All published articles of this journal are available on ScienceDirect.
Non-surgery Treatment with MEAW Technique in Skeletal Class III Malocclusion and Facial Asymmetry in Adults: A Case Report
Abstract
Background
Treating skeletal Class III malocclusions characterized by mandibular deviation, facial asymmetry, and other complex orthodontic issues is among the most demanding orthodontic procedures. Orthognathic surgery is not recommended to everyone due to the dangers involved. Hence, it is considered to be very difficult to correct face asymmetry with orthodontics alone, much less without surgery.
Objective
The goals of this case study were to decrease crowding in the upper teeth, manage the vertical dimension, and treat the patient's primary complaints of crossbite in the anterior teeth and facial asymmetry.
Case Presentation
A female patient, aged 21, came in with many concerns, including an incisor crossbite, facial asymmetry, and an insecurity that manifested only when she smiled. An adult patient with a mandibular deviation to the right and an incisor crossbite received orthodontic treatment for these issues. The patient had asymmetric molar extraction in both the lower and upper jaws to retract the lower incisors and correct the midline of the teeth using intermaxillary elastic. Fixed appliances were utilized in conjunction with overbearing lower anterior braces to manage the torque on the lower anterior teeth. As a result, she had a pleasant smile, a harmonious face, and stable dental and skeletal connections. The whole therapeutic period lasted 30 months. As a result, asymmetric molar extraction may be an acceptable option for retracting mandibular incisors in Class III malocclusion with facial asymmetry.
Conclusion
The most important step in treating the severe skeletal Class III malocclusion in this patient without surgery was to retract the lower arch. After using the MEAW approach, Class III elastics, posterior bite turbos, and orthopedic splint treatment, the patient reported a satisfactory achievement.
1. INTRODUCTION
This case discusses the treatment of Skeletal Class III malocclusions, which include facial asymmetry and man- dibular deviation. The treatment options mentioned include both surgery and non-surgical orthodontic approaches. The prevalence of misaligned dentition and facial asymmetry among orthodontic patients has increased in recent years. Diagnosing and treating individuals with Class III malocclusion, facial asymmetry, and mandibular malalignment is often more intricate compared to those without mandibular asymmetry. Ortho- dontists are required to distinguish between asymmetrical issues that arise from dental and skeletal causes. For instance, the assessment of molar compensation in the molar area should be included in the diagnostic. It is crucial to manage a growing Class III malocclusion with mandibular deviation since the malocclusion tends to deteriorate as the child matures. Nevertheless, individuals with skeletal Class III malocclusion often exhibit facial asymmetry or midline deviation, and a few of them ultimately need surgical orthodontic intervention [1]. Facial asymmetry and dental-skeletal abnormalities arise from the complex interaction of several variables that impact the process of development and growth. These discrepancies in size and location may lead to the formation of structures that are found between the skull base and maxilla, the skull base and mandible, or the maxilla and mandible. They can also be found within the rest of the craniofacial mass [2]. The majority of individuals with Class III malocclusions have difficulties with the teeth and alveolar bone, and only a limited percentage of instances may be resolved solely by orthodontic treatment. Individuals suffering from significant skeletal Class III malocclusion discrepancies often have orthognathic surgery, which may include maxillary, mandibular, or both (bimaxillary), in conjunction with orthodontic treatment [3].
The management of dentoskeletal abnormalities involves the use of orthopaedics, orthodontics, ortho- paedic surgery, or a combination of these treatments. Roughly 4% of the population exhibits dentofacial abnormalities necessitating orthodontic surgery for correction. Surgical therapy is mostly recommended for individuals with severe skeletal Class II and III malocclusion, as well as longitudinal bone discrepancies, who have completed their growth period. A significant number of individuals seeking orthodontic-surgical therapy are patients with Skeletal Class III malocclusion. Proffit et al. found that 20% of surgery patients had mandibular excess, 17% had a maxillary recession, and 10% had both conditions simultaneously. Clinical evaluation is more common in patients with skeletal Class III malocclusion compared to those with skeletal Class II malocclusion [4]. Severt and Proffit conducted a study at the University of North Carolina, where they examined a sample of 1460 patients. They found that 34% of these individuals had facial asymmetry. The Menton's deviation was seen in 74% of individuals who were considered to have asymmetry, making it the most prominent characteristic of asymmetry. These results are of great importance to doctors as they highlight the need to identify and prepare for asymmetry before initiating treatment [5].
