All published articles of this journal are available on ScienceDirect.
Characteristics of Maxillofacial Trauma in Motorcycle Accidents at a Regional General Hospital in Indonesia: A Five-year Retrospective Study using the Facial Injury Severity Scale (FISS) and Maxillofacial Injury Severity Score (MFISS)
Abstract
Purpose
This study aimed to observe the correlations between factors that influence motorcycle accidents (such as accident time and helmet use) and the Facial Injury Severity Scale (FISS) and Maxillofacial Injury Severity Score (MFISS) scores in patients with maxillofacial trauma.
Methods
Data from maxillofacial trauma patients at the Tangerang Regency General Hospital in Banten, Indonesia, were retrospectively reviewed from June 2017 and May 2022 using the FISS and MFISS scores.
Results
A total of 257 patients were included in the study. Significant differences (p < 0.05) in FISS and MFISS based on accident time and helmet use were observed. Multivariate analysis revealed significant correlations (p < 0.05) between the factors and the maxillofacial trauma severity based on the FISS and MFISS.
Conclusion
The severity of maxillofacial trauma based on the MFISS was influenced by the accident time and helmet use. Similarly, the severity of maxillofacial trauma based on the FISS was directly related to the accident time; however, it was inversely related to the use of a helmet.
1. INTRODUCTION
At least 1.35 million people die in traffic accidents every year, with motorcyclists accounting for the majority (28%), followed by pedestrians (23%) [1, 2]. In addition to material loss, traffic accidents can lead to motor and psychological damage, resulting in physical disability [3-5]. Motorcyclists are eight times more likely to be injured than car passengers. Moreover, motorcyclists are 37 times more likely to die than car passengers in an accident per vehicle mile travelled [3].
In 2014, 81% of the 113 million vehicles registered in Indonesia were motorcycles [6-8]. The high rate of motorcycle ownership has resulted in increased motorcycle accidents. According to a recent study, 73% of deaths and significant injuries due to traffic accidents occur among motorcyclists in Indonesia [6]. Champahom et al. reported that the severity of motorcycle accidents was caused by several factors, such as age, use of helmets, lighting conditions, and the condition of the path used by the vehicle [9]. Motorcycle accidents in Indonesia are associated with a higher trauma severity than other vehicle accidents, resulting in head, thoracic, pelvic, abdominal, and maxillofacial trauma [10-12].
Physical injury to the facial region is referred to as maxillofacial trauma; it is frequently associated with a high mortality rate. Maxillofacial trauma involves the soft and hard tissues in the facial region and presents various manifestations, from soft tissue lacerations to maxillofacial fractures [13-15]. Motorcycle accidents are one of the leading causes of maxillofacial fractures in several developing countries, including Indonesia [13]. The severity of maxillofacial fractures caused by a motorcycle accident can vary and is related to various factors.
Severity indices are commonly used to assess the extent of the trauma and injury. The index developed to assess the severity of trauma can be based on physiological changes or damage to the anatomical structures [16]. The trauma severity index aims to provide an overview of the treatment prognosis and the patient's condition while being treated. This scoring system is essential for epidemiological trauma studies [17]. The Facial Injury Severity Scale (FISS) and Maxillofacial Injury Severity Score (MFISS) are frequently used to assess the severity of maxillofacial trauma. The FISS is an injury scale specific to facial trauma; it acts as a practical tool for communication between the doctor and the health professional during the management of facial trauma [18]. On the other hand, the MFISS can indicate the severity of the maxillofacial injury,and it can be used to predict the treatment outcomes and estimate the consumption of medical resources [19].
The potential use of the FISS and MFISS to determine the prognosis of patients with maxillofacial trauma has shown promising results. However, related factors, such as the accident time and helmet use, which can affect the severity of maxillofacial trauma, have not been widely studied based on these indices. This study aimed to observe the correlations between factors influencing motorcycle accidents (accident time and helmet use) and the FISS and MFISS in patients with maxillofacial trauma. The relationships between FISS and MFISS and the aforementioned factors might prove useful in epidemiological studies, wherein they can be used as references for safety recommendations and to prevent traffic accidents.
