All published articles of this journal are available on ScienceDirect.
Periodontal Status in Periodontitis Patients with Temporary Periodontal Splint: A Retrospective Study
Abstract
Background
Periodontitis, an inflammatory condition initiated by a number of particular microorganisms, damages the periodontal ligament, cementum, and alveolar bone, resulting in tooth mobility or even tooth loss. Periodontal splinting can be administered in adjunct to periodontal treatment by stabilizing tooth mobility. To the best of our knowledge, no strong evidence has been reported regarding the clinical data of tooth immobilization in periodontitis in order to optimize the outcome. Therefore, this retrospective study aimed to investigate the epidemiologic data and periodontal status of periodontitis patients who underwent the temporary periodontal splinting treatment.
Methods
Periodontal medical records in the dental hospital were collected within the past two years based on the inclusion criteria of this study. Medical records of patients with systemic disease and a history of periodontal surgery were excluded.
Results
Patients who received a temporary periodontal splint was more prevalent in females (70.2%), young elderly-age group (53.2%), patients with extra-coronal splint (55.4%), patients who had occlusal adjustment prior to the splint (51.8%), patients with good Oral Hygiene Index-Simplified (OHI-S) (75%), and Trauma from the occlusion (TFO) cases (45.2%). The damage that reaches the apical third of the dental root was 7%, the middle third of the dental root was 49.2%, and tooth #31 had the largest distribution with the most alveolar bone injury. The tooth #42 had the highest vertical pattern (7%) and horizontal pattern (62.8%) of alveolar bone damage.
Conclusion
In conclusion, temporary periodontal splint therapy has been conducted widely to support periodontal status.
1. INTRODUCTION
Periodontitis is an inflammatory condition brought on by a particular type of microbe that damages the alveolar bone, cementum, and periodontal ligament, which support the teeth. Increased depth in gingival probing and recession are symptoms of periodontitis [1]. This disease poses the greatest threat to the oral cavity and is one of the main causes of tooth loss [2-4]. This condition is not only often found in developing countries but is also common in developed countries. However, it is said that the prevalence of calculus deposits and bleeding on probing (BOP) is higher in developing countries [5]. Periodontitis can occur in various age groups, with a higher prevalence in adults and the elderly because the risk of periodontitis continues to increase with age [1, 6]. Based on the Indonesian Basic Health Research (RISKESDAS) 2018, the prevalence of periodontitis in Indonesia ranges from 73.1-75.0% [7]. This evidence shows a high number when compared to the global prevalence of periodontitis, according to Nazir M. (2017), which ranges from 20-50% of the world's population [3].
Dental plaque-induced-persistent inflammation may damage the periodontal tissues, which can be observed clinically as a loss of attachment [4]. The tooth will become more mobile as the attachment loss intensifies and the alveolar bone deteriorates. Both patient comfort and cosmetic issues may result from such tooth mobility. Tooth mobility will also be increased as a result of the unfavourable crown-root ratio, known as secondary trauma from occlusion (TFO) [8, 9]. The excessive mobility issues are treated with periodontal splints. By performing this therapy, occlusal forces are distributed from the movable teeth to the abutments of the adjacent teeth. As a result, it provides reattached periodontium stability and lessens movement-induced traumatic occlusion that makes loose teeth stay longer [10, 11].
According to the kind of device, periodontal splints (Fig. 1) can be categorized as fixed or removable, and according to the therapeutic approach, they can be temporary, provisional, or permanent [3]. Temporary periodontal splints are used in the beginning stage and during active periodontal therapy. They are worn for a shorter amount of time (up to 6 months). Permanent periodontal splints that are made of composite resins and put intra-coronal, on the other hand, are utilized when a tooth needs support over a longer period of time, often for years [10].
To the best of our knowledge, no strong evidence has been reported regarding the clinical data of tooth immobilization in periodontitis in order to optimize the outcome. Therefore, this retrospective study aimed to investigate the epidemiologic data and periodontal status of periodontitis patients who underwent temporary periodontal splinting treatment.
