All published articles of this journal are available on ScienceDirect.
Full-Mouth Rehabilitation Using Combined Multiunit Abutment and Screw-Retained T-Base Abutment System: A Case Report with 24-Month Follow-up
Abstract
Introduction
The application of a multiunit abutment system in combination with a screw-retained T-base abutment for the all-in-six restoration of dental arches is considered a successful treatment for the maxillary and mandibular arches with implant-supported fixed prostheses.
Case Report
This case report presents the successful use of a multiunit abutment system combined with a screw-retained T-base abutment to support all-in-six implant-supported fixed prostheses in maxillary arches. Meticulous treatment planning and execution resulted in predictable and favourable outcomes after implant-supported fixed prostheses were applied to a patient exhibiting a partially maxillary arch with mobile grade III bilateral canines.
Conclusion
The treatment protocol, prosthetic components, and clinical and radiographic outcomes after the final restoration were excellent after 24 months.
1. INTRODUCTION
Dental implants are prosthetic devices or substances made of alloplastic materials and inserted into oral tissues beneath the mucosal and periosteal layers and on or within the arch bone. These implants support fixed or removable dental prostheses (FDPs or RPDs). Thus, a portion of an implant provides support for a dental implant abutment through adaptation on (eposteal), within (endosteal), or through (transosteal) the bone [1].
Full-arch implant-supported rehabilitation has attracted considerable interest in recent years because it restores oral function and improves the quality of life of patients with severe tooth loss [2, 3]. A combination of a multiunit abutment system and a screw-retained T-base abutment is usually preferred in delayed loading protocols because it ensures stability, retention, and aesthetic outcomes for arch restoration and results in minimal hard tissue morbidity [4, 5].
RPDs effectively replace missing teeth, facilitating oral function restoration and improving aesthetics. However, using removable dentures in the maxillary or mandibular arch presents issues related to stability, retention, and comfort, impacting patients’ daily activities and quality of life [6, 7]. Addressing these issues ensures optimal patient outcomes. Koul et al. and Nand and Mohammadnezhad highlighted challenges, such as denture instability, speech and eating difficulties, and oral tissue discomfort, which afflict individuals relying on RPDs in one of the arches or both arches [8, 9].
Hybrid prostheses offer numerous advantages over all-in-six implants in dental restoration. First, hydride prostheses provide enhanced stability and support because of their fixed and full-arch designs, which improve chewing efficiency and speech. They reduce overall cost and surgical time by requiring fewer implants and are comfortable and convenient because no dentures need to be removed and cleaned [10, 11]. High success and survival rates were recorded in a systematic review that investigated the short-term (5–10-year mean follow-up) and long-term (10 years or more) uses of fixed full-arch dental hybrid prostheses and supporting dental implants [12]. These results are supported by other studies, which demonstrated the long-term effectivity and satisfaction of implant-supported prostheses in patients with hybrid prostheses; thus, full-arch dental hybrid prostheses are viable and beneficial options for dental rehabilitation [13, 14]. The aim of this case report is to demonstrate the effectiveness of combining a multiunit abutment system and screw-retained T-base abutment for the treatment of a medically fit elderly patient who had loosening or remaining natural teeth and was experiencing discomfort when wearing maxillary and mandibular RPDs.
2. CASE PRESENTATION
The 66-year-old male patient had a fixed prosthesis and was complaining about ill-fitted maxillary and mandibular dentures for 6 years. He was suffering from pain and showed tooth mobility of the maxillary right and left canines. Apart from not smoking, he was medically and clinically fit. Extraoral findings were as follows: lip competence, symmetry of the face, normal mandibular movements, and temporomandibular joints. His intraoral findings showed normal soft tissues and the presence of bilateral maxillary canines in the maxillary arch. The remaining mandibular teeth were teeth 35, 33, 32, 31, 41, 42,43, 45, and 47 (Fig. 1A). The remaining teeth had grade 3 mobility, and the occlusion was a class I relationship. The panoramic view showed severe generalized horizontal bone loss and localized vertical bone loss in relation to teeth 13 and 23, the mesial roots of tooth 47, the insufficient crown root ratio of the remaining teeth, mesially or distally tilted teeth, and the overeruption of opposing teeth (Fig. 1B). CBCT showed the proposed sites for implants and poor bone levels in relation to the maxillary sinus floor (Fig. 1C). Data were collected for treatment planning. The vertical dimension with both RPDs was measured, and no loss in the vertical dimension was observed. Finally, maxillary and mandibular diagnostic impression, scaling, and root planning for the remaining teeth were performed.