2. METHODS
2.1. Study Design and Population
This 5-year retrospective study (from June 2017 to May 2022) comprised patients who encountered motorcycle accidents and were treated at the Oral and Maxillofacial Surgery Unit of the Tangerang Regency General Hospital in Banten, Indonesia. The Tangerang Regency General Hospital is a referral hospital for the entire Tangerang Regency area in Banten. Based on data from the Indonesian Central Statistics Agency in 2021, Tangerang Regency has a population of 3,293,533 people, and the number of motorcycles used by the residents at that time was 1,203,050; most of the motorcycles were below 250 ccs [20]. All data on maxillofacial trauma patients admitted to the Tangerang Regency Hospital were collected retrospectively and recorded. The accident time was categorized into night (6 p.m. to 6 a.m.) and day (6 a.m. to 6 p.m.), and helmet use was categorized as those wearing and not wearing a helmet.
2.2. Trauma Scoring
The severity of maxillofacial trauma was assessed retrospectively using the FISS and MFISS. The FISS, introduced by Bagheri et al. in 2006, sums the scores of fractures at specific anatomical locations. The points differ depending on the values assigned to each anatomic location; the higher the FISS score, the greater the severity of the maxillofacial trauma cases [18]. The FISS scores were classified into slight (0-1), moderate (0-5), and severe (≥ 6) [21]. The MFISS, introduced by Zhang et al. also in 2006, limits the evaluation of injuries to the maxillofacial region, regardless of other injuries the patient may have on the body. This scoring system uses the Abbreviated Injury Scale (AIS) and aims to select the three highest AIS-90 maxillofacial injury severity scores. The three scores are then combined with the injury severity scores for three maxillofacial functional parameters: malocclusion (MO), limited mouth opening, and facial deformity [19].
3. RESULTS
A total of 257 patients were examined in this study. The characteristics of the patients are shown in Table 1. The mean age of the patients was 27.56 ± 12.56 years. The proportion of men was higher than that of women (81.3% vs. 18.7%, respectively). Most patients were riders, with a ratio of 93.0% to 7.0% for riders and passengers, respectively.
The distribution of maxillofacial trauma among the patients is shown in Table 1. Trauma to the upper face or frontal bone was least frequently encountered (n = 13), whereas midface trauma was the most frequently recorded (n = 211); maxillary dentoalveolar trauma accounted for the majority of (63.03%) of all midface trauma cases. Furthermore, trauma to the mandible occurred in 166 cases, with symphyseal/parasymphyseal fractures accounting for most cases (48.19%; 80/166).
A total of 122 patients experienced a combination of fractures, with the midface and mandible combinations being the most common (95.08%; 116/122). Two patients (1.64%) had combined fractures in the upper face and midface, and none had a combined fracture in the upper face and mandible (Fig. 1). Four patients had a combination of fractures in all three regions, the upper face, midface, and mandible (Table 1). The MFISS severity index averaged 19.16 ± 12.58, with a min-max score of 1-49. The average FISS score was 3.45 ± 2.93, with a min-max score of 1-18.
3.1. The MFISS
The distribution of MFISS based on the characteristics of the patients is illustrated in Table 2. Most patients (n = 89; 34.63%) belonged to the minor category (low score), followed by 64 (24.90%) in the moderate group, 62 (24.12%) in the serious group, and 42 (16.34%) in the severe group. The mean age of the patients in the four groups was similar, ranging from 24.00 to 29.63 years in each group. The proportion of patients in the different MFISS severity categories based on gender and factors related to the accident is shown in Table 2.
Bivariate analysis using logistic regression modeling odds ratio (OR) was performed for each factor (Table 3). The MFISS in accidents that occurred at night (6 p.m.-6 a.m.) was likely to be higher (more severe) than those in accidents that occurred during the day (6 a.m.-6 p.m.) in the moderate (OR = 3.04; 95% confidence interval [CI], 1.51-6.13), serious (OR = 4.472; 95% CI, 2.21-9.07), and severe (OR = 25.53; 95% CI, 8.86-73.56) groups. Furthermore, patients who did not wear helmets had a greater chance of presenting with a higher MFISS than those who wore helmets (Table 3).
