All published articles of this journal are available on ScienceDirect.
A Comparative Analysis on the Effects of Two Different Grafts on Gingival Phenotype, Dentin Hypersensitivity, and Quality of Life: A 6-month Split-mouth Study
Abstract
Objectives
This study aimed to compare the effects of two surgical treatments of multiple gingival recessions on gingival phenotype over 6 months. Moreover, dentin hypersensitivity and quality of life scores were also monitored over time.
Materials and Methods
In this longitudinal split-mouth study, 90 upper-class Recession Type 2 (RT2) bilateral gingival recessions (GR) were randomly (right or left side) assigned to coronally advanced flaps with connective tissue graft (CTG group) or xenogeneic collagen matrix (XCM group). The primary outcome was GR reduction after surgical procedures. At the preoperative visit, 3- and 6-months gingival thickness through cone-beam computed tomography using lip retractors were determined. Oral health-related quality of life (OHRQoL) and stimulated dentin hypersensitivity were evaluated by the Oral Health Impact Profile (OHIP-14) instrument and visual analogic scale, respectively.
Results
A thicker gingival phenotype was seen at 6 months, indicating phenotype improvement. Both techniques showed similar results (p > 0.05) over time regarding root covering (CTG = 74.19% and XCM = 77.41%). At 6 months, dentin hypersensitivity only decreased in the XCM group. Independently of the treatment group, statistically significant improvements were observed (Friedman test; p < 0.05) in physical pain and limitation, psychological discomfort, and limitation domains favoring OHRQoL.
Conclusion
Gingival phenotype improved over time independently of the technique. Both surgical treatments provided similar and adequate recovery of multiple gingival recessions. At 6 months, patients experienced a better quality of life profile related to oral health. Moreover, the XCM group experienced lower dentin hypersensitivity.
1. INTRODUCTION
Despite many possible associations between soft and hard tissues, the gingival phenotype is divided into thick, medium, or thin. A thick gingival phenotype offers greater resistance to inflammation or trauma, which could imply gingival recession (GR), periodontal pocket development, and the loss of papillae. Therefore, GRS is more likely to occur in patients with a thin phenotype [1].
In addition to phenotype, GR is caused by several factors and may have important aesthetic and functional implications disturbing periodontal health [2-5]. Unfor- tunately, GR highly affects one or multiple sites of middle-aged and older groups [2, 3]. The exposed root surface is often associated with aesthetic complaints, dentin hypersensitivity, cervical root caries, and impaired biofilm control [6], leading patients to seek periodontal care [3, 7].
Although different techniques can be used aiming at root coverage [8, 9], gingival thickness impacts their results [9]. If minimal keratinized tissue (KT) is detected, a soft tissue graft, such as a connective tissue graft along with a coronally advanced flap or free gingival graft is recommended. Moreover, a coronally advanced flap may be used alone when appropriate attached gingiva width is available [8]. While dental practice guidelines dated from 2014 [10], reported unclear results regarding dentin hypersensitivity reduction by surgically covering buccal GR, a more recently published systematic review showed promising findings [11]. Overall, the meta-analysis of 13 randomized clinical trials showed that successful surgical treatment of GR is highly related to the suppression of dentin hypersensitivity [11].
Autogenous graft usually has the palatal mucosa, which is the main connective tissue donative area [12]. However, to overcome technical limitations, several biomaterials derived from enamel matrix, acellular dermal matrix, barrier membranes, and collagen matrix have been tested [13-15]. Among them, the xenogeneic collagen matrix (XCM) has demonstrated promising results in single and multiple GR by promoting gingival width and thickness improvements. Although clinical assessments provide gingival phenotype information, cone-beam computed tomography (CBCT) also offers the evaluation of bone morphology [1]. Interestingly, after separating lips and cheek, some authors [12, 16-18], suggested that CBCT scans are appropriate to determine the thickness of both palatal masticatory mucosa and buccal gingiva [17, 18].
Thus, this longitudinal split-mouth study was designed to compare the effects of two surgical treatments, coronally advanced flaps with connective tissue graft or xenogeneic collagen matrix, of multiple GR on gingival phenotype over 6 months. Moreover, it also monitored dentin hypersensitivity and Oral Health-Related Quality of Life (OHRQoL) scores over time.
2. MATERIALS AND METHODS
This longitudinal split-mouth clinical study was reviewed and approved by the Institutional Research Ethics Committee (# 4.592.151), and participants were enrolled after written informed consent. The study population was composed of 15 participants who matched the inclusion criteria and completed the 6-month post- surgical follow-up period. The present study hypothesized that a coronally advanced flap with connective tissue graft leads to a greater reduction in gingival recession than a coronally advanced flap with a xenogeneic collagen matrix within 6 months.