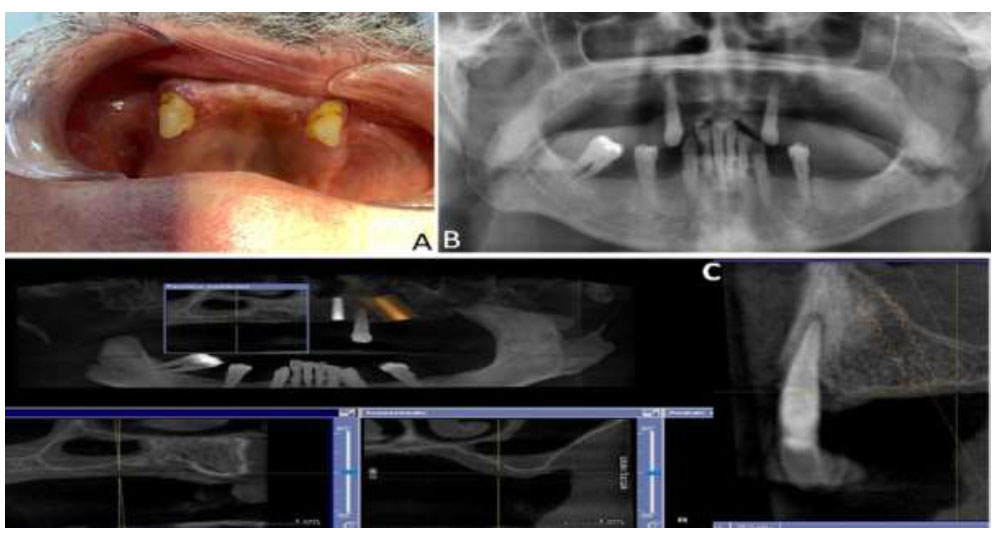
Preoperative view (A) intraoral (B) OPG, CBCT showing different sites and relation to maxillary floor of the sinus.
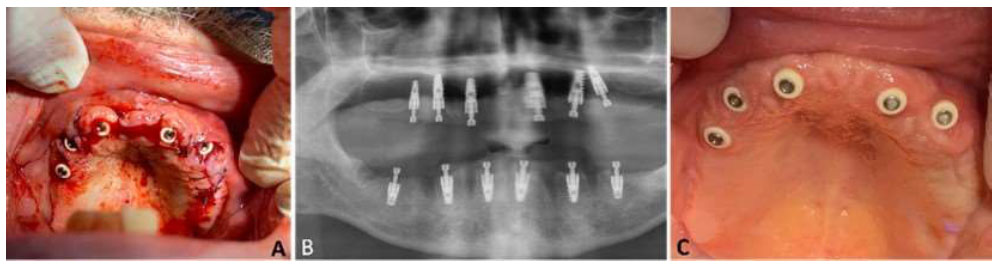
Implant insertion and sutures in place after the extraction of both canines (A), immediately after OPG (B), and after three weeks of healing (C).
The patient was diagnosed with partially edentulous dentition in both arches. The treatment protocol had preoperative assessment, surgical, restorative, and follow-up phases. After data interpretation, the extraction of remaining teeth was needed because of severe mobility and insufficient crown: root ratio or super eruption resulting in occlusal interferences with opposing teeth. Then, treatment options were discussed with the patient, including maxillary and mandibular RPDs and maxillary and mandibular implant-supported implants with maxillary sinus lifting. The patient had no preferred type of fixed implant-supported prosthesis, but he refused to undergo sinus lifting because he preferred a treatment that results in a low degree of tissue morbidity and saves time. The patient signed a consent form. The steps, types of maxillary and mandibular prostheses, and modifications were considered in treatment planning. A tilted implant was applied to the maxillary arch because of anatomical limitations. The patient was instructed to rinse his mouth with chlorhexidine 2% (FIMODENT Collutorio Antiplacca, Italy) twice a day until his next appointment.
During his second visit, topical iodine antiseptic (PHARMA Trade Company, Italy) was applied intra- and extra-orally. The surgical phase was started with conventional implant surgery protocols; no surgical guide or stent was used for the extraction of the remaining teeth after local anaesthesia injection. Then, maxillary canines were extracted, mid crestal flap incision was performed, and the mucoperiosteal flap was elevated. The drilling protocols of the manufacturer (B & B DENTAL Implant Company, Italy) were used. Six implant sites were drilled in each arch and selected according to bone density and available bone, and modifications were carried out on both distal implants, which were placed in a tilted position to prevent sinus complications (Fig. 2A).
EV-type implants with 24 × 25 × 15 B/B areas were used instead of 4.2 × 10 implants, which had aggressive threads resulting from poor bone quality, and three type-3P implants with B/B dull implant threads were used because the vascularity of the bone was almost equal to the D2 size of a 3.75 × 11.5 implant. In the mandibular arch, six implants were inserted in the same manner as those in the maxillary arch. A panoramic image was obtained immediately after the insertion of dental implants in both arches (Fig. 2B). After implant insertion, the healing abutment from the PEEK material from the same company was used, and then flap closure was carried out using a Vicryl 4/0, which ensured a simple and horizontal mattress suture. Postoperative and post-surgical instructions were given to the patient (Fig. 2C).