2. MATERIALS AND METHODS
All study designs and protocols were reviewed and approved by the Ethical Board Committee of the Universitas Indonesia (Number: 58/Ethical Approval/FKGUI/IX/2021). As a retrospective study, periodontal medical records in the Periodontology Specialist Clinic, Dental Teaching Hospital, were collected within the past two years (medical record time frame) based on the inclusion criteria of this study.
The inclusion of this study involved a complete medical record of periodontitis patients with a history of temporary periodontal splints. Medical records of periodontitis (Stage III-IV) patients who had several visits were included. Medical records of patients with systemic disease, incomplete records, patients who underwent periodontal surgery, and consisting of other types of temporary splints were excluded.
A sample was taken using the consecutive sampling approach on medical records that met the required requirements. The patient's periodontal status was determined by the tooth components that were treated. The age of the patient at the time of treatment, the clinical parameters, including OHI-S, TFO, tooth mobility, the degree of alveolar bone destruction, bone destruction pattern, and clinical attachment loss were considered. Further, A.J. collected the data under the supervision of B.S. and D.I.H. Statistical data processing software was used to analyze the research data using SPSS Ver.23 (IBM, Chicago, USA). The distribution was described using a univariate analysis.
3. RESULTS
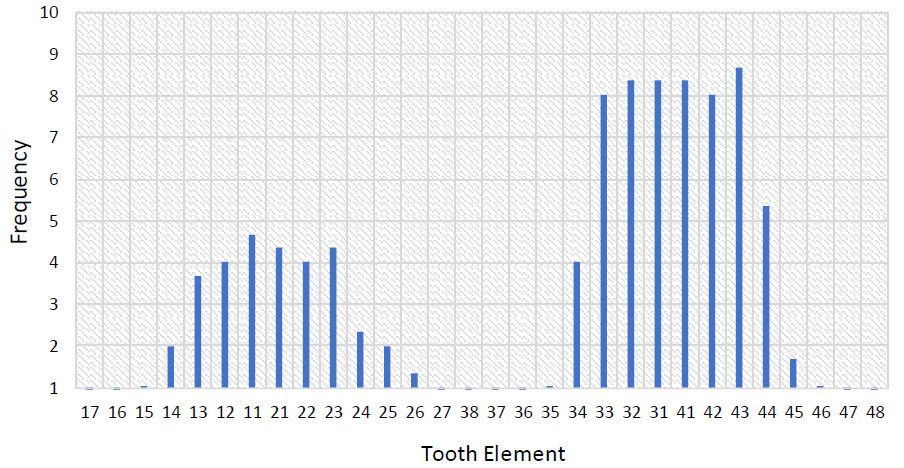
According to Table 1, from 47 medical records of periodontitis patients, the majority of patients receiving temporary periodontal splint treatment at the Clinic were women (70.2%). According to the data, the bulk of patients (53.2%) were between the ages of 46 and 55 or early elderly. Fig. (2) shows that temporary splint is mostly seen in the anterior mandible, compared to other regions.
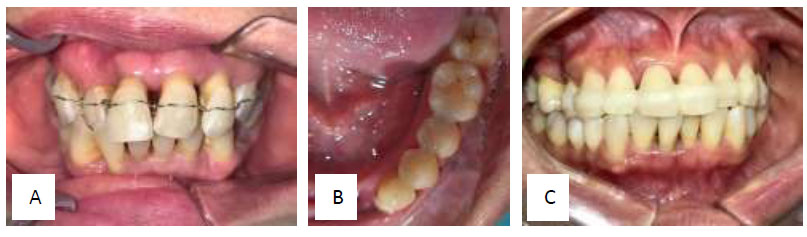
Periodontal Splint. (A) Wire temporary splint. (B) Intra-coronal permanent splint. (C) Fibres-reinforced composite resin splint. Courtesy of Department Periodontology, Faculty of Dentistry, Universitas Indonesia.