The sample size was calculated considering changes (baseline versus 6 months) in gingival phenotype (depth of GR) based on descriptive values (mean ± standard deviation) observed (2.1 ± 1.0mm; 1.7 ± 1.1mm; 2.6mm ± 0.9mm; 2.5mm ± 0.9mm) in previous studies [6, 9]. These values were applied to the following formula: DMS= t_ (5%) √((2*DMe)/N); DMS being the 10% (1mm) pre-defined minimal observed statistically significant difference, t (5%), 2 is a tabled value and DMe the standard deviation. Considering all results after applying literature values, it was demonstrated the need for a 6-month completion of 42 analytical sites (42 teeth with gingival recessions) per group. For the qualitative OHRQoL variable, OpenEpi (Open Source Epidemiologic Statistics for Public Health 3.0) was used. Considering surgical GR treatment, combining both techniques, 15 participants were required to complete the study.
The inclusion criteria consisted of individuals aged ≥18 years, with aesthetic and dentin hypersensitivity complaints, systemically healthy individuals with no contraindications for periodontal surgery, no clinical signs of active periodontal disease, multiple upper bilateral maxillary GR (Recession Type 2 - RT2 [19], equivalent to Miller's Class III [20]), good plaque control, and apical keratinized tissue width (KTW) of at least 1 mm.
The following exclusion criteria were used: pregnancy or breastfeeding, smoking, systemic disease with compromised healing potential or infectious disease, use of medications known to affect gingival conditions (hyperplasia) or interfere with healing (steroids), non-vital teeth, caries, prosthetic crowns, or dental fillings involving the cement-enamel junction area, extruded, rotated or mobile teeth, and individuals unable to attend dental appointments.
2.1. Study Design
As a split-mouth study, a dental assistant following a computer-generated list randomly allocated each participant an oral side to one treatment group: coronally advanced flap plus connective tissue graft (CTG) (n = 45 maxillary RG) or Geistlich (Geistlich Pharma do Brasil, São Paulo, Brazil) Fibro-Gide Membrane® (XCM) (n = 45 maxillary RG).
At the preoperative visit, participants received oral hygiene instructions from a trained researcher and were motivated to maintain adequate biofilm control. Data from the medical history and Oral Health Impact Profile (OHIP-14 [21]) questionnaire were taken. A trained interviewer applied the version of the questionnaire validated in Portuguese in a standardized manner. Participants were encouraged to give immediate answers and to ask questions repeatedly in case of any doubts.

Baseline pre-operative intraoral images of a study participant: (A, B) right and left sides; C, D) gingival recessions (GR) measurements with a caliper on the right and left sides; (E, F) obtaining PD on both sides.
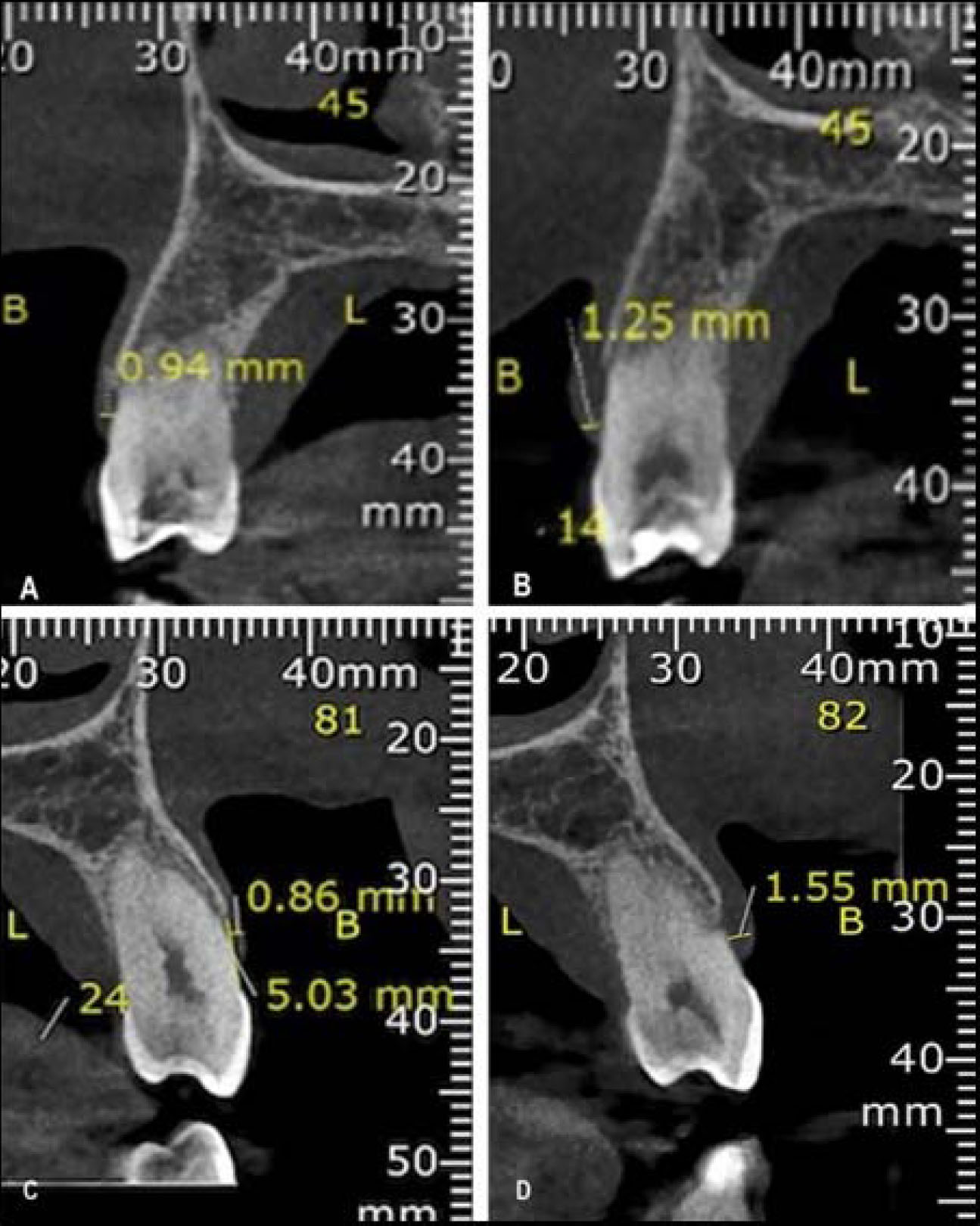
CBCT (cone-beam computed tomography) images of two pre-molar teeth: (A, B) pre-operative and 6-month measurements on the connective tissue graft (CTG group); (C, D) pre-operative and 6-month measurements on xenogeneic collagen matrix (XCM group).
