All published articles of this journal are available on ScienceDirect.
Lateral Antrostomy Integrated with Digital Approach (LAIDA): A Case Report and Literature Review
Abstract
Background
Traditionally, surgeons rely on manual measurements to translate pre-surgical plans into clinical reality during sinus floor elevation with a lateral approach. Standardizing this surgical phase could offer a reproducible technique minimizing operational errors and ensuring more consistent and predictable outcomes.
Objective
This case report presents a comprehensive digital approach integrating lateral antrostomy (LAIDA) for the elevation of the maxillary sinus floor.
Case Presentation
Lateral sinus floor elevation was required for a 61-year-old patient. A detailed digital protocol, integrating artificial intelligence, was employed to create a tooth-supported surgical guide for antrostomy. Under local anaesthesia, a full-thickness flap was elevated to expose the lateral sinus wall. The surgical guide was accurately positioned, and the antrostomy area was marked on the bone wall. The bony window was then performed using round diamond burs, and the Schneiderian membrane was gently lifted until the medial wall of the sinus was exposed. The sub-antral space was filled with a composite graft, and three implants were placed using the same surgical guide. The antrostomy was covered using a resorbable collagen membrane, and flaps were sutured with synthetic monofilament. No intra- and post-operative complications were recorded.
Conclusion
Accurate antrostomy planning and execution are crucial, considering factors, like sinus floor location, presence of alveolar-antral artery, and Underwood septa. The present study emphasizes the benefits of a standardized approach using a 3D-printed surgical guide, aiding real-time visualization of the predetermined bony window during surgery. The LAIDA workflow may help in minimizing intra-operative complications, enhancing patient comfort and improving surgical outcomes.
1. INTRODUCTION
Sinus floor elevation represents a reliable surgical approach to regenerate new bone and allow implant-supported rehabilitation of the atrophic posterior maxilla. Specifically, two main techniques have been described in the literature, i.e., lateral and transcrestal approaches, both with different and specific indications [1]. The lateral approach was first described by Boyne in 1980 and modified by Tatum in 1986 [2, 3]. This technique consists of an antrostomy performed on the lateral maxillary wall, followed by the detachment of the Schneiderian membrane from the bony walls and the filling of the sub-antral space with grafting material to facilitate new bone formation [4]. This technique has been slightly modified in the last few years in a more conservative way [5-7].
The correct implementation of the antrostomy, in the right position and with adequate shape and dimension, is a crucial step to ensure successful Schneiderian membrane elevation, minimizing the perforation risk during its detachment from the bone. It is mandatory to conduct a thorough pre-operative assessment using three-dimensional radiographs, such as CBCT (Cone Beam Computed Tomography), to evaluate the anatomy of the maxillary sinus, the amount of residual bone, and the precise location of important structures, like sinus floor, alveolar-antral artery (anastomosis between posterior superior alveolar artery and infraorbital artery) [8], Underwood septa (if present), and adjacent teeth. An accurate assessment of their exact position allows safer positioning of the bony window, reducing the incidence of intra-operative complications. Pre-surgical planning should program the lower border of the antrostomy placed at safety distance from the sinus floor to prevent damage to the Schneiderian membrane, which lines the sinus cavity. A distance of 2-3 mm is often recommended in literature as a safety margin [9-13]. Then, the lateral window should have adequate size to allow access for proper visualization and instrument manipulation, while avoiding excessive bone removal, as previous studies have shown that graft maturation and consolidation may be compromised when the dimensions of the lateral window are too large [14, 15].
Traditionally, surgeons rely on intuitive methods to transfer pre-surgical projects into clinical reality during this intervention, using mental navigation and manual measurements, to find the correct position of the antrostomy. The standardization of this surgical phase may represent an important improvement in sinus floor elevation with a lateral approach. A reproducible technique is inherently less susceptible to operational errors and facilitates a quicker learning process. Furthermore, a clearly defined method is more consistent in its execution, thus yielding more predictable outcomes. From this perspective, it is extremely important to be able to accurately transfer the pre-surgical planning information to the clinical reality in a simple and predictable manner.
Three-dimensional templates have been widely used for several years in oral implantology to aid in computer-guided implant placement. Based on the same principle, a surgical cutting guide for lateral sinus antrostomy was first proposed by Mandelaris and Rosenfeld in 2008 [16]. Subsequently, other studies have been published suggesting the use of resin templates with slight modifications to address both the position and shape of the antrostomy.