| Variable | N (%) |
|---|---|
| Gender | - |
| Male | 14 (29.8%) |
| Female | 33 (70.2%) |
| Age (year old) | - |
| 17 – 25 | 1 (2.1%) |
| 26 – 34 | 3 (6.4%) |
| 35 – 45 | 7 (14.9%) |
| 46 – 55 | 31 (53.2%) |
| 56 – 65 | 6 (12.8%) |
| > 65 | 5 (10.6%) |
| Splint type | - |
| Intra-coronal | 25 (44.6%) |
| Extra-coronal | 31 (55.4%) |
| Occlusal Adjustment therapy | - |
| Yes | 29 (51.8%) |
| No | 27 (48.2%) |
| OHI-S | - |
| Good | 42 (75%) |
| Moderate | 11 (19.6%) |
| Poor | 3 (5.4%) |
| Tooth Mobility | - |
| Yes | 187 (62.5%) |
| No | 112 (37.5%) |
| Alveolar bone destruction | - |
| Yes | 258 (86.3%) |
| No | 41 (13.7%) |
| TFO | - |
| Yes | 135(45.2%) |
| No | 164(54.8%) |
Extra-coronal splints were the most widely used kind of splint (55.4%). Of the 56 temporary periodontal splints applied in the initial phase, 29 were applied in conjunction with occlusal treatment adjustments. At the time of splinting, 75% of the patients had satisfactory OHIS. There were 187 teeth (62.5%) that were mobile at the time of splinting. According to the statistics, 135 teeth (45.2%) had TFO, and 258 teeth (86.3%) had alveolar bone deterioration.
The tooth components undergoing splint therapy are distributed by oral area in Table 2. With 149 teeth (49.8% of the total), the mandibular anterior region had the highest frequency, followed by the maxillary anterior region with 75 teeth (25.1%). The posterior mandible, which had 46 teeth (15.4%), had the third highest frequency. With a frequency of 29 teeth (9.7%), the posterior portion of the maxilla had the lowest frequency.
The frequency and distribution of the degree of tooth mobility in patients who received temporary periodontal splint therapy at the clinic are shown in Table 3. These statistics show that 92(49.2%) had degree 2 mobility and 62(33.2%) had degree 1 mobility, which are the mobility types that occur most frequently. The frequency of 33 (17.6%) was the lowest for mobility degree 3.
| Location (N = 299) | N (%) |
|---|---|
| Posterior Maxilla | 29 (9.7%) |
| Anterior Maxilla | 75 (25.1%) |
| Anterior Mandible | 149 (49.8%) |
| Posterior Mandible | 46 (15.4%) |
| Tooth | Mobility | |||||
|---|---|---|---|---|---|---|
| Grade 1 | Grade 2 | Grade 3 | ||||
| N | (%) | N | (%) | N | (%) | |
| 17 | 0 | 0% | 1 | 0.5% | 0 | 0% |
| 16 | 2 | 1.1% | 0 | 0% | 0 | 0% |
| 15 | 0 | 0% | 0 | 0% | 0 | 0% |
| 14 | 3 | 1.6% | 0 | 0% | 1 | 0.5% |
| 13 | 1 | 0.5% | 0 | 0% | 1 | 0.5% |
| 12 | 4 | 2.1% | 0 | 0% | 0 | 0% |
| 11 | 5 | 2.7% | 5 | 2.7% | 1 | 0.5% |
| 21 | 1 | 0.5% | 6 | 3.2% | 3 | 1.6% |