| Characteristics | Frequency | Percentage |
|---|---|---|
| Age (Mean, in Years) | 27,56 ± 12,56 | - |
| Sex | - | - |
| Male | 209 | 81,3% |
| Female | 48 | 18,7% |
| Accident time | - | - |
| 6 pm - 6 am | 122 | 47,5% |
| 6 am - 6 pm | 135 | 52,5% |
|
Helmet use Wearing helmet |
117 | 45,5% |
| Not wearing helmet | 140 | 54,5% |
|
Rider/passenger Passenger |
18 | 7,0% |
| Rider | 239 | 93,0% |
| Year | - | - |
| 2017 (June-Dec) | 40 | 15,6% |
| 2018 | 77 | 30,0% |
| 2019 | 56 | 21,8% |
| 2020 | 36 | 14,0% |
| 2021 | 36 | 11,3% |
| 2022 (Jan-May) | 19 | 7,4% |
| Total | 257 | 100% |
|
Type of Trauma Upper face trauma |
13 | - |
| Frontal | 13 | 100% |
| Midface trauma | 211 | - |
| Dentoalveolar | 133 | 63,03% |
| Le Fort 1 | 32 | 15,17% |
| Le Fort 2 | 24 | 11,37% |
| Le Fort 3 | 0 | 0 |
| NOE | 3 | 1,42% |
| Nasal | 35 | 16,59% |
| Orbit | 58 | 27,49% |
| Zygoma | 91 | 43,13% |
| Mandibular trauma | 166 | - |
| Dentoalveolar | 72 | 43,37% |
| Angle | 18 | 10,84% |
| Body | 17 | 10,24% |
| Ramus | 2 | 1,20% |
| Condyle | 50 | 30,12% |
| Symphysis /Parasymphysis | 80 | 48,19% |
| Combination of fracture regions | 122 | - |
| Upper face + Midface | 2 | 1,64% |
| Upper face + Mandible | 0 | 0 |
| Midface + Mandible | 116 | 95,08% |
| Upper face + Midface + Mandible | 4 | 3,28% |
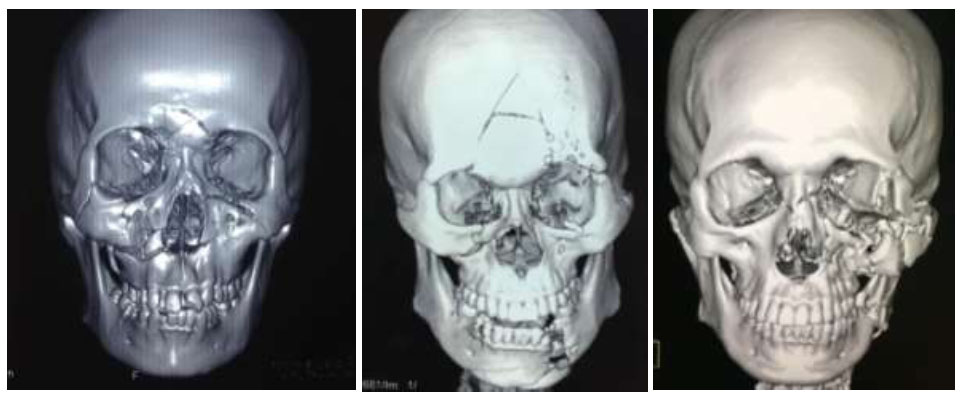
Maxillofacial 3D CT scan reconstruction in some patients: (A) Le Fort II fracture involving the frontal bone; (B) Left parasymphyseal fracture, right infraorbital rim fracture, and frontal bone fracture; (C) Left angle fracture and left zygomaticomaxillary complex fracture.
Multivariate analysis with logistic regression modeling OR was performed for the factors related to the accident (Table 4). It was found that those who met with accidents at night (6 p.m. - 6 a.m.) had a greater likelihood of presenting with a higher MFISS than those who met with accidents during the day (6 a.m. - 6 p.m.). This condition applied to the moderate (adjusted OR = 2.61; 95% CI, 1.21-5.60), serious (adjusted OR = 2.65; 95% CI, 1.13-6.20), and severe (adjusted OR = 24,41; 95% CI, 4.29-138.80) groups. Moreover, patients who did not use helmets had a greater chance of presenting with a more severe MFISS than those who wore helmets (Table 4).
3.2. The FISS Severity Factor Analysis
The distribution of the patients according to the FISS severity and based on the characteristics is documented in Table 5. Most patients were classified as having a moderate FISS score (n = 155; 60.32%); the remaining 24.12% and 15.56% belonged to the slight and severe groups, respectively. The mean ages in the three groups were similar (24.98-28.40 years). The distribution of the patients in the FISS groups based on gender and the factors involved in accidents is shown in Table 5.
