All published articles of this journal are available on ScienceDirect.
Factors Influencing Dental Practitioners in the Management of Temporomandibular Joint Related Disorders in Clinical Practice – A Structural Equation Modelling Approach
Abstract
Background
Temporomandibular joint disorders (TMJD) have shown a rising prevalence globally, affecting approximately 31% of adults/elderly and 11% of children/adolescents, with disc displacement with reduction (DDwR) being the most common condition. Despite the significant impact of TMJD on individuals and society, diagnosis and treatment remain inadequate. This study aims to identify factors that are hindering clinicians from managing TMJ-related disorders and to model these factors using latent variable structural equation modeling.
Methodology
A cross-sectional study was conducted from January to March 2023 among 470 dental practitioners in Chennai, Tamilnadu. The data were collected using a closed-ended questionnaire distributed via Google Forms, achieving an 87% response rate. Confirmatory factor analysis (CFA) and structural equation modeling (SEM) were used to analyze the data, focusing on clinician-related and patient-related factors.
Results
The measurement model was refined through CFA, achieving acceptable goodness-of-fit measures. The structural model revealed that clinician-related factors significantly impact the decision to manage TMJ disorders (β=0.65), with hesitation due to poor prognosis being the most influential factor. Patient-related factors had a lesser impact (β=0.02) when compared to clinician factors, with economic affordability being the most influential patient factor.
Conclusion
The decision-making process for managing TMJ disorders is significantly influenced by clinician-related factors, with a lack of knowledge and hesitation due to poor prognosis being major barriers. Thus, enhancing the dental curriculum with comprehensive TMJ management training could improve clinician confidence and patient outcomes. Additionally, addressing patient affordability is crucial for effective treatment planning. This study highlights the need to address knowledge and competency gaps among general dental practitioners and provides insights to inform educational reforms, ultimately improving patient care outcomes.
1. INTRODUCTION
Over recent decades, the prevalence of temporo- mandibular joint disorders (TMJD) has markedly increased worldwide, affecting approximately 31% of adults and the elderly and about 11% of children and adolescents. Among the various TMJD conditions, disc displacement with reduction (DDwR) is the most diagnosed [1]. While TMJ disorders impact over one-third of the adult population, the majority do not experience severe complications [2, 3]. A notable symptom associated with TMJD is a secondary headache, which arises as a consequence of the primary disorder. Recognizing the complexity of this symptom, the International Headache Society (IHS) has classified secondary headaches related to TMJD as a distinct category (IHS 11.7) [4], underscoring the clinical significance and the need for specialized management of these cases.
Dentists have a crucial responsibility to distinguish between headaches that are likely to respond to dental treatments and those that do not. Establishing this link before commencing treatment is essential to avoid unnecessary procedures. Despite the growing impact of TMJD on individuals and society, research indicates that many people with TMJD pain are often inadequately diagnosed and treated [5, 6]. Literature reveals significant gaps in dentists' knowledge and skills regarding TMJD management, diagnostic, and treatment procedures [7, 8]. Moreover, as TMJD-related complaints continue to rise in clinical practice, it is imperative for dentists to integrate TMJ considerations into their dental treatment plans. This study addresses a critical gap by analyzing factors that hinder clinicians from managing TMJ-related disorders effectively. We hypothesized that both clinician-related and patient-related factors could impede the effective management of TMJ disorders. The comprehensive assessment aimed to identify these factors, thereby enabling clinicians to better manage TMJ-related complaints.
The primary objective of this study was to evaluate the associations among various factors influencing clinicians' attempts to manage TMJ disorders and to model these associations using latent variable structural equation modeling (SEM). SEM was chosen for this study due to its robustness in analyzing complex relationships between observed and latent variables. This methodology allows for the simultaneous examination of multiple variables and their interactions, providing a comprehensive under- standing of how different factors influence clinical decision-making. Furthermore, by using SEM, we aimed to model the direct and indirect effects of clinician-related and patient-related factors on the management of TMJ disorders. This approach provides measurable insights into how these factors impact decision-making in TMJ disorder management, ultimately informing strategies to enhance clinical practice and improve patient outcomes.