In the prosthetic phase, after the healing time of six months in the upper jaw and three months in the lower jaw, implant-level impressions were obtained using open-tray impression copings (Fig. 3A). Each tray was fabricated and used to obtain another impression, and multiunit abutments were mounted over the implants according to the first impressions obtained using a multiunit abutment from the same company. Then, transfers for the multiunit abutments were ligated together with the other T base abutments using Duralay resin materials from (Reliance Dental Manufacturing LLC, USA), and impression adhesive from 3M was applied to each tray from inside. Then, a heavy-body silicone impression material (Express 2 VPS Impression Materials, 3M, ESPE, USA) was poured into the trays at the same time as light-body silicon from the same brand impression materials was applied to soft tissues. All transfers were covered, and the trays were inserted carefully. After the material setting, the precise impression was delivered to the technician, and a healing abutment was remounted over an implant. Then, bite preparation and registration were performed, and the vertical dimension was calculated. The impression was then delivered back from the laboratory for the metal try-in. The metals were obtained as separated maxillary and mandibular arches after milling with chrome–cobalt bar (CMC Company, Italy), which was constructed with a CAD/CAM system (Zirkonzahn Dental Milling Machines, Germany). A metal bar (induction-hardened and chromed plated bars) was then used, which was milled by C.M.C. Company (ITALIA S.R.L). Then, metal copings were clinically tested individually and simultaneously, as shown in Fig. (3B). The tested metals for both arches were returned to the laboratory and covered with composite teeth (AZDENTR, China) after the mounting of both arches on an articulator.

Healing of gingiva around the implant and multiunit abutments (A) and both arches during metal try-in (B) after 6 months.
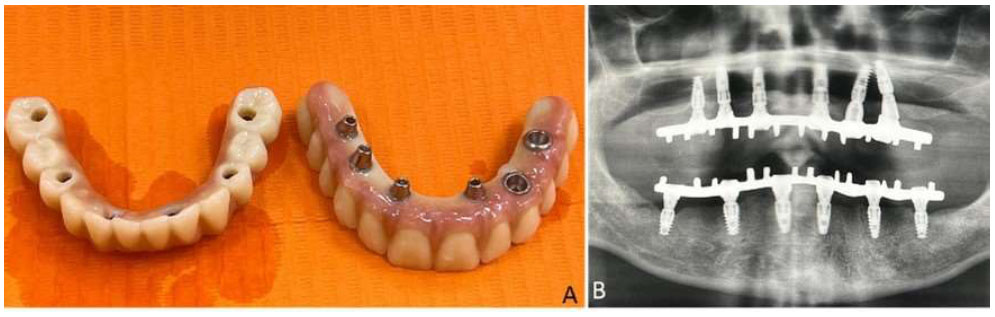
Implant-retained maxillary and mandibular prostheses (A) and OPG on the day of insertion (B).
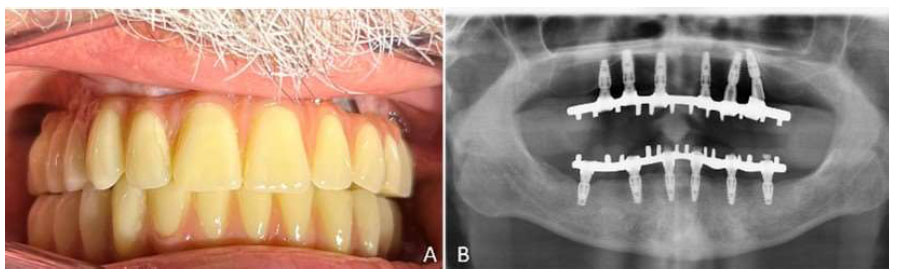
Postoperative (A) and intraoral (B) OPG after 24 months.
The final prosthesis was connected to the multiunit abutments by using screw-retained T-base abutments, which provided a stable and retrievable framework. The maxillary and mandibular implants supported the prostheses for both arches and occlusal adjustment was performed on each arch during mandibular movements (Fig. 4A). An OPG was obtained before the patient left the clinic (Fig. 4B), and postinsertion instructions were provided.
The patient was recalled regularly 1 week and 3, 6, 12, and 24 months after the insertion of the prostheses. The patient was comfortable, satisfied, and happy with his fixed prostheses. Post-operative intraoral view showed good outcomes, and no bone resorption was observed, as indicated by the OPG results 24 months after the delivery of the prostheses (Figs. 5A and B).