| 22 | 2 | 1.1% | 5 | 2.7% | 0 | 0% |
| 23 | 0 | 0% | 3 | 1.6% | 0 | 0% |
| 24 | 1 | 0.5% | 1 | 0.5% | 3 | 1.6% |
| 25 | 0 | 0% | 5 | 2.7% | 0 | 0% |
| 26 | 0 | 0% | 1 | 0.5% | 2 | 1.1% |
| 27 | 0 | 0% | 0 | 0% | 0 | 0% |
| 38 | 0 | 0% | 0 | 0% | 0 | 0% |
| 37 | 0 | 0% | 1 | 0.5% | 0 | 0% |
| 36 | 0 | 0% | 1 | 0.5% | 0 | 0% |
| 35 | 0 | 0% | 2 | 1.1% | 1 | 0.5% |
| 34 | 3 | 1.6% | 1 | 0.5% | 0 | 0% |
| 33 | 4 | 2.1% | 1 | 0.5% | 1 | 0.5% |
| 32 | 9 | 4.8% | 11 | 5.9% | 3 | 1.6% |
| 31 | 4 | 2.1% | 15 | 8.0% | 6 | 3.2% |
| 41 | 7 | 3.7% | 11 | 5.9% | 7 | 3.7% |
| 42 | 8 | 4.3% | 11 | 5.9% | 3 | 1.6% |
| 43 | 2 | 1.1% | 2 | 1.1% | 1 | 0.5% |
| 44 | 4 | 2.1% | 3 | 1.6% | 0 | 0% |
| 45 | 1 | 0.5% | 3 | 1.6% | 0 | 0% |
| 46 | 1 | 0.5% | 1 | 0.5% | 0 | 0% |
| 47 | 0 | 0% | 1 | 0.5% | 0 | 0% |
| 48 | 0 | 0% | 1 | 0.5% | 0 | 0% |
| Total | 62 | 33.2% | 92 | 49.2% | 33 | 17.6% |
| Tooth | Radiographic Bone Height | |||||
|---|---|---|---|---|---|---|
| Marginal Third | Middle Third | Apical Third | ||||
| N | (%) | N | (%) | N | (%) | |
| 17 | 0 | 0% | 0 | 0% | 1 | 0.4% |
| 16 | 0 | 0% | 1 | 0.4% | 0 | 0% |
| 15 | 1 | 0.4% | 1 | 0.4% | 1 | 0.4% |
| 14 | 0 | 0% | 2 | 0.8% | 3 | 1.2% |
| 13 | 3 | 1.2% | 4 | 1.6% | 1 | 0.4% |
| 12 | 2 | 0.8% | 7 | 2.7% | 2 | 0.8% |
| 11 | 0 | 0% | 6 | 2.3% | 6 | 2.3% |
| 21 | 0 | 0% | 6 | 2.3% | 4 | 1.6% |
| 22 | 2 | 0.8% | 7 | 2.7% | 1 | 0.4% |
| 23 | 3 | 1.2% | 5 | 1.9% | 2 | 0.8% |
| 24 | 1 | 0.4% | 1 | 0.4% | 3 | 1.2% |
| 25 | 2 | 0.8% | 1 | 0.4% | 3 | 1.2% |
| 26 | 0 | 0% | 1 | 0.4% | 2 | 0.8% |
| 27 | 0 | 0% | 1 | 0.4% | 0 | 0% |
| 38 | 0 | 0% | 0 | 0% | 0 | 0% |
| 37 | 0 | 0% | 1 | 0.4% | 0 | 0% |
| 36 | 0 | 0% | 1 | 0.4% | 0 | 0% |
| 35 | 0 | 0% | 1 | 0.4% | 2 | 0.8% |
| 34 | 2 | 0.8% | 4 | 1.6% | 1 | 0.4% |
| 33 | 3 | 1.2% | 10 | 3.9% | 5 | 1.9% |
| 32 | 1 | 0.4% | 9 | 3.5% | 15 | 5.8% |
| 31 | 1 | 0.4% | 6 | 2.3% | 18 | 7.0% |
| 41 | 1 | 0.4% | 10 | 3.9% | 14 | 5.4% |
| 42 | 1 | 0.4% | 13 | 5.0% | 9 | 3.5% |
| 43 | 3 | 1.2% | 16 | 6.2% | 2 | 0.8% |
| 44 | 2 | 0.8% | 8 | 3.1% | 2 | 0.8% |
| 45 | 0 | 0% | 2 | 0.8% | 3 | 1.2% |
| 46 | 0 | 0% | 1 | 0.4% | 2 | 0.8% |
| 47 | 0 | 0% | 1 | 0.4% | 1 | 0.4% |
| 48 | 0 | 0% | 1 | 0.4% | 0 | 0% |
| Total | 28 | 10.9% | 127 | 49.2% | 103 | 39.9% |
| Tooth | Alveolar Bone Loss | |||
|---|---|---|---|---|
| Horizontal | Vertical | |||
| N | (%) | N | (%) | |
| 17 | 1 | 0.4% | 0 | 0% |
| 16 | 0 | 0% | 1 | 0.4% |
| 15 | 3 | 1.2% | 0 | 0% |
| 14 | 2 | 0.8% | 3 | 1.2% |
| 13 | 4 | 1.6% | 4 | 1.6% |
| 12 | 8 | 3.1% | 3 | 1.2% |
| 11 | 5 | 1.9% | 7 | 2.7% |