Bivariate analysis with logistic regression modeling OR was performed, using the factors related to the accident and the FISS scores. Accidents at night (6 p.m.–6 a.m.) presented with a greater likelihood of having a high FISS score compared to those that occurred during the day (6 a.m.-6 p.m.) in the moderate (OR = 2.24; 95% CI, 1.18-4.25) and severe (OR = 15.00; 95% CI, 5.35-42.09) groups (Table 6). Furthermore, based on helmet use, patients who did not wear helmets had a greater chance of getting a more severe FISS score than those who wore helmets.
| Characteristics |
Minor (1-10) |
Moderate (11-20) |
Serious (21-30) |
Severe (≥31) |
|---|---|---|---|---|
| Total | 89 (34,63%) | 64 (24,90%) | 62 (24,12%) | 42 (16,34%) |
| Age (Mean, in years) | 27,58 ± 13,12 | 27,88 ± 13,18 | 29,63 ± 12,24 | 24,00 ± 6,55 |
|
Sex Male |
63 (70,8%) | 51 (79,7%) | 57 (91,9%) | 38 (90,5%) |
| Female | 26 (29,2%) | 13 (24,4%) | 5 (8,1%) | 4 (9,5%) |
| Accident time | - | - | - | - |
| 6 a.m.-6 p.m. | 69 (46,8%) | 34 (33,6%) | 27 (13,6%) | 5 (3,7%) |
| 6 p.m.-6 a.m. | 20 (16,4%) | 30 (24,6%) | 35 (28,7%) | 37 (30,3%) |
| Helmet use | - | - | - | - |
| Wearing helmet | 59 (42,1%) | 40 (28,6%) | 29 (20,7%) | 12 (8,6%) |
| Not wearing helmet | 30 (25,6%) | 24 (20,5%) | 33 (28,2%) | 30 (25,6%) |
| Characteristics | Minor-moderate | Minor-serious | Minor-Severe |
|---|---|---|---|
| - | OR (95% CI) | OR (95% CI) | OR (95% CI) |
|
Bivariate Analysis Accident time |
- | - | - |
| 6 a.m. - 6 p.m. | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| 6 p.m. - 6 a.m. | 3,04 (1,51-6,13) | 4,472 (2,21-9,07) | 25,53 (8,86-73,56) |
| Helmet use | - | - | - |
| Wearing helmet | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Not wearing helmet | 1,18 (0,60-2,31) | 2,24 (1,15-4,35) | 4,83 (2,17-10,77) |
| Characteristics | Minor-moderate | Minor-serious | Minor-severe |
|---|---|---|---|
| - | Coefficient Adjusted | Coefficient Adjusted | Coefficient Adjusted |
| - | B OR (95% | B OR (95% | B OR (95% |
| - | CI) | CI) | CI) |
| Accident time | - | - | - |
| Morning to evening | 0,96 2,61 | 0,97 2,65 | 3,20 24,41 |
| (6 a.m. – 6 p.m.) / | (1,21-5,60) | (1,13-6,20) | (4,29-138,80) |
| Night (6 p.m. – 6 a.m.) |
- | - | - |
| Helmet use | - | - | - |
| Not wearing | 0,044 1,05 | 0,91 2,48 | 1,72 5,57 |
| helmet/wearing helmet |
(0,49-2,24) | (1.05-5.81) | (1,30-23,91) |
| Characteristics | Slight (0-1) | Moderate (2-5) | Severe (≥ 6) |
|---|---|---|---|
| Total | 62 (24,12%) | 155 (60,32%) | 40 (15,56%) |
| Age (Mean, in years) | 28,40 ± 14,18 | 27,90 ± 12,30 | 24,98± 7,03 |
|
Sex Male |
42 (20,1%) | 130 (62.2%) | 37 (17,7%) |
| Female | 20 (41,7%) | 25 (52,1%) | 3 (7,5%) |
| Accident time | - | - | - |
| 6 a.m. – 6 p.m. | 45 (33,3%) | 84 (62,2%) | 6 (4,4%) |
| 6 p.m. – 6 a.m. | 17 (13,9%) | 71 (58,2%) | 19 (27,9%) |
|
Helmet use Wearing helmet |
37 (26,4%) | 89 (63,6%) | 14 (10,0%) |
| Not wearing helmet | 25 (21,4%) | 66 (56,4%) | 26 (22,2%) |
Table 6.