A blinded periodontist, with a North Carolina manual periodontal probe (PCPUNC 15® Hu Friedy, Chicago, IL) and a calibrated digital caliper (Caliper MTX, Global tools, Rio de Janeiro, Brazil®) (Fig. 1), measured whole mouth probing depth (PD), clinical attachment level (CAL), plaque index (PI), bleeding on probing (BoP) in addition to depth of GR and KTW. Thus, GR classification was confirmed. A blinded researcher collected aesthetics self-reported scores by using a 10 cm visual analogue scale (VAS). After 1 second of RG air stimulation, at approximately 1 cm distance under cotton roll isolation, dentin hypersensitivity was also evaluated by VAS [22].
A blinded imaging specialist determined gingival thickness from CBCT [16] taken 15 days before the surgical procedure. To measure the thickness of the labial gingiva, a clinical measurement of 1 mm above the gingival margin was used (Fig. 2).
At the baseline visit, participants underwent surgical treatment according to a randomization process. Surgical time on each maxillary side (CTG or XCM) was recorded for group comparison. Postoperative pain and swelling were controlled with nimesulide (EMS Pharma, São Paulo, Brazil) (2x/day for 3 days). Moreover, participants were instructed not to brush their teeth in the surgically treated areas, to gently rinse with 0.12% chlorhexidine solution (Colgate do Brasil, São Paulo, Brazil) for 1 minute (2x/day), and to eat soft food until suture removal within two weeks [22].
Three months after surgical procedures, participants received oral hygiene reinstructions and underwent new clinical PD, CAL, PI, BoP, depth of GR, and KT width exams. Aesthetics, dentin hypersensitivity, and OHIP-14 questionnaire were also evaluated [21]. At 6 months, the same procedures were performed in addition to gingival thickness measurement by CBCT.
2.2. Coronally Advanced Flap with Grafts
Surgeries were scheduled in the morning, and bilateral coronally advanced flap procedures plus grafts (CTG or XCM) were performed on the same morning. Participants rinsed for 1 min with 20 mL 0.12% chlorhexidine mouthwash solution. A 2% chlorhexidine gel (Byoformula, São José dos Campos, Brazil) was applied to the face using a sterile gauze (Cremer, São Paulo, Brazil).
After intraoral local anesthesia with 2% lidocaine combined with 1:100,000 epinephrine (DLA Pharma, Curitiba, Brazil), oblique submarginal incisions were made in the maxilla in the interdental areas of each GR, followed by intrasulcular incisions extending on each side of the teeth to be treated. A full/partial thickness flap was elevated in the coronal-apical direction. A dissection of the buccal mucosa was performed to eliminate muscle tension. The remaining tissue of the anatomical interdental papillae was de-epithelialized. A connective tissue graft was obtained from the palate, which was stabilized with a resorbable suture over the GR with suspension sutures on the teeth. XCM graft was stabilized with a resorbable suture over the GR with suspension sutures on the teeth. Finally, on both sides, suspension sutures with non-resorbable sutures were also used for a precise adaptation of the buccal flap over the exposed root and to stabilize each surgical papilla over each de-epithelialized interdental area.

