All published articles of this journal are available on ScienceDirect.
Enhancing Communication in Dental Clinics through Understanding Oral Medicine Terminology
Abstract
Introduction
A clear communication between healthcare providers and patients is crucial. However, challenges arise due to medical jargon, particularly for non-native English speakers, potentially affecting patient outcomes. This study assessed patients' understanding of oral medicine terms to improve clarity in patient-dentist interactions, decision-making, and overall patient well-being.
Methods
A self-administered cross-sectional survey was conducted between November 2022 and June 2023, targeting adult patients visiting dental clinics at King Abdulaziz University. Participants completed an 11-term questionnaire to evaluate their understanding of commonly used medical terminology in oral medicine.
Results
A total of 286 participants were included, 66.4% men, with a mean age of 43.4 years and 82.9% having a university education. In understanding oral medicine terminologies, for terms such as “tumor,” 70.3% understood it as a mass that could be cancerous, while 88.1% correctly defined “cancer.” Diagnostic terms such as “biopsy” were correctly identified by 56.3% of participants. Men demonstrated a higher average score (7.88±2.27) than men (6.16±3.00, P < 0.001). Age groups showed varied understanding, but there was no statistically significant difference in the overall knowledge score. Participants with a scientific background had a notably higher overall knowledge score (8.01±2.75) compared to those without (6.23±2.79, P < 0.001) it.
Conclusion
This study revealed inadequacies in dental clinic patients' grasp of translated oral medicine terms, particularly among non-native English speakers. Higher knowledge ratings among women and those with a scientific background highlight the value of face-to-face questionnaires that enable the interviewer to clarify and follow up on specific topics as needed. Thus, it enhances patient-dentist interactions in dental treatment.
1. INTRODUCTION
Clear and proper communication between healthcare providers and patients is crucial for a successful clinical practice. However, this process requires significant effort and mutual understanding [1]. Medical education has its own dictionary that can further encrypt patient health information. The gap between dentists and their patients' literacy must be connected to patient health and safety to ensure effective communication and understanding. Poor health outcomes and inefficient use of health resources are closely associated with poor health literacy [2, 3]. Since medical terminologies currently used are mostly in English, patients with non-English mother tongues may encounter difficulties understanding these terms [4]. Even those non-native speakers with solid conversational English may lack knowledge of Latin-originated medical or dental terminology [5, 6]. Furthermore, in several parts of the world, healthcare studies are offered exclusively in English, with no effort to familiarize future healthcare providers with their terminology counterparts in the native languages of their local communities [7].
In clinical practice, most medical terminology translations are based on the personal efforts of healthcare providers, which might not be of high accuracy or might not be clearly and precisely perceived by patients [8]. This poses a significant barrier when communicating with non-English-speaking patients and compromises the certainty of accurate knowledge of their diagnosis, thus affecting the treatment plan for these patients [3].
Oral medicine is a specialty in dentistry dedicated to diagnosing and treating oral mucosal lesions, salivary gland dysfunction, and orofacial pain, as well as detecting oral malignant and potentially malignant disorders. The lack of familiarity with oral medicine terminologies from the patient's perspective and the treating clinicians' unawareness regarding this lack of understanding may result in adverse outcomes. These include over or underestimated concerns, lack of patient compliance, poor patient decision-making, poor prognosis, and lower quality of life [4].
Oral medicine providers are responsible for clarifying the medical terminologies commonly used in their practice to their patients and ensuring their complete understanding [8]. This study aimed to measure patients' accuracy in understanding commonly used terminologies in oral medicine that have been professionally translated from English to Arabic (i.e., anatomical structures, clinical investigations, and clinical diagnoses). The secondary aim of this investigation was to explore the possible factors that may influence patients' understanding of these medical terminologies (i.e., age, sex, and scientific background).
2. METHODS
2.1. Study Design and Sampling
This cross-sectional survey targeted adult patients treated at King Abdulaziz University (KAU) dental clinics using a convenience sampling method. Google Forms was used to create the self-administered questionnaire. The questionnaire was sent to the targeted population through WhatsApp Messenger in the waiting area of dental clinics at KAU between November 2022 and June 2023. General dentists were assigned to manage the process of sending forms to patients, and the forms were limited to one response. The sample size was calculated using G*Power software (version 3.1.7.9). Based on the results of a previous study [5] with a power of 80%, 0.05 alpha, and 0.2 beta, the calculated sample size was 76.