2. METHODOLOGY
This cross-sectional study was conducted from January 2023 to March 2023, targeting dental practitioners in Chennai, Tamil Nadu. A representative sample of 470 dental practitioners was obtained with the support of the Indian Dental Association (Table 1). The sample size was calculated to ensure adequate power for detecting mediating effects in structural equation models, following recommendations that a sample size of 470 subjects is sufficient for most mediating models [9]. The consent for their participation was obtained from all participants along with the questionnaire. The clinicians currently practicing in Chennai (India) and who provided informed consent to participate in the study were included. This study was approved by the Saveetha Dental College Institutional Human Ethical Committee (Reference Number: IHEC/SDC/FACULTY/24/PROSTHO/010).
| Variables | N (%) |
|---|---|
| Gender | |
| Male | 310 (66) |
| Female | 160 (34) |
| Education | |
| BDS | 270 (58) |
| MDS | 200 (42) |
| Nature of practice | |
| Government | 26 (5) |
| Private | 444 (94) |
2.1. Data Collection
Data were collected using a closed-ended questionnaire distributed via Google Forms through WhatsApp in the respective IDA local branch groups. A reminder was sent after a week to encourage completion of the form, resulting in an 87% response rate. Prior to the main study, a pilot study was conducted with 20 individuals not part of the original study to test the tool for face and content validity and intra-examiner reliability, yielding a kappa coefficient of 88.5%. The questionnaire assessed factors hindering clinicians from attempting TMJ disorder management using eight close-ended questions (Table 2). Five questions represented clinician-related factors, and three represented patient-related factors, which were considered latent variables. The responses were measured on a 4-point Likert scale: 1 (strongly agree), 2 (agree), 3 (disagree), and 4 (strongly disagree).
2.2. Statistical Analysis
The collected data were organized using Microsoft Excel and subjected to further descriptive analysis of all variables was performed using JASP software. Confirmatory factor analysis (CFA) and latent variable structural equation modeling (LV-SEM) were conducted to test the causal relationships among observed and latent variables using Onyx software.
2.2.1. Measurement Model
Fig. (1) illustrates the theoretical conceptual model developed for the latent variable structural equation modeling (SEM). Each latent variable is represented as an ellipse, indicating constructs that are not directly observable but are inferred from measured indicators, shown as rectangles. This comprehensive model aims to capture the complex interplay among the constructs, providing a robust framework for testing the proposed hypotheses and understanding the underlying structure of the data. With this conceptual model as a base, a measurement model was developed using confirmatory factor analysis to assess how well the observed variables represent the underlying latent variables. The model's fit was evaluated using several indices commonly employed in structural equation modeling (SEM) analysis. The model was only considered for further analysis only if it met the recommended Goodness-of-Fit (GOF) measures in chi-squared fit statistic (χ2/df), root-mean-square error of approximation (RMSEA), goodness-of-fit index (GFI), normed fit index (NFI), and comparative fit index (CFI), all of which were required to be close to or better than the recommended thresholds [10]. The model's reliability was evaluated using reliability coefficients, specifically Coefficient ω (Omega) and Coefficient α (Alpha). Omega is considered a more robust measure of reliability than Cronbach's Alpha as it accounts for varying loadings of items on their respective factors, providing a better estimate of true score variance. Despite its limitations, such as assuming equal loadings and unidimensionality, Cronbach's Alpha remains a valuable indicator of internal consistency.
2.2.2. Latent Variable Structural Equation Model
The latent variable structural equation modeling (SEM) analysis was conducted to test the causal relationships among the observed and latent variables within the model. Maximum likelihood estimation was employed for the parameter estimations, complemented by 1,000 bootstrap samples re-sampled from the original dataset to derive less biased standard errors and 95% percentile confidence intervals. In SEM, maximum likelihood estimation assumes that the data follows a multivariate normal distribution. This approach ensures that the conclusions drawn are based on reliable and valid statistical inferences, ultimately informing better clinical decision-making and improving patient outcomes.