Intraoral clinical images of a study participant at each time-point of evaluation: (A, B) baseline; (C) 3 months connective tissue graft (CTG group); (D) 3 months xenogeneic collagen matrix (XCM group); (E) 6 months connective tissue graft (CTG group); (D) 6 months xenogeneic collagen matrix (XCM group).
Fig. (3) exemplifies pre and post-operative (3 and 6 months) intraoral clinical images for the three study participants.
2.3. Statistical Analysis
Kappa test was used to evaluate intraexaminer reproducibility scores 7 days before preoperative visits, 3- and 6-month visits regarding the following clinical parameters: PD, CAL, depth of GR, and KTW. PD and CAL measurements (mm) were obtained at six points per tooth for all teeth except for the third molar.
First, the association between the graft groups (CTG and XCM) was evaluated. Data analysis included a descriptive characterization of the variables of interest. The normality of the data was evaluated using the Kolmogorov–Smirnov test. Parametric and non-parametric tests (Chi-Square, Student’s t, and Friedman) were used when appropriate. The groups (CTG and XCM) were also analyzed over time. The results were statistically significant when p < 0.05, and the analysis was performed using the SPSS 14.0 software for Windows.
The OHIP-14 questions were combined into seven domains, each measuring a different dimension, namely: functional limitation (Q1-Q2), physical pain (Q3-Q4), psychological discomfort (Q5-Q6), physical limitation (Q7-Q8), psychological limitation (Q9-Q10), social limitation (Q11-Q12), and disadvantage (Q13-Q14). Thus, the total score was calculated by adding single scores for each question. The highest possible total OHIP-14 score was 56, indicating a very poor OHRQoL. Total scores were compared over time.
3. RESULTS
A total of 90 teeth were followed up throughout the 6-month period; therefore, 45 teeth received CTG and 45 XCM grafts.
CTG group presented 74.19% root coverage and the XCM group presented 77.41% without any differences between techniques (p = 0.358). Table 1 demonstrates no statistically significant difference between the groups (CTG and XCM) at each time point. The boxplots shown in Figs. (4 and 5) present the mean clinical and CBCT measurements at baseline and at 6 months, demonstrating that both techniques provided improvements. In both groups, CTG and XCM, there was a decrease in depth GR, an increase in KTW, and a thicker gingival phenotype (p < 0.05) (Table 2). At 6 months, dentin hypersensitivity only decreased in the XCM group.
| Variables | Visits | CTG (45 teeth) | XCM (45 teeth) | p-value | |
|---|---|---|---|---|---|
| Mean ± Standard Error | Mean ± Standard Error | ||||
| Visual Analogue Scale (score) |
Aesthetics | Baseline | 5.70a ± 2.56 | 5.60a ± 2.56 | - |
| 3-months | 5.27 ± 2.08 | 5.30 ± 2.09 | 0.813 | ||
| 6-months | 2.80a ± 2.26 | 2.80a ± 2.06 | - | ||
| Dentin Hypersensitivy | Baseline | 3.90 ± 3.34 | 4.71 ± 3.81 | 0.082 | |
| 3-months | 3.77 ± 3.21 | 4.33 ± 3.42 | 0.182 | ||
| 6-months | 3.10 ± 3.28 | 3.47 ± 3.62 | 0.190 | ||
| Clinical parameters (mm) |
Probing depth | Baseline | 1.74 ± 0.79 | 1.71 ± 0.72 | 0.775 |
| 3-months | 1.65 ± 0.67 | 1.67 ± 0.57 | 0.784 | ||
| 6-months | 1.44 ± 0.52 | 1.48 ± 0.62 | 0.666 | ||
| Clinical attachment level |
Baseline | 4.05 ± 1.22 | 4.23 ± 0.95 | 0.417 | |
| 3-months | 3.81 ± 1.51 | 4.10 ± 1.19 | 0.171 | ||
| 6-months | 2.99 ± 1.25 | 3.22 ± 0.86 | 0.240 | ||
| Plaque Index | Baseline | 1.00a ± 0.00 | 1.00a ± 0.00 | - | |
| 3-months | 1.00a ± 0.00 | 1.00a ± 0.00 | - | ||
| 6-months | 1.00a ± 0.00 | 1.00a ± 0.00 | - | ||
| Bleeding on probing | Baseline | 0.20a ± 0.61 | 0.20a ± 0.61 | - | |
| 3-months | 0.00a ± 0.00 | 0.00a ± 0.00 | - | ||
| 6-months | 0.10a ± 0.30 | 0.15a ± 0.30 | - | ||
| Depth of Gingival Recession | Baseline | 2.32 ± 0.89 | 2.49 ± 0.85 | 0.326 | |
| 3-months | 2.16 ± 0.99 | 2.46 ± 0.87 | 0.108 | ||
| 6-months | 1.58 ± 1.09 | 1.75 ± 0.82 | 0.338 | ||
| Keratinized Tissue width | Baseline | 2.26 ± 0.74 | 2.12 ± 0.73 | 0.318 | |
| 3-months | 2.85 ± 0.95 | 2.87 ± 1.64 | 0.944 | ||
| 6-months | 2.97 ± 0.81 | 2.71 ± 1.50 | 0.232 | ||
| Gingival phenotype (mm) | CBCT | Baseline | 1.11 ± 0.34 | 1.22 ± 0.42 | 0.232 |
| 6-months | 1.41 ± 0.38 | 1.43 ± 0.48 | 0.893 | ||
a mm: millimeter; CBCT: cone beam computed tomography.