The majority of individuals with Class III malocclusion exhibit dental and alveolar issues, and only a small number of instances may be resolved solely by orthodontic treatment. Patients who have significant skeletal Class III malocclusion discrepancies typically have orthodontic surgery on the maxilla, mandible, or both, along with orthodontic therapy. The occurrence of mandibular asymmetry is more often observed in individuals with Skeletal Class III malocclusion [6]. Kerr et al. reported that patients with an ANB angle below 4° and mandibular incisors with an inclination below 83° were more likely to require orthodontic-surgical treatment [7]. When dealing with facial asymmetry, the usual strategy is to use orthodontics alone to fix the issue horizontally. However, this method generally fails to provide the desired results, and many patients see a return of the asymmetry [8]. Class III malocclusion, caused by the bone's inclination to misalign the jaw unevenly, is regarded as a very challenging condition to address with orthodontic methods alone, without the need for surgical intervention. This case report presents the orthodontic treatment of a mature patient with skeletal Class III malocclusion, characterized by a rightward mandibular deviation and an incisor crossbite. The lower incisors have been inclined posteriorly to offset the skeletal imbalance. The patient had asymmetrical molar extraction in both the upper and lower jaws to retract the lower incisors and align the midline of the teeth using intermaxillary elastics. Fixed appliances were used in conjunction with forceful lower anterior braces to regulate the torque of the lower incisors. Following a treatment duration of 30 months, we successfully attained a pleasing smile, improved facial aesthetics, and a fully functional bite. Asymmetric molar extraction might be a suitable choice for moving back the lower incisors in cases with Class III malocclusion with midline deviation.
2. CASE REPRESENTATION
2.1. Diagnosis and Etiology
A 21-year-old Vietnamese female patient complained of tension in her front teeth and a lack of confidence when smiling. Her medical history revealed nothing unusual; she had lost the right lower first molar, and her chin was asymmetrically concave and deviated to the left. During the extraoral examination, the profile showed a concave profile, harmoniously thick lips, sharp nasolabial angles, and an almost flat labial fold. The view from the front showed an asymmetrical dolichofacial face; the lower part of the face was increased, and the nose was even but was slightly shifted to the left. Patients with lips that were not aesthetically pleasing had regular lip lengths and shapes. When smiling, the patient had a smile that was not in harmony with the entire length of the front tooth crown, did not reveal the gums, and had an even lip line. She had an average lip length and shape and a normal upper midline (Fig. 1). Intraorally, the patient had good oral hygiene with some racial pigmentation. She had an Angle Class III on both sides and a Class III canine relationship on both sides. Malocclusion was complicated by tilted and protruding lower incisors. She had a moderate density in her lower arch. The arch forms of the upper and lower casts were oval-shaped (Fig. 2).

The facial photographs of pre-treatment, 21 y/o female.

Intraoral photographs of pre-treatment.