3. RESULTS
Table 1 provides a detailed overview of the demographic and professional composition of the study participants. Of the total participants, 270 (58%) held a Bachelor and 200 (42%) held a Master of Dental Surgery (MDS) degree. The gender distribution comprised 310 males (66%) and 160 females (34%). In terms of practice setting, 26 participants (5%) worked in government practices, whereas 444 participants (94%) were engaged in private practices. This demographic and professional breakdown offers a comprehensive understanding of the study population.
3.1. Measurement Model
The confirmatory factor analysis resulted in a measurement model that examined the relationship between the measured variables and their corresponding latent variables. Not all the measured variables in Table 2 demonstrated a good fit. Consequently, some variables were eliminated based on their factor loading estimates and standardized residual covariances. The estimated values of the Goodness of Fit (GOF) measures are presented in Table 3, along with the recommended levels. Within the final model, certain variables exhibited stronger associations with their respective latent variables. For clinician-related factors, C2 (Hesitation due to poor prognosis) and C3 (Prolonged treatment duration) had higher factor loadings compared to C5 (Difficulty in diagnosis). Regarding patient-related factors, P1 and P3 were retained, with P1 (Economically not affordable) showing a stronger association with the latent variable (Table 2).
3.2. Latent Variable Structural Equation Model
The SEM analysis revealed significant impacts of both clinician and patient-related factors on the decision-making process for managing TMJ-related disorders in clinical practice. Standardized estimates from the SEM (Fig. 2) indicated that clinician-related factors had a substantial impact on clinician’s decisions (β = 0.65), whereas patient-related factors had a comparatively weaker impact (β = 0.02). This suggests that clinicians' knowledge, confidence, and perceived prognosis are critical determinants in their management of TMJ disorders. Among clinician-related factors, “Hesitation due to poor prognosis” (C2) had the highest association with the latent variable, with a regression weight of 0.93, underscoring its significant influence on decision-making. Similarly, within patient-related factors, “Economically not affordable” (P2) had a higher association with the latent variable (regression weight of 0.78) compared to other patient factors, highlighting the substantial role of economic considerations in treatment decisions.
| Outcome Variable | Do you Attempt to Treat TMJ-related Disorders? |
|---|---|
| Observed Variable Code | Parameter |
| - | Latent variable: Clinician factors |
| C1 | Lack of lab support in splint fabrication |
| C2 | Hesitation due to poor prognosis |
| C3 | Prolonged treatment duration |
| C4 | Lack of importance in academic theoretical learning |
| C5 | Difficulty in diagnosis due to many differential diagnosis |
| - | Latent variable: Patient factors |
| P1 | Poor patient compliance for noninvasive splints |
| P2 | Economically not affordable |
| P3 | Patient neglect for treatment |
| Fit Index | Index | Recommended Levels | Estimate Values |
|---|---|---|---|
| Absolute fit index | c2/df | < 5 | 1.805 |
| RMSEA | < 0.08 | 0.070 | |
| GFI | > 0.9 | 0.991 | |
| Incremental fit indices | NFI | > 0.9 | 0.994 |
| CFI | > 0.9 | 0.997 |
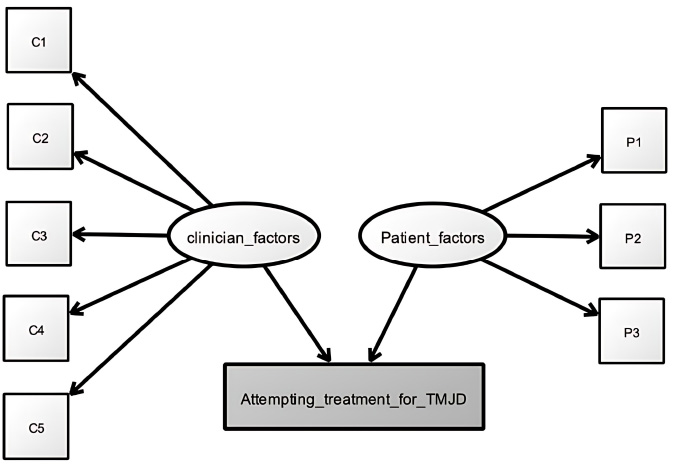
Theoretical conceptual model of observed and latent variables.