Preoperative (T0) and 6 months (T2) keratinized tissue width (KTW) boxplots for connective tissue graft (CTG) and xenogeneic collagen matrix (XCM).
Note: Mean ± standard deviation; mm: millimeter.
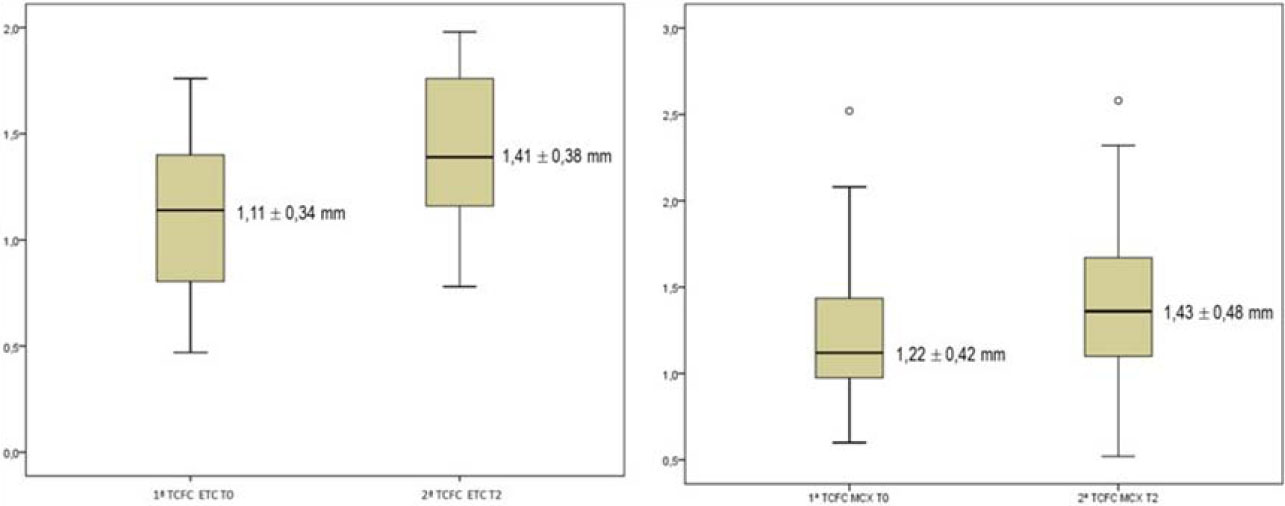
Baseline (T0) and 6 months (T2) boxplots for the gingival phenotype (CBCT) variable of CTG and XCM groups.
Note: Mean ± standard deviation; mm: millimeter.
CBCT: cone-beam computed tomography (gingival phenotype); CTG: connective tissue graft; XCM: xenogeneic collagen matrix.
Table 3 presents the description of the OHIP-14 questionnaire over time. There was no report of a very poor OHRQoL at any time point. The highest scores were in physical pain and psychological discomfort domains with 4.45 and 3.00 mean values, respectively. Fortunately, these two domains were reduced after surgical procedures. Friedman test showed statistically significant reductions (p < 0.05) regarding physical pain (Q3-Q4), psychological discomfort (Q5-Q6), physical limitation (Q7-Q8), and psychological limitation (Q9-Q10) domains, thus favoring the OHRQoL (Table 3).
4. DISCUSSION
A split-mouth design allows for minimizing individual variables, which increases the power of the study. This design could be particularly interesting for the analysis of subjective data, such as VAS and OHIP-14 scores. This information is also shared by Tonetti et al. [6].
In the present study, GR reductions were the primary outcome. To evaluate the gingival phenotype, a clinical measurement of 1 mm above the gingival margin was carried out [18]. A lip retractor made gingival tissue visualization possible, thus through CBCT both bone and gingival tissues were evaluated. De Silva et al. [18] compared clinical and CBCT gingival thickness measurements. Significant correlations were observed for measurements of 1 and 3 mm above the gingival margin; that is, CBCT has proven to be a reliable method for measuring soft tissues, especially in areas involving aesthetics. Moreover, Gupta et al. [12] did not find differences between CBCT and probing when comparing palatal mucosa thickness. Januário et al. [17] emphasized that the use of lip retractors allows a quantitative assessment. However, it is not possible to distinguish specific aspects, such as an inflamed gingiva from a healthy one, or the type of soft tissue, such as epithelial or connective tissue [17]. In the present study, CBCT images from multiple GR sites obtained with a lip retractor were demonstrated to be useful and applicable in daily practice.