2.2. Ethical Considerations and Participants Consenting
The Research Ethics Committee examined and approved this study for adherence to the Declaration of Helsinki [9] (ethical approval number: #138-120-22) which conformed to the STROBE checklist. Before the questionnaire was administered, all potential participants were provided with a cover letter describing the study's goals and ensuring the confidentiality of their responses. The participants were informed that their participation was entirely voluntary and that they could withdraw anytime. Before completing the questionnaire, each participant provided written informed consent.
2.3. Inclusion and Exclusion Criteria of the Study
Inclusion criteria included a willingness to participate in the questionnaire voluntarily and signing a consent form before starting. All included patients were 18 years old and above and could read and understand either Arabic or English with no restriction on their educational level. Individuals who participated in the face and content validity tests were excluded from the analysis. Dental students and faculty members were excluded from this study.
2.4. Study Tools and Data Collection
The questionnaire comprised 17 questions, most of which were multiple-choice. Additionally, participants could provide written elaboration if none of the provided choices suited their opinion for each question. The questionnaire consisted of two sections: 1) demographic and background data (i.e., age, sex, education level, scientific background, Arabic proficiency) and 2) medical terminology (meaning of tumors, ulcer, vesicle, biopsy, swab, culture, and temporomandibular joint [TMJ]). This questionnaire was modified and adapted for relevance to our study [1]. The questionnaire, in both English and Arabic, is available upon request from the authors.
2.5. Forward and Backward Translation Validity
The questionnaire was constructed in English and incorporated common medical terminology in oral medicine, surgery, and pathology practices. A systematic process was used to translate the original English questionnaire into Arabic. This process was initiated by assigning three translators native to Arabic who were highly proficient in English and one bilingual translator (native to English and Arabic). Everyone produced a written translated version, after which all translators met to discuss the translation and produced a final version [10].
A backward translation (Arabic to English) was performed to confirm the accuracy and quality of the translated English version. The process was completed by two double-blinded translators from the original English questionnaire version and assigned to translate the final Arabic questionnaire into English to confirm its consistency with the original version of the English questionnaire [10]. An expert committee comprising a methodologist, oral medicine professionals, and language professionals reviewed various versions of the questionnaires, and a definite pre-final version was produced for face and content validity testing.
2.6. Face Validity and Content Validity Testing
Two patients attending the KAU clinics with no scientific background were chosen to participate in the survey to assess the questionnaire's face validity before its distribution. The two patients also provided feedback on the survey's clarity, and all comments were considered. Based on their feedback, the questionnaire was revised by two experts in the field to improve its validity.
2.7. Statistical Analysis
Data were automatically transferred from Google survey forms to a password-protected digital online Excel spreadsheet. Descriptive statistics (i.e., means and standard deviations for continuous variables and measures of frequency for categorical variables) were calculated for each question. Comparisons based on sex, age, and scientific background were conducted using the chi-squared test. An independent t-test was conducted to evaluate the difference between the studied groups (men and women, <50 years and ≥50 years, and participants with or without a scientific background) regarding the overall knowledge score. P-values under 0.05 were regarded as statistically significant. SAS version 9.4 and SPSS version 22 were used for the analysis.
2.8. Patient or Public Contributions
In this study, the role and input of the patients who participated in the survey, including their influence on the research findings, are referred to as patient contributions. The patient's contribution to this situation consists of participation in surveys, providing responses and demographic information, and influencing study outcomes. In general, the involvement of patients in this research is essential to meet the study's objectives, which include evaluating patients' understanding of oral medicine terminology and ultimately enhancing patient-provider communication in dental care environments.
3. RESULTS
3.1. Participants Characteristics and Background
A total of 286 participants were included, with a mean age of 43.4 ± 15.4 years. Men accounted for 66.4% of the participants, and women accounted for 33.6%. Approximately 63.3% of the participants had a scientific background. Regarding educational attainment, a substantial percentage of the participants had a university-level education (82.9%), 15% had completed secondary school (15%), and 2.1% had finished primary school. Regarding linguistic proficiency in Arabic, 97.6% of participants indicated that Arabic was their first language. The demographic data and characteristics of the study participants are summarized in Table 1.