| 21 | 5 | 1.9% | 5 | 1.9% |
| 22 | 8 | 3.1% | 2 | 0.8% |
| 23 | 8 | 3.1% | 2 | 0.8% |
| 24 | 4 | 1.6% | 1 | 0.4% |
| 25 | 2 | 0.8% | 4 | 1.6% |
| 26 | 0 | 0% | 3 | 1.2% |
| 27 | 1 | 0.4% | 0 | 0% |
| 37 | 0 | 0% | 1 | 0.4% |
| 36 | 1 | 0.4% | 0 | 0% |
| 35 | 1 | 0.4% | 2 | 0.8% |
| 34 | 4 | 1.6% | 3 | 1.2% |
| 33 | 12 | 4.7% | 6 | 2.3% |
| 32 | 17 | 6.6% | 8 | 3.1% |
| 31 | 14 | 5.4% | 11 | 4.3% |
| 41 | 16 | 6.2% | 9 | 3.5% |
| 42 | 18 | 7.0% | 5 | 1.9% |
| 43 | 15 | 5.8% | 6 | 2.3% |
| 44 | 7 | 2.7% | 5 | 1.9% |
| 45 | 2 | 0.8% | 3 | 1.2% |
| 46 | 1 | 0.4% | 2 | 0.8% |
| 47 | 2 | 0.8% | 0 | 0% |
| 38 | 0 | 0% | 0 | 0% |
| 48 | 1 | 0.4% | 0 | 0% |
| Total | 162 | 62.8% | 96 | 37.2% |
The distribution of alveolar bone loss in the areas receiving temporary periodontal splint therapy is shown in Table 4. Based on these findings, damage to the middle 1/3 of the alveolar bone accounts for the majority of cases (127; 49.2%) of alveolar bone damage. The injury to the apical 1/3 had the next-highest incidence, at 103 (39.9%). The frequency of damage up to 1/3 of the cervical spine was the lowest, at 28 (10.9%).
The distribution of bone damage patterns that occur in dental elements with radiographic bone degradation is shown in Table 5. According to these data, a total of 162 horizontal damage patterns (62.8%) and 96 vertical damage patterns (37.2%) have the highest frequency of damage patterns. With a total of 18 (7%), tooth 42 had the highest frequency of horizontal damage patterns, followed by tooth 41 with a total of 16 (6.2%). With a total of 11 (4.3%), teeth 31 had the highest frequency of vertical damage patterns, followed by teeth 41 with a total of 9 (3.5%).
The distribution of clinical attachment loss by dental components of patients who received a temporary periodontal splint is shown in Table 6. The table shows the frequency of loss. With a frequency of 23 (8.2%) by category of bad clinical attachment loss, tooth 31 had the highest frequency of clinical attachments. As shown in Fig. (2), tooth element 41, which has a frequency of 20 (7.1%) and falls under the category of poor clinical attachment loss, had the second-highest frequency. When severity levels were recorded, tooth element 33 had the highest frequency in the category of moderate clinical attachment loss with a total value of 4 (1.4%), and tooth element 33 also had the highest frequency in the medium category with a total value of 6(2.1%) value. The next highest frequency was in the category poor, which occurred in the tooth element 31 with a frequency of 23(8.2%).