| Variables | 6 Months versus Baseline | |||
|---|---|---|---|---|
| Group | Mean ± Standard Error | p-value | ||
| Visual Analogue Scale (score) | Aesthetics | CTG | -2.84 ± 3.17 | 0.000* |
| XCM | -2.74 ± 3.07 | 0.000* | ||
| Dentin Hypersensitive | CTG | -1.06 ± 3.10 | 0.065 | |
| XCM | -1.35 ± 2.98 | 0.017* | ||
| Clinical parameters (mm) | Pocket Depth | CTG | -0.26 ± 1.11 | 0.204 |
| XCM | -0.23 ± 1.00 | 0.218 | ||
| Clinical Attachment Level | CTG | -0.99 ± 1.40 | 0.000* | |
| XCM | -1.01 ± 1.10 | 0.000* | ||
| Plaque index | CTG | - | - | |
| XCM | - | - | ||
| Bleeding on Probing | CTG | -0.10 ± 0.30 | 0.083 | |
| XCM | -0.10 ± 0.30 | 0.083 | ||
| Depth of Gingival Recession | CTG | -0.72 ± 0.84 | 0.000* | |
| XCM | -0.72 ± 0.79 | 0.000* | ||
| Keratinized Tissue width | CTG | 0.69 ± 0.80 | 0.000* | |
| XCM | 0.60 ± 1.30 | 0.015* | ||
| Gingival phenotype (mm) | CBCT | CTG | 0.31 ± 0.28 | 0.000* |
| XCM | 0.20 ± 0.53 | 0.041* | ||
Abbreviation: CTG: connective tissue grafts; XCM; xenogeneic collagen matrix; mm: millimeter; PI: plaque index; CBCT: Cone-beam computed tomography.
| OHIP-14 Domains | 15 Participants (CTG and XCM) 90 Teeth | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 3-months | 6-months | ||||||
| Functional limitation | Q1-Q2 | 0.73 ± 1.27 | 0.00 ± 0.00 | 0.00 ± 0.00 | ||||
| Physical pain | Q3-Q4 | 4.45 ± 1.69 | 1.55 ± 2.11 | 0.36 ± 0.81 | ||||
| Psychological discomfort | Q5-Q6 | 3.00 ± 2.93 | 0.64 ± 1.12 | 0.00 ± 0.00 | ||||
| Physical limitation | Q7-Q8 | 1.82 ± 1.78 | 0.45 ± 0.82 | 0.00 ± 0.00 | ||||
| Psychological limitation | Q9-Q10 | 1.45 ± 2.16 | 0.00 ± 0.00 | 0.00 ± 0.00 | ||||
| Social limitation | Q11-Q12 | 0.36 ± 0.81 | 0.00 ± 0.00 | 0.00 ± 0.00 | ||||
| Disadvantage | Q13-Q14 | 0.18 ± 0.60 | 0.00 ± 0.00 | 0.00 ± 0.00 | ||||
| OHIP-14 domains | 15 participants (CTG and XCM) 90 teeth | |||||||
| Baseline | 3 months | 6 months | χ2 | p-value | ||||
| Functional limitation | Q1-Q2 | 2.27 | 1.86 | 1.86 | 6.00 | 0.050 | ||
| Physical pain | Q3-Q4 | 2.82 | 1.73 | 1.45 | 14.82 | 0.001* | ||
| Psychological discomfort | Q5-Q6 | 2.55 | 1.91 | 1.55 | 8.86 | 0.012* | ||
| Physical limitation | Q7-Q8 | 2.68 | 1.82 | 1.50 | 13.92 | 0.001* | ||
| Psychological limitation | Q9-Q10 | 2.36 | 1.82 | 1.82 | 8.00 | 0.018* | ||
| Social limitation | Q11-Q12 | 2.18 | 1.91 | 1.91 | 4.00 | 0.135 | ||
| Disadvantage | Q13-Q14 | 2.09 | 1.95 | 1.95 | 2.00 | 0.368 | ||
Abbreviation: OHIP: Oral Health Impact Profile; CTG: connective tissue graft; XCM; xenogeneic collagen matrix.