4. DISCUSSION
This study provides a detailed analysis of factors influencing clinical practitioners in managing temporo- mandibular joint (TMJ) disorders. The data, derived entirely from clinicians' perceptions, reveal that clinician-related factors have a substantial positive factor loading of 0.96 in the structural equation modeling (SEM) analysis. In SEM, a factor loading signifies the relationship between an observed variable and its underlying latent variable. A loading of 0.65 indicates a very strong association, underscoring the significant negative impact of clinician-related factors on clinical decision-making. This finding emphasizes the critical need to address and mitigate these obstacles to enhance clinical practice.
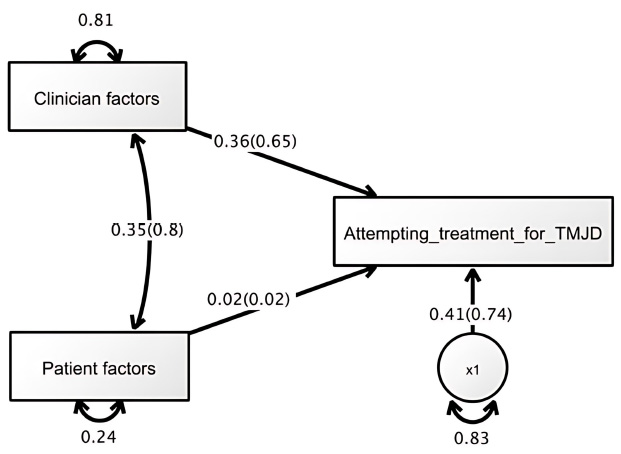
Latent variable structural equation model.
Additionally, research in craniomandibular disorder management has consistently demonstrated a notable disparity in the knowledge levels between general dental practitioners and experts in this field. Several surveys highlight this knowledge gap, underscoring the urgent need for further education and training to ensure optimal patient care [12-15]. This is in accordance with the observations of our study, which confirms that factors such as hesitation due to poor prognosis, prolonged treatment duration, and diagnostic challenges are significant obstacles for clinicians managing TMJ disorders. Notably, most participants in our study were general dentists without specialization, which has important implications. These practitioners may lack the depth of knowledge and expertise that specialists possess, potentially affecting the quality of care they provide. One contributing factor to these clinician-related challenges is the limited access the general dentists have to research evidence in diagnosing and managing TMJ disorders. Keeping up with the vast and rapidly evolving knowledge in temporomandibular disorders and orofacial pain (TMD/ OFP) is nearly difficult for general dental practitioners (GDPs), leading to inevitable, albeit acceptable, delays in translating research findings into clinical practice [16]. Baharvand et al. indicated that TMD specialists are significantly more knowledgeable than general dental practitioners (p<0.05) [17].
Similarly, Tegelberg's [18] research highlights signi- ficant knowledge differences between TMD specialists and general dental practitioners, particularly in treatment and prognosis. This gap in TMD management skills and knowledge can be effectively addressed by incorporating relevant training into the regular dental curriculum. A study by De Medeiros Tormes et al. [19] demonstrated that pre-doctoral dental students showed low agreement with current gold standards for TMD. Most students did not feel confident treating TMD patients (62.6%), were dissatisfied with the TMD content in their curriculum (55.8%), and identified a lack of clinical practice as a primary limitation in their training (59.2%).