| Tooth | Clinical Attachment Loss | |||||
|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | ||||
| N | (%) | N | (%) | N | (%) | |
| 17 | 0 | 0% | 0 | 0% | 1 | 0.4% |
| 16 | 0 | 0% | 0 | 0% | 1 | 0.4% |
| 15 | 0 | 0% | 1 | 0.4% | 2 | 0.7% |
| 14 | 0 | 0% | 1 | 0.4% | 5 | 1.8% |
| 13 | 2 | 0.7% | 2 | 0.7% | 4 | 1.4% |
| 12 | 0 | 0% | 2 | 0.7% | 8 | 2.9% |
| 11 | 0 | 0% | 1 | 0.4% | 12 | 4.3% |
| 21 | 2 | 0.7% | 1 | 0.4% | 10 | 3.6% |
| 22 | 1 | 0.4% | 4 | 1.4% | 5 | 1.8% |
| 23 | 1 | 0.4% | 3 | 1.1% | 8 | 2.9% |
| 24 | 1 | 0.4% | 1 | 0.4% | 5 | 1.8% |
| 25 | 0 | 0% | 1 | 0.4% | 5 | 1.8% |
| 26 | 0 | 0% | 1 | 0.4% | 3 | 1.1% |
| 27 | 0 | 0% | 0 | 0% | 1 | 0.4% |
| 38 | 0 | 0% | 0 | 0% | 1 | 0.4% |
| 37 | 0 | 0% | 1 | 0.4% | 0 | 0% |
| 36 | 0 | 0% | 1 | 0.4% | 1 | 0.4% |
| 35 | 0 | 0% | 0 | 0% | 3 | 1.1% |
| 34 | 1 | 0.4% | 1 | 0.4% | 9 | 3.2% |
| 33 | 4 | 1.4% | 6 | 2.1% | 13 | 4.6% |
| 32 | 1 | 0.4% | 5 | 1.8% | 19 | 6.8% |
| 31 | 0 | 0% | 2 | 0.7% | 23 | 8.2% |
| 41 | 1 | 0.4% | 4 | 1.4% | 20 | 7.1% |
| 42 | 0 | 0% | 3 | 1.1% | 19 | 6.8% |
| 43 | 1 | 0.4% | 5 | 1.8% | 16 | 5.7% |
| 44 | 1 | 0.4% | 2 | 0.7% | 11 | 3.9% |
| 45 | 0 | 0% | 1 | 0.4% | 4 | 1.4% |
| 46 | 0 | 0% | 0 | 0% | 3 | 1.1% |
| 47 | 0 | 0% | 0 | 0% | 2 | 0.7% |
| 48 | 0 | 0% | 0 | 0% | 1 | 0.4% |
| Total | 16 | 5.7% | 49 | 17.5% | 215 | 76.8% |
4. DISCUSSION
Forty-seven subjects who experienced temporary periodontal splint treatment in the past two years were observed. This study focused on the conveyance of patients' periodontal status based on tooth components. The results show that of the 47 subjects, the foremost age group was the early elderly (46-55 years old), to be specific, 53.2%. The most noteworthy recurrence was found in the late adult age group (34-45 years old), specifically 14.9%, and the late elderly age group (56-65 years old), specifically 12.8%. This is in agreement with national studies and others, which show that the most elevated recurrence of periodontitis happens between the age of 45-54 years old [12, 13].
Based on Table 1, it can be seen that the larger part of patients who experienced temporary periodontal splints utilized extra-coronal type (55.4%). Intra-coronal types were utilized very habitually, as much as 44.5%. This may be credited to the larger part of teeth that were splinted, specifically front teeth, where the intra-coronal splint could give a better value [10, 14, 15]. Based on Table 1, temporary periodontal splint frequently followed occlusal adjustment therapy with the value of 51.8%. This may be credited to occlusal adjustment therapy, where precise articulation information is required and will be troublesome to attain in hypermobility teeth [16].
Based on Table 2, tooth 43 had the most temporary periodontal splint (8.7%). Later, teeth 31, 32, and 41 showed an 8.4% value in each group, following teeth 33 and 42 with 8%. This might be due to the alveolar bone of the front teeth being thin and patients refusing to have their incisors extracted [17, 18]. Based on the distribution (Fig. 1), the front teeth of the mandible feature a recurrence of the most noteworthy mobility with 149 teeth (49.8%), continuing with the maxillary front area with 75 teeth (25.1%). The areas for the third-lowest and fourth-lowest frequencies individually were the mandibular back and maxillary back. This may be due to the more slender alveolar bone anteriorly and the mandibular teeth emitting more rapidly than the maxillary teeth [17, 18].