3.2. Medical Terminology
3.2.1. Type of Lesions: Tumor, Malignant, Benign Tumor, Cancer, Ulcer, and Vesicle
For the term “tumor,” 70.3% perceived it as a mass that could either be cancerous or not, 13.3% believed it to be cancer, 8.7% associated it with swelling, 0.3% described it as unrestricted growth yet to be classified, and 7.3% were unsure of the definition. For “malignant tumor,” 2.4% believed it could be cancerous, 81.1% identified it as a cancerous tumor, 11.9% as uncertain, and 4.5% considered it non-cancerous. Regarding “benign tumor,” 7.7% thought it might or might not be cancerous, 6.6% perceived it as cancerous, 74.1% identified it as non-cancerous, and 11.5% were unsure of its definition. Finally, for “cancer,” 88.1% defined it as a disease that can spread to other body organs, 5.6% believed it to be an untreatable disease, 4.5% were uncertain, and 1.7% thought of it as an infectious disease. Regarding “ulcer,” 11.2% described it as a cyst full of fluids; 8% considered it a tender, soft mass; 55.6% described it as tissue with a scrapped surface; and 25.2% were unsure. For “vesicle,” 46.2% believed it to be a cyst full of fluids, 10.1% thought it was a tender, soft mass, 5.6% described it as a tissue with a scrapped surface, 37.4% admitted they did not know, and 0.3% had other descriptions, as shown in Fig. (1).
| Variables | Frequency | Percent | |
|---|---|---|---|
| Age (Mean± SD) | 43.4 ± 15.4 | ||
| Gender | Male | 190 | 66.4% |
| Female | 96 | 33.6% | |
| Scientific background | Yes | 181 | 63.3% |
| No | 105 | 36.7% | |
| Highest level of education | Primary School | 6 | 2.1% |
| Secondary School | 43 | 15% | |
| University education | 237 | 82.9% | |
| Arabic as the first language | Yes, Arabic is my first language | 279 | 97.6% |
| No, but I am proficient in Arabic and can speak it fluently | 4 | 1.4% | |
| No, but I can speak, read, and understand Arabic easily | 1 | 0.3% | |
| No, but I can slightly speak and understand Arabic | 2 | 0.7% | |
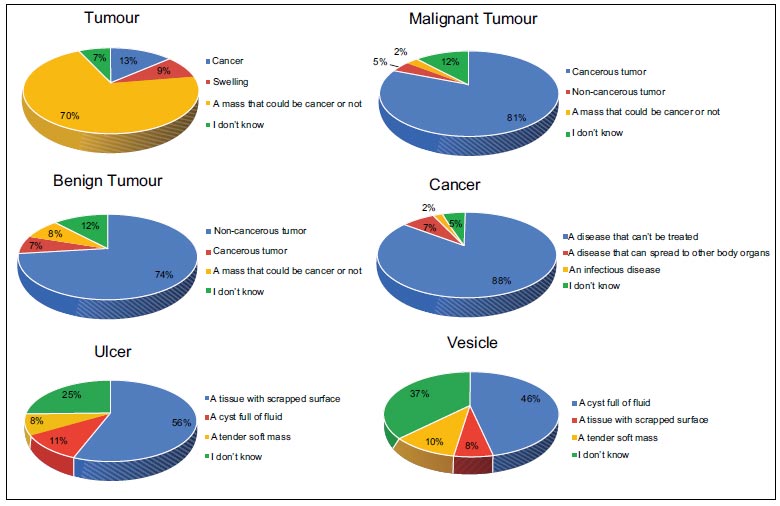
Pie charts showing percentages of answers of different types of lesions.