Among clinician-related factors, hesitation due to poor prognosis is the most significant hindrance. This underscores the need to strengthen the theoretical foundation for general dentists in managing TMJ disorders. Enhancing TMD education in undergraduate curriculums will help dental students gain more experience and confidence in treating TMD, ultimately leading to better patient outcomes. A study by Taimeh et al. (2022) [20] highlights the drawbacks of specialist healthcare services from the perspective of TMD patients, suggesting that delays in specialist appointments may worsen symptoms. Regarding patient-related factors, affordability has the most significant impact on treatment decisions (β=0.78), indicating that a patient's ability to pay for diagnostic and therapeutic services greatly influences the recommended treatment plan.
From the clinician's perspective, in addition to considering patient-related factors, psychological factors such as stress management and anxiety response are crucial in managing masticatory muscle tension and joint overload. However, some patients may be hesitant to accept counseling approaches and cognitive treatments that do not yield immediate results. This reluctance can lead to avoidance of self-realization or rejection of physiotherapy-based solutions. Additionally, some patients may be unwilling to take medications, preferring instead for the doctor to “fix the problem,” which requires substantial time and patient cooperation. Lastly, although not included in our model fit criteria, the literature supports the notion that individuals with mild pain or a clicking joint often attempt self-coping strategies without professional advice, potentially exacerbating clinical symptoms [21, 22]. Thus, addressing both clinician and patient-related factors is essential to improve the management of TMJ disorders. Enhancing education and training for general dentists and addressing psychological and affordability concerns from the patient's perspective can lead to more effective and comprehensive care [23, 24].
5. LIMITATIONS
This study was confined to dental practitioners in Chennai, Tamil Nadu, which, while providing valuable insights into this specific demographic, limits the generalizability of the findings to other regions or countries. Variations in educational backgrounds, clinical practices, and healthcare systems could influence the applicability of the results. Additionally, the study focused on a predefined set of clinician-related and patient-related factors, potentially overlooking other significant influences on TMJ disorder management, such as institutional policies, access to continuing education, and advance- ments in diagnostic technologies.
6. FUTURE RECOMMENDATIONS
Future research should include a more diverse and geographically dispersed sample to enhance the generalizability of the findings. Including practitioners from various healthcare settings, such as public health clinics and academic institutions, can provide a more comprehensive understanding of TMJ disorder manage- ment. Combining quantitative data with qualitative insights through interviews and focus groups with practitioners can reveal nuanced perspectives and identify additional factors influencing clinical decision-making. Furthermore, future studies should focus on patient-reported outcomes and satisfaction with TMJ disorder management. Understanding the patient's perspective can help tailor interventions to better meet their needs and improve the overall quality of care. Additionally, by addressing these limitations and implementing the recommended strategies, future research can significantly advance the understanding and management of TMJ disorders, ultimately leading to improved patient outcomes and more effective clinical practices.
CONCLUSION
Our comprehensive evaluation underscores the clinicians’ decision-making process is more influenced by their own factors rather than those of the patient-related factors when it comes to the management of temporo- mandibular joint disorders. Clinician-related factors, such as knowledge and confidence, have a much stronger influence on treatment decisions compared to patient-related factors. Specifically, hesitation due to poor prognosis emerged as a critical deterrent among clinicians, indicating the need for enhanced education and training to address these uncertainties. Additionally, economic considerations were found to be the most significant patient-related factor affecting treatment decisions. This underscores the importance of making TMJ treatments more affordable and accessible. Overall, the study highlights the necessity for targeted professional development, curriculum enhancements, and policy changes to improve TMJ disorder management, ultimately aiming for better patient outcomes and more efficient healthcare delivery.
AUTHOR’S CONTRIBUTIONS
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| TMJD | = Temporomandibular Joint Disorders |
| DDwR | = Disc Displacement With Reduction |
| CFA | = Confirmatory Factor Analysis |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Saveetha Dental College Institutional Human Ethical Committee (Reference Number: IHEC/SDC/FACULTY/24/PROSTHO/010).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
The consent for their participation was obtained from all participants along with the questionnaire.