The objective of the present study was to outline a detailed protocol for the surgical technique, informed by an extensive review of the existing literature on the topic. This protocol was designed to be an integral component of a comprehensive digital approach, incorporating artificial intelligence, for the implant-prosthetic rehabilitation of the atrophic posterior maxilla.
2. CASE PRESENTATION
A 61-year-old male patient, in good general health, presented to our observation asking for a fixed rehabilitation of a maxillary Kennedy class II edentulism. CBCT, performed using a radiographic guide incor- porating the virtual diagnostic waxing, revealed an advanced bone atrophy in the upper right maxilla. Following a thorough radiographic, clinical, and occlusal examination, and after discussing with the patient the possible therapeutic alternatives, maxillary sinus floor elevation with the simultaneous insertion of three dental implants was planned. The presence of a wide sinus cavity (bucco-palatal distance at 10 mm height ranging from 13.8 mm and 23.2 mm at the programmed implant sites) suggested choosing a lateral approach [1, 17]. Further- more, CBCT highlighted the presence of two symmetrical Underwood septa, which are to be carefully evaluated in the surgical planning.
A sequential digital process was employed in creating a surgical stent to guide maxillary sinus antrostomy with the following steps [18]:

CBCT DICOM files and virtual diagnostic wax-up were superimposed using a guided surgery software and virtual implant planning was performed.
1) CBCT DICOM files and virtual diagnostic wax-up in STL format were superimposed using a guided surgery software (CREA 3D Guided Surgery, BioSAFin – Media Lab, Trezzano Rosa, Italy) and virtual implant planning was performed (Fig. 1).
2) All data were uploaded into the software CREA 3D AI JARVIS (BioSAFin - Media Lab, Trezzano Rosa, Italy), which employs artificial intelligence algorithms to analyze dental radiographic images and automatically segment the anatomical areas of interest. In this specific case, automatic segmentation of the maxillary bone and subsequent export in STL format have been requested.
3) The entire dataset was transferred to CREA 3D Sculpt software (BioSAFin – Media Lab, Trezzano Rosa, Italy), where the surgical guide was planned. This process factored in parameters, like antrostomy shape, size, and position. Once these antrostomy details were precisely defined, a tooth-supported surgical guide was designed, aiming to assist in implant placement and enable real-time visualization of the predetermined bony window during the procedure (Figs. 2-3). The final project of the surgical guide was then saved in STL format.
4) The surgical guide was then manufactured in biocompatible medical resin using a 3D printer (Envision One cDLM, EnvisionTec, Gladbeck, Germany) and sterilized using ethylene oxide gas [19] (Fig. 4).
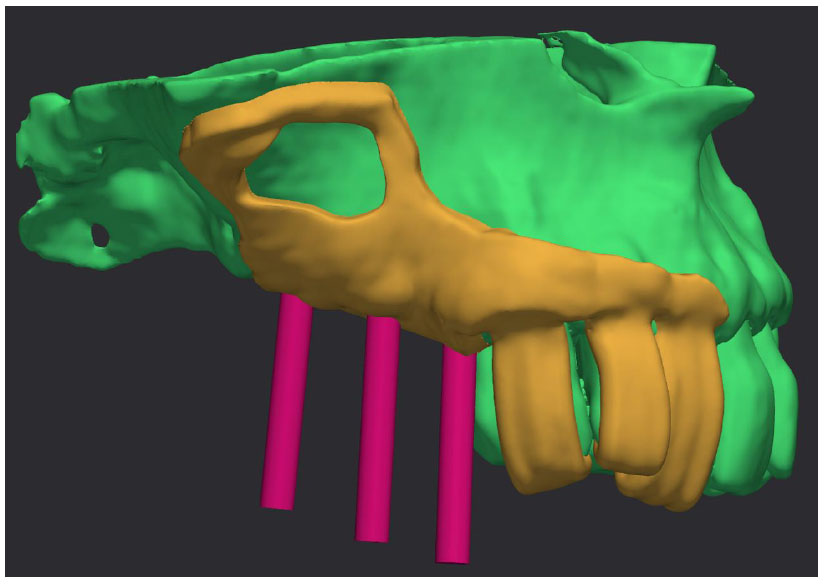
A tooth-supported surgical guide was designed on the AI-generated model, aiming to guide implant placement and enable real-time visualization of the planned antrostomy.