3.2.2. Diagnostic Modalities: Biopsy, Sample Culture, and Swab
Regarding “biopsy,” 56.3% correctly defined it as a deep sample taken by cutting tissue, 9.1% believed it is a superficial sample taken by scraping the tissue surface, 15% thought it was a superficial sample taken from the body and cultured outside of it, and 19.6% were uncertain. For “sample culture,” 6.3% associated it with a deep sample taken by cutting tissue, and 14.3% believed it was a superficial sample taken by scraping the tissue surface. Furthermore, 54.5% rightly associated it with a superficial sample taken from the body and cultured outside it. A total of 24.1% did not know, and 0.6% had other definitions. Concerning the “swab,” 4.9% thought it to be a deep sample taken by cutting tissue, and 57.7% correctly identified it as a superficial sample taken by scraping the tissue surface. Moreover, 19.9% believed it to be a superficial sample taken from the body and cultured outside of it, and 17.5% were unsure, as shown in Fig. (2).
3.2.3. Anatomical Structures: Lymph Nodes and Temporomandibular Joint
Regarding the term “lymph nodes,” 5.6% perceived them as cancerous masses and 48.3% identified them as glands that eliminate body toxins. Additionally, 17.1% thought they were glands that secrete saliva, and 29% were unsure. Finally, for “TMJ,” 8.7% believed it is a joint connecting the jaw with the ear, and 1.7% thought it connects the jaw with the neck. Furthermore, 44.8% rightly perceived it as a joint connecting the lower jaw with the upper jaw, and another 44.8% admitted they did not know, as shown in Fig. (3).
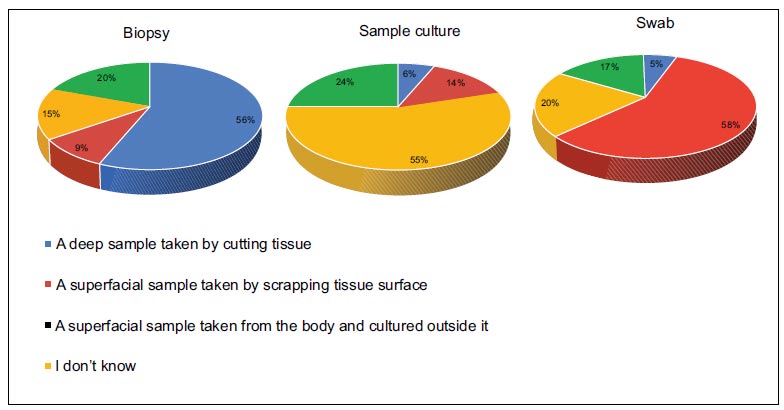
Pie charts showing percentages of diagnostic modalities terminologies.
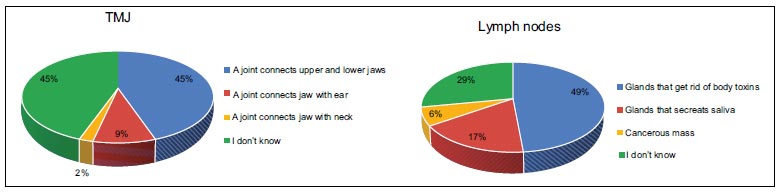
Pie charts showing percentages of anatomical structures terminologies.
3.3. Influence of Demographic Data on Understanding Terminologies Utilized in the Oral Medicine Clinics
3.3.1. Sex
Women demonstrated a significantly higher percentage of correct answers than men for the terms “malignant tumor” (93.8% vs. 74.2%, P < 0.001), “benign tumor” (85.4% vs. 68.4%, P < 0.001), “lymph nodes” (68.8% vs. 36.8%, P < 0.001), “ulcer” (62.5% vs. 51.6%, P = 0.013), “Vesicle” (54.2% vs. 42.6%, P < 0.001), “biopsy” (69.8% vs. 48.9%, P < 0.001), “sample culture” (63.5% vs. 50.0%, P = 0.011), “swab” (65.6% vs. 53.2%, P = 0.005), and “TMJ” (60.4% vs. 36.3%, P < 0.001). Additionally, the overall knowledge score was higher for women (7.88±2.27) compared to men (6.16±3.00, P < 0.001). Other terms, such as “tumor” and “cancer,” did not show statistically significant differences in correct responses between sexes, as shown in Table 2.