Based on the result shown in Table 3, the most noteworthy recurrence was portability degree 2 of 92 (49.2%), followed by portability degree 1 of 62 (33.2%). Mobility of 3 degrees had the most reduced recurrence of tooth #33 (17.6%). The most noteworthy portability recurrence was seen in tooth 31 with 15(8%) with degree 2 mobility, followed by tooth #32, 41, and 42 with the same recurrence 11(5.9%). Front teeth had the most elevated recurrence of all teeth, and this could be ascribed to incisor teeth, which have shorter roots. Hence, these teeth have lower resistance to versatility compared to other dental elements [18]. Grade 2 mobility is categorized as a flawed prognosis, in which, if treatment is carried out, the periodontal status can return to steadiness [5]. Typically upheld by the consideration of Balaji et al., in teeth with mobility grade 3, most are categorized in a poor prognosis where the tooth will more often be extracted [19].
Based on Table 4, the foremost common alveolar bone height following the temporary periodontal splint was the middle third of the root, with 127 cases (49.2%). The other most reported alveolar bone height was the apical third of the root, which was 103 (39.9%), while the cervical third comprised 28 cases (10.9%). The tooth most involved in the temporary periodontal splint was tooth #31, with bone height up to the apical third (18 cases or 7%). Further, tooth 43 with middle third bone height comprised 16 cases (6.2%). Information from alveolar bone loss is comparable to clinical attachment loss information from Table 6, where the most elevated recurrence happened in tooth 31 with a recurrence of 23 (8.2%) with the category of severe clinical attachment loss. The following most noteworthy recurrence was tooth components 41, 32, and 42. This may be due to the alveolar bone of the front teeth being more vulnerable, making it more susceptible to harm [17]. The thickness of the alveolar bone of the mandibular front teeth was thinner compared to the maxillary anterior bone [20]. Typically, compared to the findings of Thomson et al., mandibular tooth loss was more predominant than maxillary front teeth [21].
Based on Table 5, the most elevated recurrence of horizontal alveolar bone loss was up to 162 (62.8%), and for vertical bone loss, it was 96 (37.2%). Vertical bone loss was related to periodontal malady caused by TFO in these teeth, whereas the loss was ordinarily associated with periodontal illness [22]. This is in agreement with other studies where vertical bone loss was found in 82.7% of teeth with TFO and 17.9% of teeth with ordinary impediment, and a level design was found in 91.4% of ordinary impediment and 8.6% of teeth with TFO [23].
The utilization of a splint makes cleaning more difficult [24]. In this sense, plaque accumulation may contribute to worsening the inflammation. This finding supports that patients who were given proper Dental Health Education (DHE) after splinting had a lower plaque record than people who were not [25, 26].
CONCLUSION
Information dispersion among patients who experienced a temporary periodontal splint were most frequently female (70.2%), young elderly (53.2%), extra-coronal type (55.4%), who underwent an occlusal adjustment (51.8%), had good OHI-S (75%), and had TFO (45.2%). The most utilized periodontal splint was tooth #43 (8.7%) and mandibular front region. The most experimented tooth with a periodontal splint was tooth #31, with a 2-degree mobility of 8%, and the alveolar bone height to the apical third of the root was 7%. These findings suggest that mandibular teeth are likely to have mobility and, therefore, need a temporary periodontal splint. As a consequence, proper oral care should be maintained in order to improve the periodontal condition.
AUTHORS’ CONTRIBUTION
B.S., D.I.H., and A.J. designed the study.
H.R. and F.M.T. reviewed the study.
B.S., D.I.H., and A.J. performed the study.
B.S., D.I.H., and A.J. analyzed the data.
B.S. and D.I.H. wrote the main manuscript.
All authors reviewed the manuscript.
LIST OF ABBREVIATIONS
| BOP | = Bleeding On Probing |
| TFO | = Trauma From Occlusion |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The protocol of this study has been registered and approved by the Ethical Board Committee of the Universitas Indonesia (Number: 58/Ethical Approval/FKGUI/IX/2021).
HUMAN AND ANIMAL RIGHTS
All human procedures were followed in accordance with the guidelines of the Declaration of Helsinki.
CONSENT FOR PUBLICATION
Written informed consent has been taken from the patients /Volunteers/ guardians of the children for this study as stated in the medical record that all data can be used in regard to scientific purposes.