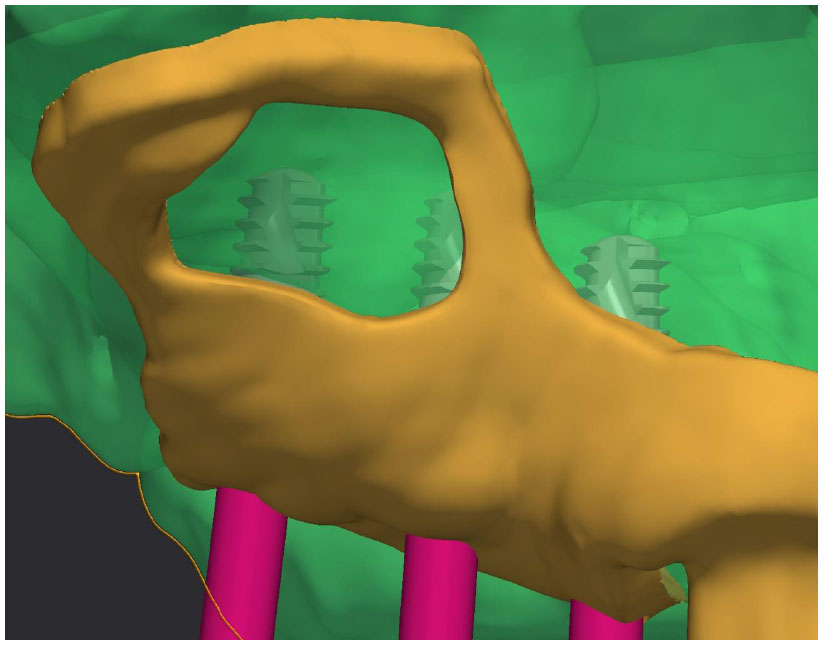
Closer detail of Fig. (2), showing planned implant positioning.

The surgical guide was manufactured using a biocompatible 3D printing resin for medical applications.
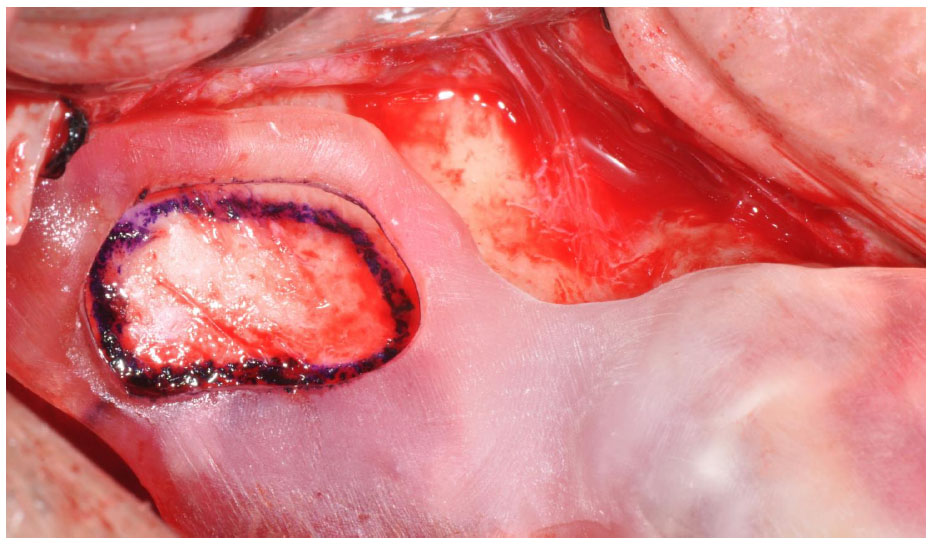
The surgical guide was carefully stabilized in the correct position and the antrostomy area was marked on the bony wall using a surgical pen.