| Characteristics | Slight-moderate | Slight-severe |
|---|---|---|
| - | OR (95% CI) | OR (95% CI) |
| Accident time | - | - |
| 6 a.m.-6 p.m. | 1 (Ref) | 1 (Ref) |
| 6 p.m.-6 a.m. | 2,24 (1,18-4,25) | 15,00 (5,35-42,09) |
|
Helmet use Wearing helmet |
1 (Ref) | 1 (Ref) |
| Not wearing helmet | 1,10 (0,60-2,00) | 2,75 (1,21-6,27) |
| Characteristics | Slight-moderate | Slight-severe | ||
|---|---|---|---|---|
| - | Coefficient B | Adjusted OR (95% CI) |
Coefficient B | Adjusted OR (95% CI) |
| Accident time | - | - | - | - |
| Morning to evening (6 am-6 pm) |
0,57 | 1,77 (0,69-4,51) | 3,15 | 23,44 (2,42-227,37) |
| Night (6 pm-6 am) | - | - | - | - |
| Helmet use | - | - | - | - |
| Wearing a helmet / Not wearing a helmet | -0.30 | 0,74 (0,30-1,85) | -0.08 | 0,93 (0,18-4,90) |
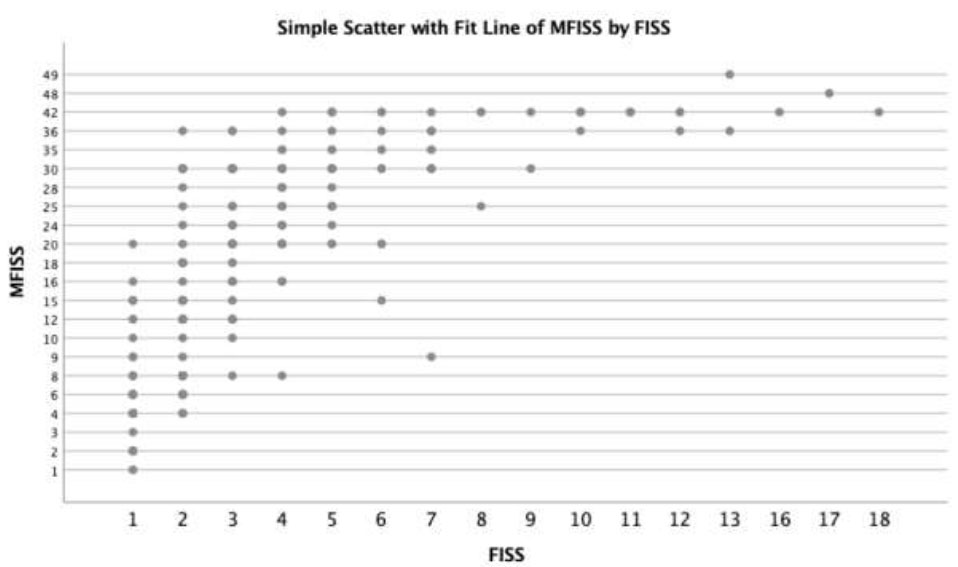
Correlations between the FISS and MFISS scores were registered among the study subjects.
Multivariate analysis with logistic regression modeling OR was performed for each factor with the FISS score (Table 7). Accidents at night (6 p.m.-6 a.m.) generally presented with a greater likelihood of having a higher FISS score than accidents that occurred during the day (6 a.m.-6 p.m.). This condition applied to the moderate (adjusted OR = 1.77; 95% CI, 0.69-4.51) and severe (adjusted OR = 23.44; 95% CI, 2.42-227.37) groups. Meanwhile, patients who did not wear helmets had a lower chance of having a high FISS score than those who wore helmets. Pearson’s correlation analysis between the FISS and MFISS results showed a significant positive relationship (r = 0.761; p < 0.01; Fig. 2).
4. DISCUSSION
Motorcycle accidents are one of the leading causes of maxillofacial trauma, particularly in Indonesia. This study examined correlations between factors influencing motorcycle accidents (accident time and helmet use) and the FISS and MFISS scores in maxillofacial trauma patients at the Tangerang Regency General Hospital. The high number of cases over a 5-year period indicates the importance of assessing the severity of maxillofacial trauma. The results revealed significant differences in the proportions of MFISS and FISS based on helmet use. In the MFISS score analysis, patients who did not wear a helmet had a 4.83 times greater chance of getting a severe score than those who wore a helmet. This result follows studies that reveal that using helmets as personal protective equipment (PPE) can significantly protect craniofacial structures. The absence of a helmet can result in more severe maxillofacial trauma, leading to greater surgical complexity and more extended hospital stays [22].
Several studies have reported the effects of helmet use on the characteristics of maxillofacial trauma. In the study by Moshy et al., 42.3% of mandibular fracture patients wore helmets during accidents, yet, no significant difference in the incidence of mandibular fractures was observed between those who wore and those who did not wear helmets [23]. A meta-analysis by Cavalcante et al. found an increased risk of upper-face and mid-face fractures in patients without a helmet compared with a half-face helmet [24]. Nonetheless, no significant difference in mandible fractures was observed in their study. Our study shows differences in trauma severity based on helmet use on the MFISS and FISS scores. The MFISS score directly correlates with helmet use, while the FISS score shows an inverse relationship.