3.3.2. Age
Participants aged 50 years and older had a significantly higher percentage of correct answers for the term “ulcer” compared to those under 50 years old (63.6% vs. 48.0%, P = 0.015). Similarly, the older age group showed a greater accuracy for “vesicle” (53.5% vs. 40.1%, P = 0.004) and “sample culture” (62.8% vs. 46.7%, P = 0.013). In contrast, individuals below 50 years exhibited superior knowledge of “biopsy,” with 62.5% answering correctly as opposed to 50.4% in the older group (P = 0.004). Other terms, including “tumor,” “malignant tumor,” “benign tumor,” “cancer,” “lymph nodes,” “swab,” and “TMJ,” and the overall knowledge score did not display statistically significant differences between the two age groups, as shown in Table 3.
| Terms | Male | Female | P-value | |
|---|---|---|---|---|
| Tumour | Correct | 130 (68.4%) | 71 (74.0%) | 0.053 |
| Incorrect | 41 (21.6%) | 23 (24.0%) | ||
| I don't know | 19 (10%) | 2 (2.1%) | ||
| Malignant tumour | Correct | 141 (74.2%) | 90 (93.8%) | <0.001 |
| Incorrect | 22 (11.6%) | 3 (3.1%) | ||
| I don't know | 27 (14.2%) | 3 (3.1%) | ||
| Benign tumour | Correct | 130 (68.4%) | 82 (85.4%) | <0.001 |
| Incorrect | 29 (15.3%) | 12 (12.5%) | ||
| I don't know | 31 (16.3%) | 2 (2.1%) | ||
| Cancer | Correct | 163 (85.8%) | 86 (89.6%) | 0.362 |
| Incorrect | 16 (8.4%) | 8 (8.3%) | ||
| I don't know | 11 (5.8%) | 2 (2.1%) | ||
| Lymph nodes | Correct | 70 (36.8%) | 66 (68.8%) | <0.001 |
| Incorrect | 51 (26.8%) | 17 (17.7%) | ||
| I don't know | 69 (36.3%) | 13 (13.5%) | ||
| Ulcer | Correct | 98 (51.6%) | 60 (62.5%) | 0.013 |
| Incorrect | 34 (17.9%) | 22 (22.9%) | ||
| I don't know | 58 (30.5%) | 14 (14.6%) | ||
| Vesicle | Correct | 81 (42.6%) | 52 (54.2%) | <0.001 |
| Incorrect | 21 (11.1%) | 24 (25.0%) | ||
| I don't know | 88 (46.3%) | 20 (20.8%) | ||
| Biopsy | Correct | 93 (48.9%) | 67 (69.8%) | <0.001 |
| Incorrect | 46 (24.2%) | 24 (25.0%) | ||
| I don't know | 51 (26.8%) | 5 (5.2%) | ||
| Sample culture | Correct | 95 (50.0%) | 61 (63.5%) | 0.011 |
| Incorrect | 39 (20.5%) | 22 (22.9%) | ||
| I don't know | 56 (29.5%) | 13 (13.5%) | ||
| Swab | Correct | 101 (53.2%) | 63 (65.6%) | 0.005 |
| Incorrect | 46 (24.2%) | 26 (27.1%) | ||
| I don't know | 43 (22.6%) | 7 (7.3%) | ||
| Temporomandibular joint | Correct | 69 (36.3%) | 58 (60.4%) | <0.001 |
| Incorrect | 18 (9.5%) | 13 (13.5%) | ||
| I don't know | 103 (54.2%) | 25 (26.0%) | ||
| Overall knowledge score | 6.16±3.00 | 7.88±2.27 | <0.001 | |
| Terms | <50 years | ≥50 years | P-value | |
|---|---|---|---|---|
| Tumour | Correct | 110 (72.4%) | 89 (69.0%) | 0.545 |