2.1. Surgical Procedure
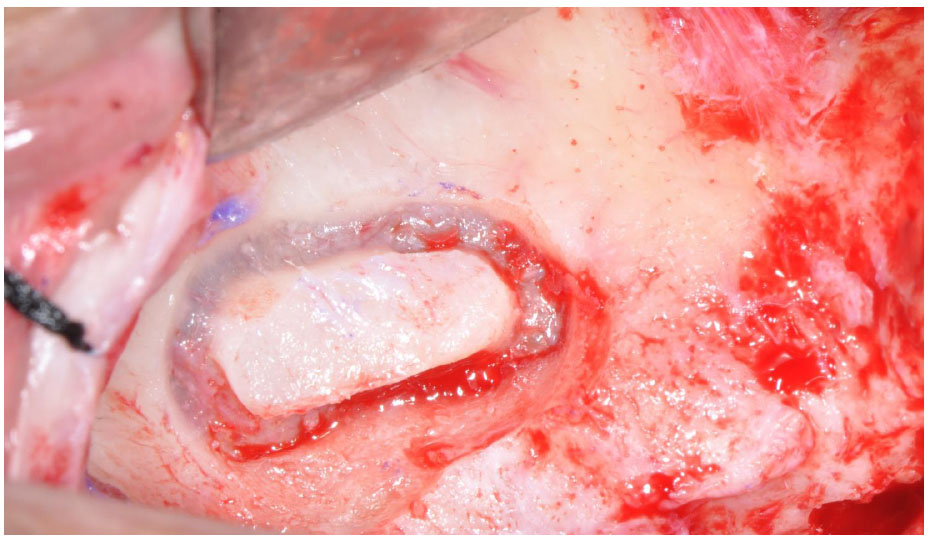
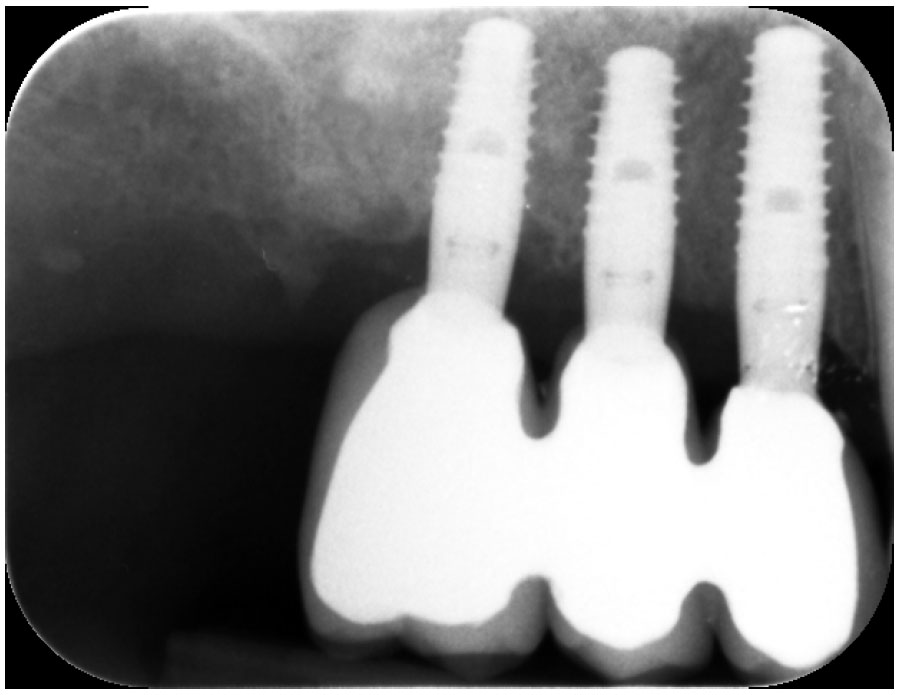
Under local anaesthesia (4% articaine with 1:100.000 epinephrine), a full-thickness flap with two releasing incisions was elevated to expose the lateral bone wall of the posterior maxilla. The tooth-supported surgical guide was carefully stabilized in the correct position, and the antrostomy area was marked on the bony wall using a surgical pen (Fig. 5). After removing the template, the antrostomy was performed using diamond round burs (Figs. 6-7) and the bony window was reflected into the sinus cavity [3]. Following the traditional surgical steps, the Schneiderian membrane was then detached and elevated using manual instruments, until exposing the medial wall of the sinus. The sub-antral space was then grafted with a composite graft formed by anorganic bovine bone (Bio-Oss, Geistlich, Wolhusen, Switzerland), mixed in 50:50 proportion with autologous bone harvested from the same surgical site. Three implants (KE, BioSAFin, Trezzano Rosa, Italy) were then inserted using the surgical guide (Fig. 8) and the antrostomy site was covered with a resorbable bovine collagen membrane (Bio-Gide, Geistlich, Wolhusen, Switzerland). The flaps were finally sutured with the Sentineri technique [20] and single stitches with 5.0 non-resorbable synthetic monofilament. No intra-operative complications (i.e., membrane perforation and haemorragic events) were recorded and post-operative panoramic radiograph confirmed satisfactory vertical augmentation without any sign of graft dissemination (Fig. 9). Implants were uncovered after a six-month healing period, demonstrating successful osseointegration and soft tissue health (Fig. 10). Screwed metal-ceramic crowns were delivered after two additional months (Fig. 11).