Although CTG is the first treatment of choice for single GR, the treatment of multiple GRs remains a challenge due to the large surgical field, anatomical factors, and the limited amount of connective tissue in the donor area [6, 22-24]. A systematic review [25], concluded that CTG offers the best clinical results in the treatment of multiple Miller Class I and II GRs [20]. In this study, both CTG and XCM provided favorable results when the coronally advanced flap was used in multiple RT2 GRs [17]. Despite its benefits, CTG is associated with longer operative time, pain, and discomfort related to the donor area, which is supported by other researchers [6, 16, 22, 26, 27]. In addition, graft removal may cause trans- and postoperative complications [16, 22, 26, 28], especially in the treatment of multiple GRs that increase the need for donor tissue [6, 22]. For these reasons, alternative surgical techniques and materials have been suggested and compared with CTG [6, 22, 26, 29]. In this context, XCM has been proposed as a potential substitute for soft tissue grafts to increase keratinized tissue of single [24, 28] and multiple GRs [6, 22, 29]. In addition, its use is associated with less pain and shorter operative time, as it does not depend on the donor area [6, 22, 26, 29]. In the present study, the mean surgical time was significantly lower for the XCM group (45.55 ± 12.26 minutes) than for the CTG group (87.17 ± 13.20 minutes) (p=0.000). Similarly, Nahas et al. [22] also showed a lower time (p < 0.001) for XCM (31.30 ± 4.30 minutes) in comparison to CTG (48.10 ± 6.10 minutes). Both procedures caused pain, which was greater for the CTG group, as reported by participants.
Regarding stimulated dentin hypersensitivity scores at 6 months, XCM provided a statistically significant mean reduction of 1.35 ± 2.98 (p = 0.017) that was not observed in the CTG group (1.06 ± 3.10 [p = 0.065]). Moreover, after six months, Nahas et al. [22] obtained a mean reduction of 2.0 ± 3.0 for CTG and 2.3 ± 3.3 for XCM with no difference between the groups (p = 0.647). These improvements are possibly related to an increase in keratinized tissue and root coverage [30, 31].
In this study, the CTG group presented 74.19% root coverage and the XCM group demonstrated 77.41% without differences between techniques (p = 0.358). After tunneling, Aroca et al. [32] demonstrated 85.00% of root coverage for CTG-treated and 42.00% for XCM-treated GRs. In a randomized study on multiple GRs, Cardaropoli et al. [29] compared graftless CAF with CAF using an XCM flap and found CRC in 72.00% of sites treated with CMX+CAF and 58.00% of sites treated with CAF alone. Different factors, such as surgical technique, anatomical factors, baseline depth of the gingival recession, and follow-up time points, could influence the percentages of root coverage [24].
The gingival zenith position and interdental papilla height are key aspects of anterior aesthetics. In fact, these gingival parameters interfere with prosthetic, restorative, periodontal, implant, postorthodontic, and esthetic treatment outcomes [33]. Humagain et al. [34] observed differences between genders and sides, which could impact aesthetic results. For both lateral incisors, values significantly differed between males and females. In addition, a significant difference was found for the lateral incisor between the right and the left side. In males, the gingival zenith level of right and left lateral incisors was 0.74 mm and 0.71 mm. In females, the gingival zenith level of right and left lateral incisors was 0.76 mm and 0.72 mm.
As for aesthetics, the participants in this study reported improvement at six months with no significant differences between CTG and XCM groups. Similarly, Nahas et al. [22] reported that both patients and specialists observed improvements in aesthetics after 12 months with no difference between treatment groups. In this study, the highest OHIP-14 scores at baseline (T0) were assigned to the domains of physical pain (4.45), psychological discomfort (3.00), physical limitation (1.82), and psychological limitation (1.45), and at six months, these domains, which could be assumed to derive from DH and aesthetics, reached a score of zero with statistically significant differences (p < 0.05, Table 3), favoring the OHRQoL of the participants since the third postoperative month.
Regarding periodontal parameters, there was no significant difference in PD and CAL gain between the CTG and XCM groups over time. Nahas et al. [22] found no significant differences in PD and CAL gain between the CTG and XCM groups at any point in time (p > 0.05). Both treatments resulted in significant CAL gains at three, six, and 12 months (p < 0.05). As reported by Nahas et al. [22], all participants in this study had low PI and BoP, with no significant differences between groups (CTG and XCM) or follow-up periods (baseline, 3, and 6 months).
In the present study, both treatments provided clinical improvements. Depth of gingival recessions reduced at 6 months (p = 0.000) while KTW increased (0.69 ± 0.80 mm for CTG (p = 0.000) and 0.60 ± 1.30 mm for XCM (p = 0.015)). Moreover, CBCT revealed thicker gingival phenotypes with an increase of 0.69 ± 0.80 mm for CTG (p = 0.000) and 0.60 ± 1.30 mm for XCM (p = 0.041). This scenario demonstrates that the intended goals of both grafts were met. These results are similar to those reported by Aroca et al. [32] in a split-mouth design and a modified tunnel flap. Similarly, for multiple GRs, Cardaropoli et al. [29] reported a mean depth for GR of 0.20 ± 0.34 mm in XCM after 12 months of treatment. Furthermore, a multicenter study by Tonetti et al. demonstrated a mean reduction of 1.70 mm after six months of treatment of multiple GRs with the CAF technique using XCM. In the study by Nahas et al. [22], both procedures resulted in significant increases in KTW at 12 months compared to the baseline. The mean KTW gain was greater in the CTG group (1.2 ± 1.1 mm) than in the XCM group (0.30 ± 0.70 mm). In contrast, Jepsen et al. reported an increase in KTW of 0.93 mm for XCM in the same period. Similarly, a significant increase in KTW (1.34 mm) in the treatment of localized GR was described 12 months after treatment with XCM [26]. These differences in KTW may be due to the use of different methods of assessment, flap design, and follow-up times. In addition to tissue gain, the increase in KTW may be attributed to a tendency for the mucogingival junction to return to its original genetically determined position, which is seen after one year of postoperative follow-up [27].