| Incorrect | 34 (22.4%) | 29 (22.5%) | ||
| I don't know | 8 (5.3%) | 11 (8.5%) | ||
| Malignant tumour | Correct | 125 (82.2%) | 102 (79.1%) | 0.769 |
| Incorrect | 12 (7.9%) | 13 (10.1%) | ||
| I don't know | 15 (9.9%) | 14 (10.9%) | ||
| Benign tumour | Correct | 116 (76.3%) | 93 (72.1%) | 0.459 |
| Incorrect | 22 (14.5%) | 18 (14.0%) | ||
| I don't know | 14 (9.2%) | 18 (14.0%) | ||
| Cancer | Correct | 136 (89.5%) | 110 (85.3%) | 0.457 |
| Incorrect | 11 (7.2%) | 11 (8.5%) | ||
| I don't know | 5 (3.3%) | 8 (6.2%) | ||
| Lymph nodes | Correct | 78 (51.3%) | 57 (44.2%) | 0.246 |
| Incorrect | 38 (25.0%) | 30 (23.3%) | ||
| I don't know | 36 (23.7%) | 42 (32.6%) | ||
| Ulcer | Correct | 73 (48.0%) | 82 (63.6%) | 0.015 |
| Incorrect | 38 (25.0%) | 17 (13.2%) | ||
| I don't know | 41 (27.0%) | 30 (23.3%) | ||
| Vesicle | Correct | 61 (40.1%) | 69 (53.5%) | 0.004 |
| Incorrect | 34 (22.4%) | 11 (8.5%) | ||
| I don't know | 57 (37.5%) | 49 (38.0%) | ||
| Biopsy | Correct | 95 (62.5%) | 65 (50.4%) | 0.004 |
| Incorrect | 24 (15.8%) | 42 (32.6%) | ||
| I don't know | 33 (21.7%) | 22 (17.1%) | ||
| Sample culture | Correct | 71 (46.7%) | 81 (62.8%) | 0.013 |
| Incorrect | 35 (23.0%) | 26 (20.2%) | ||
| I don't know | 46 (30.3%) | 22 (17.1%) | ||
| Swab | Correct | 88 (57.9%) | 74 (57.4%) | 0.610 |
| Incorrect | 35 (23.0%) | 35 (27.1%) | ||
| I don't know | 29 (19.1%) | 20 (15.5%) | ||
| Temporomandibular Joint | Correct | 64 (42.1%) | 61 (47.3%) | 0.503 |
| Incorrect | 15 (9.9%) | 15 (11.6%) | ||
| I don't know | 73 (48.0%) | 53 (41.1%) | ||
| Overall knowledge score | 6.69±2.79 | 6.84±2.98 | 0.655 | |
3.4. Influence of Scientific Backgrounds on Understanding Terminologies Utilized in the Oral Medicine Clinics
Participants with a scientific background had higher accuracy in identifying “malignant tumor” than those without (88.9% vs. 77.6%, P = 0.041). Similarly, for the term “lymph nodes,” those with a scientific background demonstrated superior knowledge (65.4% vs. 40.5%, P < 0.001). Other terms where the scientific background group outperformed included “ulcer” (67.9% vs. 50.2%, P = 0.009), “vesicle” (66.7% vs. 38.5%, P < 0.001), “biopsy” (70.4% vs. 50.2%, P < 0.001), “sample culture” (69.1% vs. 48.8%, P < 0.001), and “TMJ” (63.0% vs. 37.1%, P < 0.001). The overall knowledge score was also significantly higher for participants with a scientific background (8.01±2.75) than those without (6.23±2.79, P < 0.001). Other terms, such as “tumor,” “benign tumor,” “cancer,” and “swab,” did not present statistically significant differences between the two groups, as shown in Table 4.