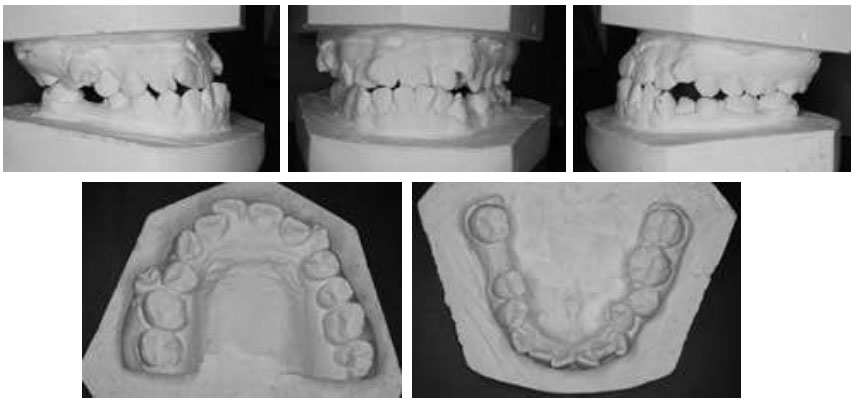
The study models (casts) of pre-treatment.
Additionally, dental casts showed an asymmetric maxillary arch in the transverse and anteroposterior planes due to constriction in the upper right posterior segment compared to the upper left segment buccally positioned crossbite incisors UR1, UR2, UL1, and UL2 (Fig. 3). This caused the upper right segment to be ahead of the upper left segment. Moreover, the mandibular arch had an asymmetric arch form in the anterior segment transversely and anteroposteriorly. The patient had mesiolabial rotation in incisor LR1 LR2, LL1, and LL2. A space analysis using a digital caliper indicated moderate crowding (7 mm) in the lower arch and severe crowding in the upper arch (12 mm) (Fig. 3).
The analysis of lateral cephalometric radiography and its tracing showed that according to Vietnamese norms, the patient had a skeletal Class III relationship (SNA: 86.75°, SNB: 90.16°, ANB: -4.56°) that was confirmed by Wits appraisal: -4.56 mm, mandibular plane angle (Go-Gn to SN): 36.01°, overbite: 0.51 mm, overjet: -1.26 mm, U1 to FH: 117.32°, U1 to NA: 3.22 mm, interincisal angle: 130.39°, L1 to A-Pog: 6.03 mm, L1 to mandibular plane angle: 84.11°, upper molar to PtV: 17.71 mm. Further- more, she had a normal nasolabial angle and upper retrusion and a normal lower lip (nasolabial angle: 86.48°, lower lip to E-plane: 3.37 mm, upper lip to E-plane: -0.17 mm) (Table 1).
The panoramic radiograph showed that condyles and ramus were relatively symmetrical. The tooth morphology, bone level, temporomandibular joint, and maxillary sinus were normal, and no bony pathologies were observed, with both upper third molars erupting (Fig. 4).
2.2. Treatment Objectives
The treatment goals resolved the patient's primary concern of crossbite in the anterior teeth and over- crowding of teeth to enhance facial appearance and symmetry, achieving a harmonious facial profile, proper lip function, and secure lip closure. In addition, it was crucial to manage the patient's vertical dimension, address the upper dental crowding, preserve a Class I canine relationship on both sides, achieve an optimal horizontal overlap and vertical overlap of the front teeth, and repair the misalignment of the dental midline, asymmetry in the arch, and a disparity in tooth size. Our goal was to establish a functional occlusion where the upper and lower teeth fit together properly, using a canine-guided mutually protected occlusal scheme without any interferences and creating a distinct grin arc.
2.3. Treatment Plan
The plan for this camouflage treatment was to resolve the Class III relationship by retracting the lower arch and correcting the anterior crossbite. We used a positioner to lift the joint to erase muscle memory and bring the lower jaw to the midline position. We used the MEAW technique, and posterior bite turbos were planned to assist with the correction. Early light short triangle, Class III, and box elastics were utilized to rectify the molar relationships.