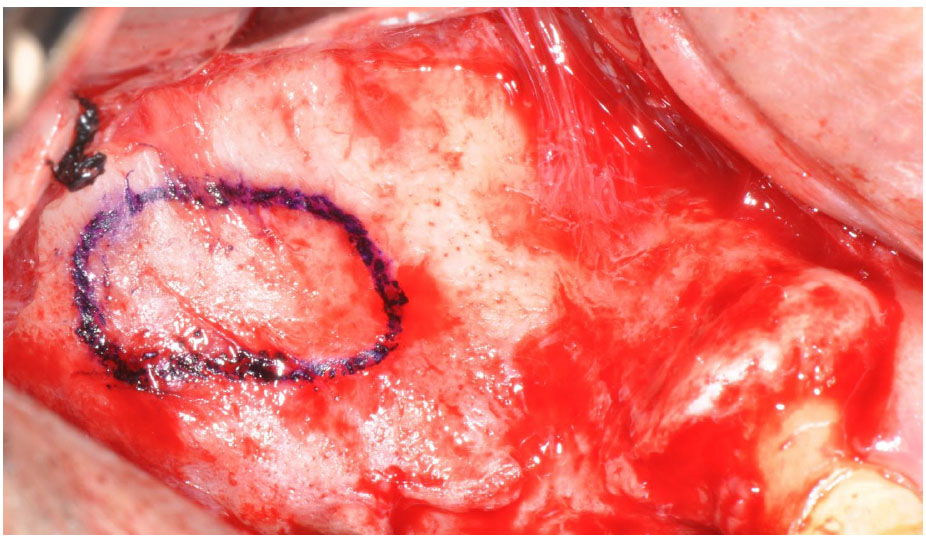
After template removal, the position and shape of the programmed antrostomy were clearly visible on the lateral wall of the sinus.
The antrostomy was performed in the planned position using diamond round burs.
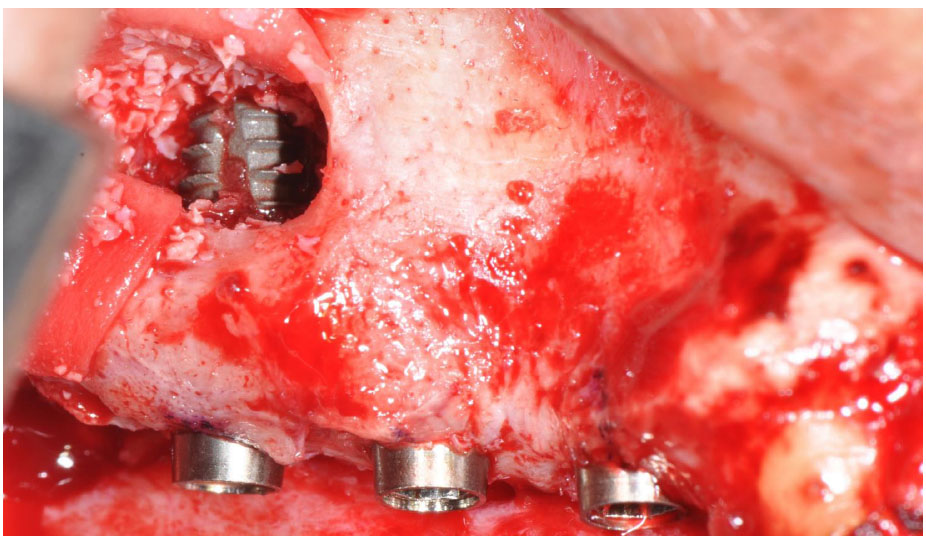
Three tissue-level implants (KE, BioSAFin, Trezzano Rosa, Italy) were inserted using the same surgical guide.