| Terms | No Scientific Background | Scientific Background | P-value | |
|---|---|---|---|---|
| Tumour | Correct | 142 (69.3%) | 59 (72.8%) | 0.813 |
| Incorrect | 47 (22.9%) | 17 (21.0%) | ||
| I don't know | 16 (7.8%) | 5 (6.2%) | ||
| Malignant tumour | Correct | 159 (77.6%) | 72 (88.9%) | 0.041 |
| Incorrect | 23 (11.2%) | 2 (2.5%) | ||
| I don't know | 23 (11.2%) | 7 (8.6%) | ||
| Benign tumour | Correct | 145 (70.7%) | 67 (82.7%) | 0.075 |
| Incorrect | 35 (17.1%) | 6 (7.4%) | ||
| I don't know | 25 (12.2%) | 8 (9.9%) | ||
| Cancer | Correct | 137 (84.4%) | 76 (93.8%) | 0.085 |
| Incorrect | 20 (9.8%) | 4 (4.9%) | ||
| I don't know | 12 (5.9%) | 1 (1.2%) | ||
| Lymph nodes | Correct | 83 (40.5%) | 53 (65.4%) | <0.001 |
| Incorrect | 53 (25.9%) | 15 (18.5%) | ||
| I don't know | 69 (33.7%) | 13 (16.0%) | ||
| Ulcer | Correct | 103 (50.2%) | 55 (67.9%) | 0.009 |
| Incorrect | 41 (20.0%) | 15 (18.5%) | ||
| I don't know | 61 (29.8%) | 11 (13.6%) | ||
| Vesicle | Correct | 79 (38.5%) | 54 (66.7%) | <0.001 |
| Incorrect | 34 (16.6%) | 11 (13.6%) | ||
| I don't know | 92 (44.9%) | 16 (19.8%) | ||
| Biopsy | Correct | 103 (50.2%) | 57 (70.4%) | <0.001 |
| Incorrect | 51 (24.9%) | 19 (23.5%) | ||
| I don't know | 51 (24.9%) | 5 (6.2%) | ||
| Sample culture | Correct | 100 (48.8%) | 56 (69.1%) | <0.001 |
| Incorrect | 42 (20.5%) | 19 (23.5%) | ||
| I don't know | 63 (30.7%) | 6 (7.4%) | ||
| Swab | Correct | 115 (56.1%) | 49 (60.5%) | 0.354 |
| Incorrect | 50 (24.4%) | 22 (27.2%) | ||
| I don't know | 40 (19.5%) | 10 (12.3%) | ||
| Temporomandibular Joint | Correct | 76 (37.1%) | 51 (63.0%) | <0.001 |
| Incorrect | 23 (11.2%) | 8 (9.9%) | ||
| I don't know | 106 (51.7%) | 22 (27.2%) | ||
| Overall knowledge score | 6.23±2.79 | 8.01±2.75 | <0.001 | |
4. DISCUSSION
4.1. Medical Terminology
Understanding medical terminology is significant because it enables people to actively control their dental health and produce better results [11]. However, studies have shown that, even in highly specialized medical settings, patient knowledge levels are frequently lower than anticipated [12]. No prior research has considered how people comprehend the language used in oral medicine. However, this practice is widely used in primary and secondary care dentistry [11].
Our findings indicate variable comprehension of medical terms related to lesions. A significant 70.3% of participants correctly understood that a “tumor” could be either cancerous or benign, aligning with a prior outpatient study where 65% displayed similar knowledge [1]. Conversely, another study found that only 20% of patients understood this [5]. The high percentage of correct answers could be because most participants had a university-level education. Another explanation could be that our survey was sent through WhatsApp while waiting. Therefore, patients might have used an Internet search to answer [13]. Approximately 81% of our survey participants correctly defined “malignant” as a cancerous tumor, which is higher than the 65% found in a breast clinic environment [12] but closer to Hayes et al.'s findings of 70% [1]. The terms “ulcer” and “vesicle” showed that over half of the participants were familiar with their definitions, although Hayes et al. reported a higher 91% accuracy for the vesicle definition [1]. The terms “vesicle” and “ulcer” might be more commonly understood by the general population due to their broader application across multiple medical specialties and their frequent occurrence in daily life. For instance, conditions like cold sores or skin blisters are vesicles. Peptic ulcers or mouth ulcers are regularly encountered or discussed, making these terms more relatable and familiar to many individuals than specialized terms like “cancer” or “tumor.”
When it comes to diagnostic procedures, our study had a higher number of respondents who correctly described the term “biopsy,” in contrast with the 29% and 12% reported in 2 other studies [1, 5], respectively. Similar results were shown with both terms “sample culture” and “swab” attributed to the frequent media coverage and public discussions surrounding coronavirus disease 2019 testing methods, where swabbing became a commonplace term [14].
Focusing on anatomical structures, for the term “lymph nodes,” only 47.6% provided the correct definition. This contrasts with Hamilton's study, in which a mere 23% defined the lymph node as part of the lymphatic system, and the majority remained uninformed [5]. These conflicting results could be attributed to several factors, including different study populations, settings, and educational systems. When participants were queried about “TMJ,” our results were consistent with findings from another study where approximately 50% of participants displayed comparable knowledge [15].
Uncovering the level of understanding of these medical terminologies will provide a better assessment of the clarity of information that oral medicine providers convey to their patients. It will also help discover areas that require further efforts from oral medicine providers to educate their patients and enhance patient-dentist communication and mutual understanding, leading to better decision-making, a stress-free environment, and a higher quality of life.