Our study has some limitations. The 6-month follow-up time and the possible contamination or spilling of the effects from one intervention to another (“carry-cross” effects of the split-mouth design) can influence treatment outcomes. It should be stressed that the test and control sites were in diametrically opposite quadrants, which should minimize this effect. Moreover, split-mouth design also has the advantage of reducing interindividual variability in the estimated treatment effect and potentially requires fewer subjects than a parallel group trial with the same power.
Considering that most information is derived from single GR studies, data from the present study could be supportive of the clinical decision-making process. Further studies with larger samples and longer follow-up periods are needed. Thus, XCM was shown to be as effective as CTG and provided the added benefit of causing less postoperative pain and discomfort. Therefore, some clinically relevant conclusions can be drawn, and these results can serve as a basis for future studies (Fig. 6).
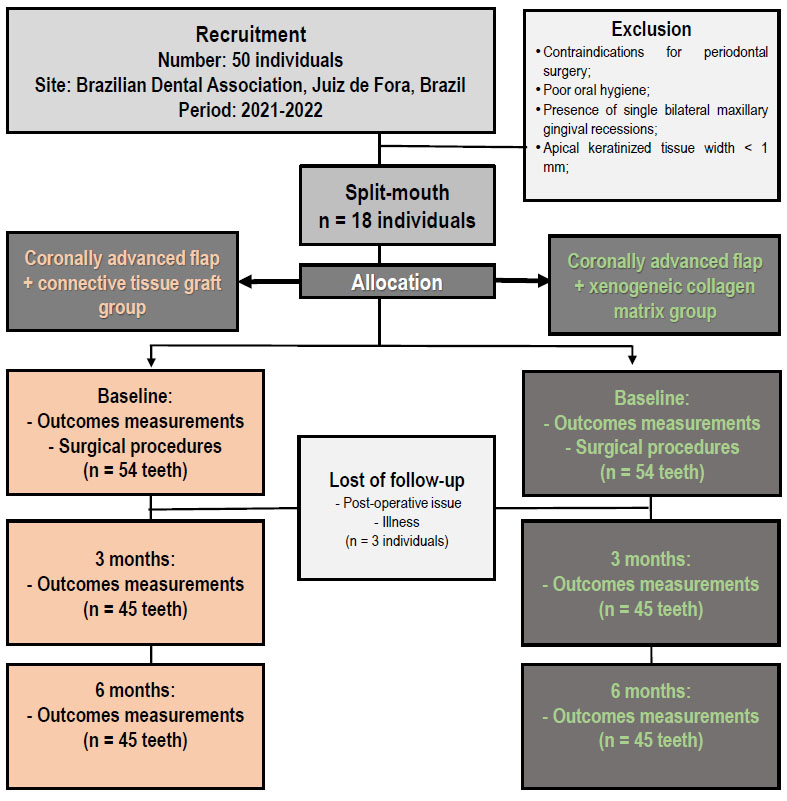
Consort diagram flow.
CONCLUSION
Significant improvements were found in the gingival phenotype revealed by the thicker gingival phenotype 6 months after treatment. These improvements were observed for both treatment groups.
Both surgical treatments provided similar and adequate root recovery, especially considering how challenging multiple gingival recessions are in daily dental practice.
Quality of life related to oral health improved over time with more discrete results regarding dentin hyper- sensitivity. Only the XCM group experienced a reduction in dentin hypersensitivity.
CLINICAL SIGNIFICANCE
Multiple gingival recessions are treatable conditions in dental daily practice. Patients could benefit from xenogeneic collagen matrix since it was found to be as effective as connective tissue grafting; however, it causes less postoperative pain and discomfort and reduces dentin hypersensitivity.
After the treatment, a better Oral Health-Related Quality of Life (OHRQoL) can be achieved.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| OHRQoL | = Oral Health-Related Quality of Life |
| GR | = Gingival Recessions |
| RT2 | = Recession Type 2 |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This longitudinal split-mouth clinical study was reviewed and approved by the Institutional Research Ethics Committee (Approval No. 4.592.151), University of Taubaté Ethics Research Committee, Brazil.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in the University of Taubaté repository of theses at (http://repositorio.unitau.br/), reference number (http://repositorio.unitau.br/jspui/handle/20.500.11874/6848).
ACKNOWLEDGEMENTS
Declared none.