| Measurements | Norm (SD) | Initial | Post-treatment |
|---|---|---|---|
| SNA | 81.08 (3.7) | 86.75 | 87.18 |
| SNB | 79.17 (3.8) | 90.19 | 85.68 |
| ANB | 2.46 (1.8) | -4.56 | 1.50 |
| Wits appraisal | -0.33 (2.7) | -5.56 | 0.29 |
| Facial axis | 88.1 (2) | 86.94 | 88.05 |
| Y-axis | 59 (6) | 59.21 | 59.51 |
| Lower anterior face height | 65 (5) | 61.96 | 62.57 |
| Mandibular plane angle (Go-Gn to SN) | 32 (4) | 36.01 | 35.24 |
| Facial angle | 87.8 (3.5) | 92.17 | 92.08 |
| A-B to mandibular plane | 69.3 (2.5) | 59.74 | 57.85 |
| ANS-Xi-Pm | 47 (4) | 50.77 | 52.33 |
| ODI | 72.15 (5.5) | 58.46 | 57.5 |
| Combination factor | 157.9 (6.5) | 149.27 | 148.58 |
| APDI | 85.74 (4) | 90.81 | 91.08 |
| Overbite | 2 (2) | 0.51 | 0.96 |
| Overjet | 2 (2) | -1.26 | 2.1 |
| U1 to FH | 113.8 (6.4) | 117.32 | 121.12 |
| U1 to NA(mm) | 4 (3) | 3.22 | 4.96 |
| Interincisal angle | 128 (5.3) | 130.39 | 141.8 |
| L1 to A-Pog(mm) | 1 (2) | 6.03 | 3.75 |
| L1 to mandibular plane angle | 92 (5) | 84.11 | 70.36 |
| Upper molar to PtV | 21.1 (3) | 17.71 | 15.51 |
| Nasolabial angle | 95 (5) | 86.48 | 63.5 |
| Lower lip to E-plane | 0 (2) | 3.37 | 0.74 |
| Upper lip to E-plane | 0 (2) | -0.17 | 0.9 |

The lateral cephalogram, panoramic radiograph of pre-treatment.
2.4. Treatment Alternatives
2.4.1. Option 1
Orthognathic surgery is often indicated for severe skeletal Class III malocclusions. In this case, it was the option that could achieve the best treatment outcome; however, the cost and morbidity of orthognathic surgery caused the patient great concern.
2.4.2. Option 2
This involved extracting the third molar on the left lower jaw and the third molar on the upper left on both sides, retracting, and using the TSAD for anchorage. This option has the advantage of preserving stronger teeth because the 2nd molars are usually stronger than the 3rd molars. However, a downside to this option is that it increases the difficulty of retraction: the mandibular arch and midline are misaligned even though the patient has lost the lower right first molar, and it is difficult to align the midline.
2.4.3. Option 3
This involved extracting the upper second premolars on both sides and the lower first premolars on the left, controlling midline alignment, posterior teeth bite elevation, and anterior tooth cross-alignment, and using intermaxillary elastic with MEAW techniques.
After a thorough discussion of the advantages and disadvantages of each approach, the patient chose option 3 as the most desirable camouflage treatment to avoid surgery. The patient provided informed consent for the treatment, knowing that this approach was challenging and that the outcome would be compromised. It was also suggested that the upper 3rd molars should be extracted because they would not be within the occlusion after treatment.