4.2. Knowledge Gaps between Participants
Gender disparities in the comprehension of medical terminology were evident, with women consistently demonstrating a superior grasp over a range of terms compared to men. This difference may allude to factors such as educational background, exposure to healthcare environments, and sex-specific communication patterns. Women's superior performance in recognizing terms like “malignant tumor,” “benign tumor,” and “lymph nodes,” among others, may suggest that they are more actively engaged in health discussions or have more frequent encounters with healthcare systems. However, it is intriguing that terms such as “tumor” and “cancer” did not display the same-sex bias, possibly indicating that these terms are so commonly used in public discourse that gender disparities are minimized. The distinct overall knowledge score further emphasizes the potential differences in health literacy between genders. Recognizing these disparities is crucial for healthcare providers to effectively tailor patient education and communication strategies.
Age appears to play a pivotal role in the comprehension of medical terminology. Participants aged 50 and above displayed a more refined understanding of terms such as “ulcer,” “vesicle,” and “sample culture” compared to their younger counterparts. This could be attributed to their potentially increased interactions with healthcare settings or generational differences in the emphasis on specific medical conditions [16]. Conversely, the younger demographic's superior grasp of “biopsy” might suggest more recent exposure to this terminology or differences in health information access across generations. Various terms, including “tumor,” “malignant tumor,” and others, including the overall knowledge score, transcended age differences, pointing to a uniform understanding or shared cultural exposure to these concepts across generations. This highlights the need for age-tailored health education approaches to ensure that all age groups maintain comprehensive medical literacy.
The scientific background appears to significantly influence proficiency in understanding specific medical terminology. Participants with a scientific background showcased a marked advantage in correctly identifying terms like “malignant tumor,” “lymph nodes,” “ulcer,” “vesicle,” “biopsy,” “sample culture,” and “TMJ.” This pronounced difference might stem from their formal education, exposure to scientific literature, or more frequent interactions with healthcare settings and professionals [17]. The tangible edge in the overall knowledge score further emphasized the impact of having a scientific foundation on medical literacy. Nonetheless, terms such as “tumor,” “benign tumor,” “cancer,” and “swab” seem to be universally understood, hinting that they might be embedded more deeply in common discourse, irrespective of one's academic orientation. This insight emphasizes the role of educational exposure in shaping health and the importance of targeted health communication in various demographic groups. Patient perceptions and interpretations of medical knowledge may be influenced by their personal experiences, cultural beliefs, and individual values. Healthcare professionals must be aware and respectful of diverse viewpoints, focusing on communication and educational efforts regarding the unique requirements of each patient [17, 18]. Regardless of the patient's scientific background, healthcare personnel must communicate with patients clearly to ensure their accurate understanding [19]. Awareness of oral medicine, including terminology, should not be limited to the general population. Medical students and practitioners should also know targets to improve their significant lack of knowledge [20].
5. LIMITATIONS
This study has several limitations. Voluntary participation in the survey may limit the number of respondents and may not fully represent the studied community. Moreover, although this survey was directed at all adult patients seen in dental clinics in KAU, it would be more critical if more participants were included (western province) since Jeddah is the geographic source of this investigation. Finally, the subjectivity of responses and the possibility of guessing answers were expected, and inevitable limitations that might compromise the reliability of the provided answers could be minimized if face-to-face interviews were conducted.
CONCLUSION
In conclusion, there are wide variations in people's understanding of medical terminology, depending on their age, sex, and level of education. While most patients understand certain concepts, others exhibit differences in recognition. Specific medical terms are typically more straightforward for women, older adults, and individuals with scientific backgrounds. However, it is essential to acknowledge that some patients have a deep understanding of their medical circumstances, regardless of their background. This study emphasized how crucial it is for medical staff to communicate clearly and individually with each patient. Furthermore, it underscored their particular needs to ensure every patient can access and understand medical information.
AUTHORS' CONTRIBUTIONS
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
ABBREVIATION
| KAU | = King Abdulaziz University |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Ethics Committee at King Abdulaziz University Faculty of Dentistry (ethical approval number: #138-120-22).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.