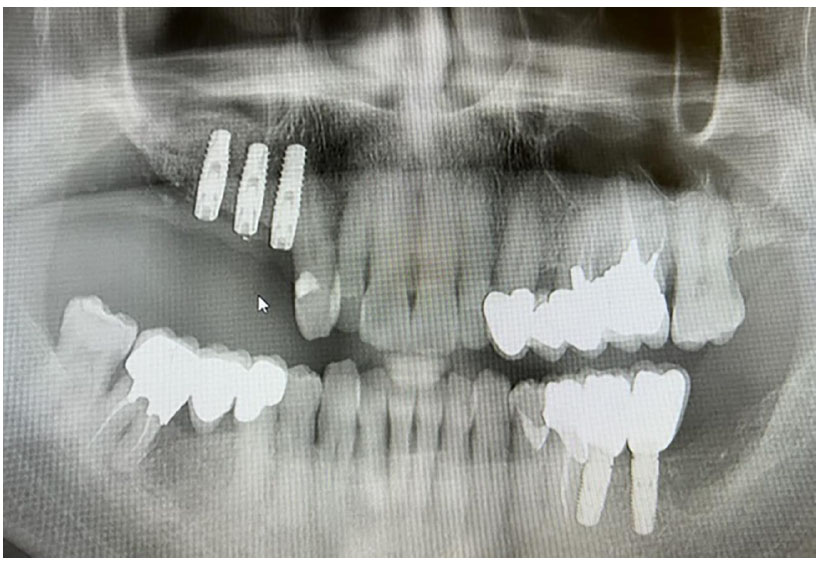
Post-operative panoramic radiograph confirmed satisfactory vertical augmentation with no sign of graft dissemination.
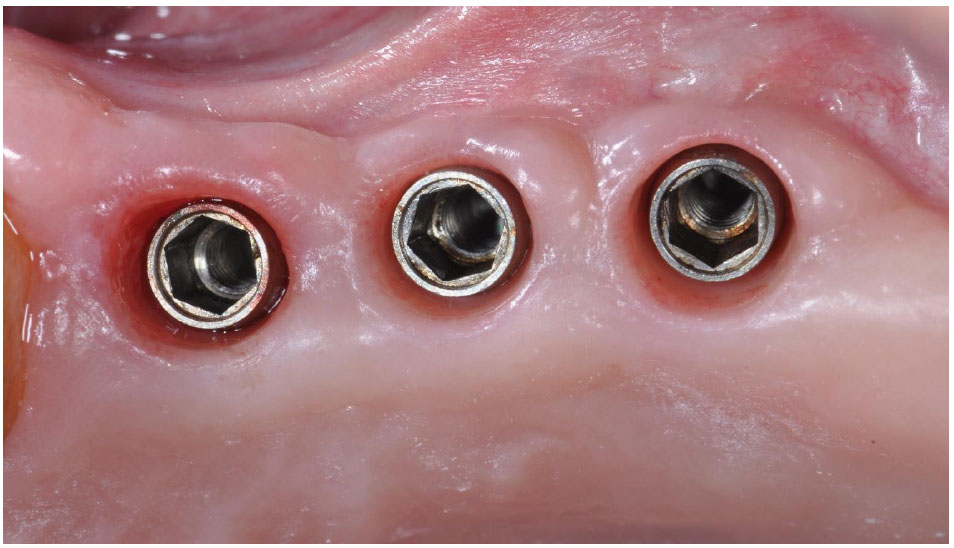
After the second-stage surgery, all of the three tissue-level implants demonstrated successful osseointegration and soft tissue health.
Screwed metal-ceramic crowns were delivered two months after second-stage surgery.
3. DISCUSSION
The opening of the bony window on the lateral wall of the maxillary sinus (or antrostomy) is a crucial moment for the success of the entire procedure of sinus augmentation. Its location must be carefully planned in the pre-operative phase, taking into account the following factors: i) the coronal border positioned 2-3 mm apical to the sinus floor and drawn following its course; ii) the apical border positioned parallel to the coronal border, at a distance of 8-10 mm; iii) the mesial border positioned as close as possible to the anterior wall of the sinus; iv) the distal border determined by the number of implants to be inserted; v) evaluation of the possible intraosseous course of the alveolar-antral artery and/or the presence of Underwood septa (which may require the creation of two antrostomies) [21, 22]. In order to minimize intra-operative complications in maxillary sinus floor elevation, it is well documented in the literature that the use of piezosurgery with its selective cutting on hard tissues significantly reduces the likelihood of membrane perforations or vascular injuries. However, in this case report, the antrostomy preparation was performed using rotating instruments for logistical reasons [23, 24]. Furthermore, in this specific case, tissue-level implants with a convergent collar were used to exploit the ability of these implants to better maintain peri-implant bone levels in the medium and long term [25, 26]. This is achieved through the coronal displacement of the implant-abutment micro-gap, which is not located at the bone level but within the supracrestal soft tissue.