2.5. Treatment Progress
We used an orthopedic splint treatment to erase muscle memory and bring the lower jaw to the midline position within 5 months (Fig. 5). After 5 months, we extracted the upper second premolars on both sides and the lower first premolars on the left. A 0.022-in slot Victory Series (MBT -0.022 slot), 3M Unitek® US fixed appliance bracket was selected with all specified archwires and orthodontic auxiliaries. A 0.022-in slot Victory Series was bonded on the lower teeth with a 0.014-in CuNiTi archwire engaged. Standard torque was selected for the brackets. In the 12th month, the leveling and alignment were completed. The upper archwires were changed to 0.016 × 0.025-in SS (Fig. 6). In the 18th month, we used the MEAW technique to correct the midline and Class I canine. Early light short triangle elastics (Quail, 3/16-in, 2 oz; Ormco) were used for 3 months to correct the anterior crossbite. Simultaneously, box elastics (Fox, 1/4-in, 3.5-oz; Ormco) from both sides, U4,6 to L4,6, were used to correct (Fig. 7). In the 25th month, both archwires were changed to 0.014 × 0.025-in NiTi. Class III elastics (Quail, 3/16-in, 2 oz; Ormco) and light short triangle elastics (Quail, 3/16-in, 2 oz; Ormco) were used bilaterally from U6s to L3s for 5 months to achieve a Class I molar relationship. Simultaneously, box elastics (Fox, 1/4-in, 3.5-oz; Ormco) from UR4, UR6 to LR4, LR6 were used for correction. After 30 months of active treatment, all fixed appliances were removed (Fig. 8), and fixed retainers were bonded on the lingual surfaces from canine to canine in the mandibular arch, with restoration of the second lower right premolar and second lower right molar. The upper retainers were delivered using the Hawley appliance.
3. RESULTS ACHIEVED
The facial aesthetics and anterior crossbite were significantly improved after 30 months of active treatment (Fig. 9). The molar relationships were corrected to Class I on the left and Class II on the right (Fig. 10). The post-treatment panoramic radiograph documented acceptable root parallelism (Fig. 11). The superimposed cephalo- metric tracing showed proclined maxillary incisors resulting from anterior crossbite correction (Fig. 12). The axial inclination of the upper incisors (U1-FH) increased by 4° after treatment (117.32° to 121.12°), and the axial inclination of the lower incisors (L1-MP) fell inside (84.11° to 70.36; Table 1). The lower lip was retruded following the retraction of the anterior segments. The mandibular plane angle (SN-MP) was well-maintained (Table 1). The patient was pleased with the final results without orthognathic surgery.

Orthopedic splint.

At 12 months of orthodontics treatment.

At the 18-month treatment, we used light short triangle elastics (Quail, 3/16-in, 2 oz; Ormco) and box elastics (Fox, 1/4-in, 3.5-oz; Ormco) with the MEAW technique in the mandibular.

The facial and intraoral photographs of post-treatment.

The facial photographs of post-treatment.
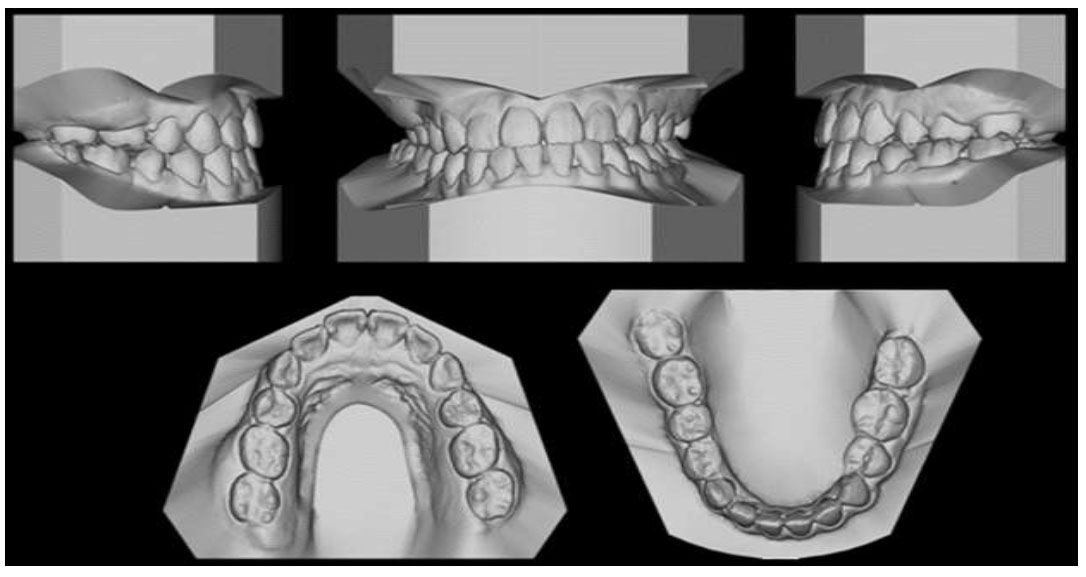
The study models (scan) of post-treatment.