3. DISCUSSION
In recent years, full-arch implant-supported rehabilitation has attracted considerable interest because it can restore oral function and enhance the quality of life of patients with extensive tooth loss [2]. In this study, a multiunit implant-supported prostheses system (all-in-six) and a screw-retained T-base abutment were successfully combined to provide stability and ensure retention and aesthetic outcomes for the patient. This approach reduced hard-tissue morbidity and eliminated the need for a sinus lift procedure. It involved two types of abutments with a hybrid prosthesis and satisfied the patient’s dental implant treatment needs. All-in-six restoration resulted in satisfactory aesthetic and functional outcomes and ensured stability, retrievability, and ease of maintenance [10, 15].
Implant-supported hybrid prostheses offer notable advantages over RPDs in dental rehabilitation. By affixing the prosthesis to dental implants, we were able to markedly enhance stability and ensure retention, eliminating issues associated with denture movement and potential discomfort. The enhanced stability ensured natural oral function during mastication and speech, thus improving patient confidence and overall quality of life [4, 16-19]. Additionally, hydride implant–supported FPD prostheses eliminated the need for adhesives or clasps, alleviating hygiene concerns and simplifying daily maintenance. Moreover, they effectively preserved the underlying bone through the stimulation provided by implant integration, preventing bone resorption, which commonly occurs in individuals with RPDs. These collective attributes render implant-supported hybrid prostheses viable treatment options for edentulous individuals seeking optimal oral rehabilitation outcomes [4, 18, 19].
In the present case, treatment was performed based on a systematic approach recommended by textbooks. The preoperative phase involved proper clinical examination, CBCT imaging, and intraoral photography, which were performed to determine the proper and ideal implant number and positions. However, the positions of the implants were raised because the patient refused to undergo sinus lifting onthe maxillary left side. This approach reduced hard tissue morbidity, eliminated the need for a sinus lift procedure and bone removal, and minimized surgery and healing period [20]. Subsequently, the surgical phase mainly subjected oral tissues to traumatic extraction for primary implant stability. Six implants were placed in each arch edentulous arch [21, 22]. Moreover, the implant survival rate in the maxilla tends to decrease with increasing levels of alveolar atrophy and is low under moderate‐to‐severe atrophic conditions [23].
The use of hybrid prostheses for full-mouth rehabilitation has garnered substantial attention within contemporary dental prosthetic practice. This approach involves the use of implant-supported fixed prosthetic frameworks, combining the advantages of dental implants with those of RPDs [10]. By securing a hybrid prosthesis over implants, the inherent stability and longevity of implant-supported restoration synergized with enhanced aesthetics, functional capacity, and patient satisfaction associated with implant-supported fixed prostheses [15]. These attributes constitute a comprehensive oral rehabilitation strategy, which is beneficial to edentulous and severely compromised dentition cases, thereby affording patients an improved quality of life and dental functionality [10, 15].
Additionally, in the prosthetic phase following the healing periods, a proper impression is associated with the registration of arches. Thus, using composite artificial teeth in the fabrication of implant-supported prostheses has attracted attention in contemporary prosthodontic practice. This methodology involves the incorporation of composite resin teeth onto metal bases, offering distinct benefits in terms of aesthetics, mechanical properties, and ease of chairside modification [15, 16]. It is compatible with oral characteristics, thus presenting a promising avenue for optimizing patient comfort, functional efficacy, and overall treatment outcomes [17]. Furthermore, the material’s inherent flexibility and shock-absorbing properties can potentially mitigate occlusal forces, enhancing the longevity of prostheses and underlying structures [15-17]. Mudliar et al., 2022 stated that denture teeth of the same material should be used as antagonists where possible, and the superficial outer layer of the teeth must be preserved as much as possible during intra-oral adjustments occlusal adjustments to minimize the wear resistance of the opposing teeth [24].
Finally, with regard to the amount of bone around the implant necks in both arches, a well-integrated implant was obtained during the follow-up period and after 24 months of survival function. We detected no complications, such as peri-implantitis, and changes or resorption after comparing the OPG results immediately after delivery (Fig. 4B) and those obtained after 24 months (Fig. 5B). During the follow-up periods, stable results in terms of aesthetics and functions were obtained in both arches, and excellent oral hygiene status was observed.
CONCLUSION
This case report demonstrates the successful application of a multiunit abutment system in combination with a screw-retained T-base abutment for the all-in-six restoration of the maxillary arch with implant-supported fixed prostheses. The approach resulted in optimal aesthetic and functional outcomes, thus improving the quality of life of the patient. The strategic removal of teeth with questionable prognoses for the delivery of a hybrid prosthesis with implant-supported maxillary and mandibular full-arch restorations should be applied to certain types of patients. Furthermore, a longer follow-up period is warranted for the evaluation of the long-term success and maintenance of this treatment modality.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Approved by University of lbn al-Nafis for Medical Science (Ref 160) dated 15/11/2021.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.