The inverse relationship between the FISS score and helmet use is related to the number of helmet users (140 patients or 54.5%), and all of them use half-face helmets, except for only one person who uses a full-face helmet. Meanwhile, 117 motorcyclists (45.5%) did not use helmets. In a previous study, Kurniawan et al. reported a difference in the incidence of maxillofacial trauma based on the type of helmet used; 86.33% of patients wore a half-face helmet, while the remaining 13.67% wore a full-face helmet [25]. Furthermore, Ruslin et al. reported that a half-face helmet would not provide maximum protection to the head and face area [26]. In another study, Cini et al. demonstrated that half-face helmet users were twice as likely to require surgery as full-face helmet users [27]. These studies showed that half-face helmets provide less protection against maxillofacial trauma, so the proportion of maxillofacial trauma in the recent study was similar between patients who wear helmets and those who do not. This condition could be related to the multivariate analysis of the FISS score, which showed an inverse relationship.
A significant difference in the average proportions of the MFISS and FISS based on accident time was observed in the current study. Patients who met with an accident at night had a 25.53 times greater chance of getting a severe MFISS score than those who met with an accident during the daytime. Furthermore, patients who had an accident at night had a 41.33 times greater chance of getting a severe FISS score than those who had an accident during the daytime. The results of the multivariate analysis showed different results regarding the differences in the proportions of the MFISS and FISS based on accident time. Patients who met with an accident at night were 24.41 times more likely to present with severe MFISS scores than those who met with an accident during the day. In the FISS score analysis, patients who met with an accident at night had a greater chance of getting a severe score than those who met with an accident during the day. This result is in line with the results of the study by Nyameino et al., which found that motorcycle accidents occurred more frequently at night than during the day [28]. Furthermore, Sohal et al. reported differences in the proportion of accidents at night with and without lighting [13]. Lighting is known to affect motor vehicle accidents; nonetheless, it needs to be examined in detail. Our study showed that maxillofacial trauma due to motor vehicle accidents at night was more severe than that during the day, based on the MFISS and FISS scores.
In this study, it was found that the OR analysis results obtained had a large 95% CI on some variables. This needs to be considered because the OR obtained has a large standard error. This study is a monocentric epidemiological study at Tangerang Regency General Hospital, therefore, the sample obtained does not really describe the general population. Moreover, to overcome these limitations, research can be carried out with a larger and multicentric sample size to obtain a more representative sample.
Some of the limitations in this study can also be revised in future research by considering other variables. This study did not consider the fall's mechanism, the part that was hit first, drunkenness, and drowsiness, which were also not recorded and not analyzed, therefore, they could be confounding factors. In addition, the accident time variable, which serves as a proxy for the time of the accident, can be investigated by considering the lighting directly at the accident location.
CONCLUSION
Based on the MFISS, the severity of maxillofacial trauma was influenced by the time of the accident and helmet use in this study. Likewise, the severity of maxillofacial trauma, based on the FISS, was directly influenced by the time of the accident; however, helmet use showed an inverse relationship with the FISS score. The MFISS and FISS scores were positively correlated in the present study. Additional multicentric studies with a larger sample size and an increased number of research variables, such as the trauma mechanism, the area affected, drunkenness, and drowsiness, are warranted to confirm the findings of this study.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to itssubmission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| FISS | = Facial Injury Severity Scale |
| MFISS | = Maxillofacial Injury Severity Score |
| AIS | = Abbreviated Injury Scale |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The present research was approved by the Dental Research Ethics Committee at the Faculty of Dentistry Universitas Indonesia, Jakarta, Indonesia (No.70/Ethical Approval /FKGUI/IX/2022).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in the: https://docs.google.com/document/d/1H Sk7-Dh8aginq2uPdeaA1EozWhkV8HPG/edit?usp=shar ing &ouid=112605713309522803995&rtpof=true&sd=true
FUNDING
This study was funded by Direktorat Riset dan Pengembangan Universitas Indonesia (The Directorate of Research and Community Engagement Universitas Indonesia) through Hibah PUTI Pascasarjana 2022 (The International Indexed Publication Grant 2022), Funder ID: The Directorate of Research and Community Engagement Universitas Indonesia, Awards/Grant number: NKB-228/ UN2.RST/HKP.05.00/2022.