The lateral cephalogram, panoramic radiograph of post-treatment.
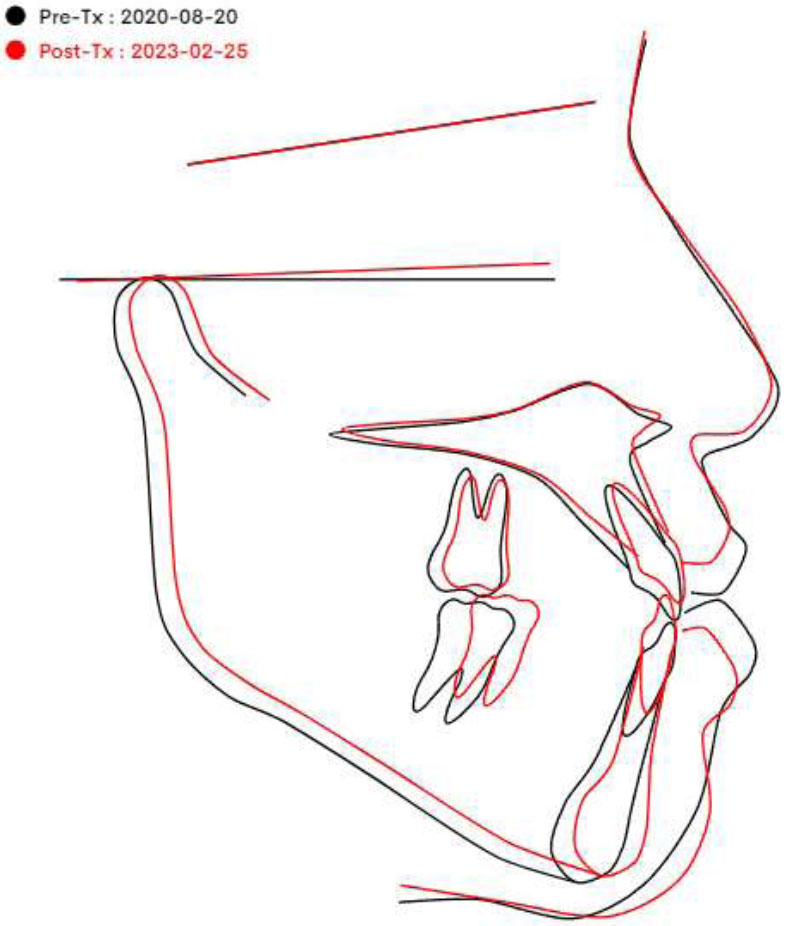
The superimposed cephalometric tracings, with the black representing the pre-treatment and the red representing the post-treatment, demonstrate the pre-treatment Class I molar relationship. The proclined maxillary incisors resulting from anterior crossbite correction were observed and deemed satisfactory.
4. DISCUSSION
The alveolar dehiscence on L3 was caused by unmitigated forces and inaccurate L3s center of resistance estimates. The torquing auxiliary could not be used due to inadequate leveling and rotation. Moreover, to alleviate periodontal problems, active, unmitigated orthodontic pressures should be removed from the tooth in consideration [9]. The most effective approach is to eliminate active forces from L3, allowing the root to move into the alveolar housing. Excessive tooth movement towards the labial cortical plate can cause gingiva thinning and partial visibility of the root contour, leading to the “washboard effect” and potentially causing bone loss or resorption of the root when teeth touch the cortical bone [10]. When teeth were moved forward, Nasib Balut (2019) and Adith Venugopal (2020) found that the buccal alveolar plate had dehiscence or fenestrations. When the teeth were moved back into their original positions within the alveolar housing, the defects healed and were repaired [11, 12]. The most effective approach is to eliminate active forces from L3, allowing the root to move into the alveolar housing. Excessive tooth movement towards the labial cortical plate can cause gingiva thinning and partial visibility of the root contour, leading to the “washboard effect” and potentially causing bone loss or resorption of the root when teeth touch the cortical bone.