Given the standardization of the surgical intervention, the use of 3D-printed surgical guides, obtained from a digital workflow, may represent a considerable advancement. The guide serves as a navigational aid for the oral surgeon, offering a visual roadmap throughout the entire procedure. It enables intra-operative visualization of the planned bony window, providing clear guidance for accurate execution of the antrostomy and, later, for implant placement. This real-time visualization is instrumental in ensuring that the surgical steps align precisely with the predetermined parameters established during the planning phase. LAIDA aims to prevent the involvement of anatomical structures, such as Underwood septa and the alveolar-antral artery, which may lead to surgical intra-operative complications, such as membrane perforation or uncontrolled bleeding [7, 8, 10]. Moreover, by allowing for precise visualization during the procedure, LAIDA minimizes the need for intra-operative adjustments, reducing surgical time and enhancing overall workflow. This contributes to improved patient comfort and more predictable surgical outcomes.
Mandelaris and Rosenfeld [16] pioneered the utilization of a sinus guide in 2008. Their protocol involved the creation of two distinct cutting guides: one exclusively for the superior border and a second guide for the remaining borders. The design and fabrication of the guide were accomplished through a stereolithography system provided by a surgical guide company. Since then, numerous articles have been published describing various techniques for creating a sinus guide in a simple and predictable manner [18, 27-41]. Among them, Osman et al. (2018) conducted a comparison of the effectiveness of CAD-CAM-based antrostomy guides against the conventional lateral window approach technique, focusing on reducing the incidence of membrane perforation. The study showed that computer-guided sinus floor elevation exhibits promising results, effectively reducing perforation rate, with the potential to serve as a secure alternative to the standard technique [29].
Bishbish et al. (2023) showed that planning and execution of the lateral window osteotomy, along with the implant osteotomy, can be precisely carried out through the use of dynamic navigation technology [42]. This is a further confirmation that navigational systems in implantology, such as dynamic navigation, have demonstrated promising outcomes. However, they are associated with elevated costs and demand a significant learning curve for effective utilization.
Although following LAIDA workflow may initially consume time, it should be noted that complications possibly arising during surgery due to imprecise planning necessitate more time for correction compared to computer-guided surgical procedures. This not only prolongs the surgical duration, but also exposes the patient to increased surgical trauma. An additional benefit of LAIDA involves integrating DICOM datasets with STL files from intraoral scans or scanned models. In contrast to traditional methods, this entirely digital workflow significantly simplifies surgical guide production. It eliminates the need for an extra radiological template during 3D imaging for the final surgical guide creation. Therefore, there is no need for additional scheduling, costs, or notably, additional radiation exposure for the patient [43]. Furthermore, the use of artificial intelligence allows an automatic segmentation (the process of separating or isolating specific structures or regions of interest within CBCT), ensuring precision and repeatability in the creation of the three-dimensional anatomical model.
However, it is important to note that while tooth-supported surgical guides offer remarkable advantages, they require careful planning, expertise in digital dentistry and oral surgery, and adequate training for their optimal utilization. Furthermore, their success is dependent on the quality of pre-operative imaging and accurate data transfer to the software used for guide fabrication.
CONCLUSION
Pre-surgical planning of regenerative surgery is mandatory, with consideration of all the risks associated with the intervention. The use of a surgical guide for the realization of the antrostomy may therefore represent an aid to the oral surgeon, leading to the reduction of intra-operative complications, such as membrane perforation and bleeding events following injuries to the alveolar-antral artery. Furthermore, this technique may lead to a reduction in terms of surgical time.
LIST OF ABBREVIATIONS
| LAIDA | = Lateral Antrostomy Integrated with Digital Approach |
| CBCT | = Cone Beam Computed Tomography |
| DICOM | = Digital Imaging and COmmunications in Medicine |
| STL | = Standard Tessellation Language |
| AI | = Artificial Intelligence |
| CAD-CAM | = Computer Aided Design-Computer Aided Manufacturing |
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study will be available from the corresponding author [C.S] upon special request.


