.1 c | 13.72 ± 4.2 c |
| VITA 5 | 4.83 ± 2.8 a | 5.63 ± 2.8 ab | 7.96 ± 2.6 bc | 9.25 ± 3.5 c | |
| Illumination | Low light | Day light | Unit light | - | |
| ΔΕ | VITA 4 | 2.93 ±1.9 a | 6.42 ± 2.7 ab | 5.34 ±3.4 b | |
| VITA 5 | 2.94 ±1.3 a | 3.97 ±2.5 a | 6.85 ± 2.8 b | ||
4. DISCUSSION
The results of the current study showed that both the measuring distance and contact angle cause significant color shifting, thus, the first null hypothesis was rejected. The moisture condition of the tooth and surrounding light condition significantly affected the color accuracy thus the second null hypothesis was also rejected.
The study evaluated the impact of various factors on the accuracy of shade-taking using digital shade guides. Although there are several digital shade-taking devices available on the market, we limit the inclusion of two devices from the same manufacturer only to limit the effect of technical variation among different manufacturers. The basic mechanism working in a digital shade-taking device is to capture an image of the contact surface in the presence of specific light illumination projected from the tip of the device and then calculate the color parameters. The final shade that projects in the digital shade device has been calculated using the preset formula set by the manufacturer [14, 15]. In our study, a measuring distance of 0-1 mm did not cause significant color shifting, which rightfully allowed the clinician to use a protective sleeve or barrier to prevent contamination of the measuring tips. Moving the measuring tips more than 1mm away from the surface can significantly alter the color parameter. The projected light intensity can be altered by the interference of surrounding light due to the creation of a room by moving the tips away from the substrate surface following the Inverse square law [16]. Another explanation could be the view area that increased by moving the tips away from the surface [17].
In our study, a contact angulation of 15 degrees, 30 degrees, and 45 degrees significantly shifted the color measurement by both devices. Furthermore, to record a correct shade, the tip of the device needs to be parallel to the surface of interest and should be in 0-degree contact. There are several factors that are related to the contact angle. First, a contact angle of more than 0 degrees can scatter the projected light and reduce the intercity of reflecting light recorded by the sensor following Lambert’s cosine law [18]. Second, the Vita Easyshade device is designed to capture the color of the tooth at a specific point, known as the “measurement point.” Holding the device at an angle can cause a shift in the measurement point. Human teeth are a multi-chromatic structure, where the chroma increases from the incisal to the cervical direction [19, 20]. In our study, increasing the contact angle and projecting incisal reduced the chroma value of the tooth specimens. Finally, holding the device at an angle can also cause the camera to capture a wider area of the tooth surface, which can lead to variations in color and shading that are not representative of the specific area being measured [21].
As a result of moisture exposure, both devices displayed color shifting in certain circumstances.
When using the digital shade device to take shade measurements on teeth that are moist or have a wet surface, there are several factors to consider to ensure accurate results. Firstly, moisture can cause light to scatter, which can affect the accuracy of shade measurements. This is because the reflected light from the tooth surface can be dispersed in different directions, leading to variations in color perception [22]. Furthermore, to minimize the effects of moisture, it is important to blot and dry the tooth surface thoroughly before taking the shade measurement. This can be performed using absorbent materials such as cotton rolls or gauze. Overall, taking shade measurements with the digital shade device on a wet or moist tooth surface requires careful attention to detail and proper preparation to ensure accurate and consistent results [23]. While it is important to ensure that the tooth surface is blotted dry when taking shade measurements with the digital shade device, it is equally important to avoid drying the tooth or using the device on a completely dry tooth. When a tooth is over-dried or completely dry, the surface can become dehydrated and appear lighter in color than it actually is [24]. This can lead to inaccuracies in shade matching, as the shade captured by the device may not match the actual shade of the tooth [25]. Furthermore, to avoid these issues, it is important to use a gentle air-drying technique or absorbent material to remove excess moisture from the tooth surface without completely drying it out. This will ensure that the surface is dry enough for accurate shade matching but not so dry that it affects the color perception.
The surrounding lightness with the digital shade device can affect the accuracy of shade measurements. In this case, adding dental unit light can cause a shift in the color parameter of VITA 5.0, which can lead to inaccuracies in shade matching. This is because the dental unit light may have a different color, temperature, or intensity compared to the standardized lighting conditions used with the digital shade device, which can cause the color of the tooth to appear different and lead to variations in shade-matching results [26, 27]. Moreover, to minimize the effects of surrounding lightness and dental unit light, it is important to control the lighting conditions in the room as much as possible.
CONCLUSION
Based on the study findings, it was concluded that the shade-taking accuracy of a digital shade-taking device is affected by the measuring distance, measuring angle, moisture condition of the tooth, and the surrounding light condition. Moreover, to take an accurate shade using the digital shade-taking device, clinician is recommended to use zero contact distance and angulation between the tooth surface and the tip of the digital shade device. Additionally, the teeth should be blot dried, and the tooth shade should be taken in optimal daylight conditions.
AUTHOR’S CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study protocol was reviewed and approved by the research and ethical committee of RAK Medical and Health Sciences University with the approval number RAKMHSU-REC-010-2022/23-UG-D.
HUMAN AND ANIMAL RIGHTS
This study adheres to internationally accepted standards for animal research, following the 3Rs principle. The ARRIVE guidelines were employed to report experiments involving live animals and promote ethical research practices.