In orthopedic splint treatment, a lower splint is used to reposition the mandible in a forward position while allowing normalization of the condyle, disc, and fossa relationships. The orthopedic splint treatment is performed on the lower arch with a heavy lingual bar connecting the two acrylic halves. First, treatment with an orthopedic functional appliance deploying a distraction brace can reduce mandibular asymmetry between the affected and unaffected sides. Second, treatment with a distraction splint causes mandibular growth rates on the affected and unaffected sides to become equivalent in most patients. Distraction splints optimize dentoalveolar development on the affected side to avoid occlusal collapse. Avoiding such collapse is important for the coordinated condylar and dentoalveolar growth required to achieve optimal vertical mandibular growth. It is unlikely that chiropractic treatments cause the condyle to grow more than is indicated by the individual’s normal genetic predisposition; however, here we present evidence supporting beneficial bone improvement in facial asymmetry in JIA patients treated with distraction bracing for unilateral TMJ arthritis. The clinical value of early distraction splinting also lies in its ability to produce equivalent bilateral growth so that asymmetry is minimized when the mandibular growth phase ends, even in patients with unilateral arthritis [13]. Most authors concluded that skeletal changes combined with improvements in fusion after treatment with orthodontic orthodontics may result in better dentofacial aesthetics. The function of this tool is to reduce the severity of surface changes, improving the development of the mandible and condyle [14]. Several clinical and experimental studies suggested a relationship between masticatory muscle function and craniofacial development [15, 16]. Therefore, experimental intervention in jaw and facial muscle development has been shown to entail major changes in mandibular shape [16, 17]. In the case of asymmetry, this can be the front and back, with the components being horizontal and vertical. The orthodontist must determine which components contribute to the problem asymmetry to plan appropriate treatment methods [18].
Class III elastic traction is an intermaxillary traction force from the lower canine region to the molar region of the upper jaw. This moves the upper teeth forward and the lower teeth back. Class III elastic traction is used in several cases, such as camouflage treatment in Type III patients with failure to thrive, the orthognathic extension of the maxilla in skeletal Class III patients with maxillary deficiency, and anchorage reinforcement [19]. This asymmetry case report has three components: the front and back components are different molars and canines, and the third component is the relationship between right and left. The horizontal component represents the left posterior crossbite, and the vertical component is the occlusal tilt. Bite misalignment is very difficult to fix with non-surgical treatment, especially when related to the lateral deviation of the mandible; thus, we try to treat the vertical asymmetry component. However, in this case, this is only effectively resolved with bone surgery because we can only care for teeth. Anterior-posterior asymmetrical components are treated by extracting asymmetrical lower molars. In this case, we extracted the first premolar on the left of the lower jaw and used symmetrical Class III intermaxillary elastics to correct the Class III molar relationship on the right side and move the teeth and midline mandible to the right. Although the left side initially had Class III canines and molars, the patient had the lower right second molar extracted to retract the lower incisors and use an anchor from the second molar on the right sides of the lower jaw to move the midline of the upper teeth to the right side with a Class III intermaxillary elastic. The horizontal asymmetry component was corrected with diagonal and anterior diagonal elastic. It is necessary to be especially careful when using this if the intermaxillary elastic between the jaws is asymmetrical to avoid creating or aggravating malocclusion [20]. Additionally, intermaxillary elastics require excellent patient cooperation to be effective [21].
This case report emphasizes the importance of wearing intermaxillary elastics in every appointment to achieve good results. Posterior bite turbos, which are designed to help correct bite issues, can be positioned in the posterior segments. Nevertheless, certain limitations should be considered regarding this treatment option. The protocol for bite turbos was necessary to correct the anterior crossbite [22]. A posterior bite raiser made the mandible rotate anticlockwise due to intruding posterior teeth and correction of an anterior open bite, decreasing the lower anterior facial height. A posterior bite plane that extends posteriorly from the first premolar to disocclude anterior teeth is beneficial for managing an anterior crossbite. Additionally, due to the vertical intrusive forces on the posterior segments, these have also been used to manage cases of open bites [23]. Biomechanics assists the clinician in visualizing the expected direction of inclination and planning the appropriate length and thickness of the occlusal plane. Bite advancement devices have a different mechanism when used in conjunction with fixed orthodontic treatment, which has been briefly explained. The occlusal plane influences the molar tilt; in the case of a posterior bite, the block is placed in the patient’s mouth. When a force is applied to the molar’s distal apex, it is far from its center of resistance. Therefore, a distal tilt of this molar will occur. If molars are already leaning toward the near side, the force will be extremely large and far from its center of resistance; therefore, no opportunities will be created for molar repair. Thus, the bite turbo is extended further to create penetrating forces that are more distant from the center of resistance, leading to erect mesial molars. However, with Class III, this can be placed on the lower incisors to either open the bite or treat the negative overjet, as the functional bite turbos can procline the upper incisors [24].
The MEAW technique possesses several mechanical properties that facilitate the correction of various types of malocclusions. It provides control over each tooth by applying gentle and even pressure. Difficult cases such as open bites or skeletal Class III malocclusions with low to moderate severity can be effectively treated with this method [25]. Once the upper dental arch was symmetrical, we used a MEAW on the lower arch to adjust the bite relationship. An important goal to achieve when treating Class III is to reconstruct the occlusal plane because Class III malocclusion requires a steeper occlusal plane for the mandible to adapt posteriorly. The posterior curvature of the MEAW aligns the premolars and molars to a vertical position and penetrates the molars. The precise treatment mechanism used is activating a gradual 3° to 5° retroflex from the premolars to the molar area with short (3/16-inch, 6 oz) Class III elastics on the teeth. The MEAW technique has been proven effective in treating Class III malocclusion. The MEAW is a valuable alternative in treating Class III malocclusion when the patient refuses surgery, and the disharmony of the bony structure is not severe. A MEAW used correctly can accurately reconstruct the occlusal plane, enabling a precise and stable bite and improving facial shape and balance [26]. The MEAW technique appears to have significant therapeutic advantages and functions as a compensatory treatment modality in certain types of malocclusion [27].
CONCLUSION
In summary, the successful treatment for challenging skeletal malocclusion Class III facial asymmetry and mandibular deviation was completed in only 30 months without orthognathic surgery. For the present patient, retracting the lower arch was the key to managing the severe skeletal Class III malocclusion without surgery. Moreover, by using orthopedic splint treatment and posterior bite turbos combined with Class III elastics and the MEAW technique, the patient was provided with an acceptable result. However, long-term follow-up was necessary to ensure the ongoing stability and maintenance of the occlusion. The use of a Hawley retainer coupled with careful monitoring every 12 months enabled a successful outcome in this complex case.
AUTHORS' CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| MEAW | = Multiloop Edgewise Archwire |
| Upper Right | = UR |
| UL | = Upper Left |
| LR | = Lower Right |
| LL | = Lower Left |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethics committee approval was received for this studyfrom the Ethics Committee in Biological Research of Can Tho University of Medicine and Pharmacy, CanTho City, Vietnam.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data that supports the findings of the article will be available from the corresponding author [L.N.L] upon reasonable request.


