All published articles of this journal are available on ScienceDirect.
Assessment of Panoramic Radiograph Errors: An Evaluation of Patient Preparation and Positioning Quality at Soelastri Dental and Oral Hospital
Abstract
Background:
Dental radiography is an important component of comprehensive patient care. One of the most frequently used extraoral radiographic techniques is panoramic radiography. Panoramic radiographs lose value when the quality of the diagnostic radiographs is poor. In their application, there are still many errors that occur in panoramic radiographs.
Objective:
This study aimed to determine the quality and frequency of panoramic radiograph errors due to patient preparation and positioning errors at the Soelastri Dental and Oral Hospital, Universitas Muhammadiyah Surakarta (RSGM Soelastri UMS), Indonesia.
Methods:
This type of research is descriptive, quantitative, observational, and takes a retrospective approach. A total of 312 panoramic radiographs of patients at RSGM Soelastri UMS from January to December 2021 who met the inclusion and exclusion criteria were taken at random stages and evaluated. Radiographs were compared with ideal quality, given a National Radiological Protection Board (NRPB) rating, and the frequency of errors that occurred was evaluated.
Results:
The most common rating obtained on panoramic radiographs in this study was 2 of 173 (55.45%). The frequency of preparation errors was 1.22%, while the frequency of patient position errors was 98.78%. The highest patient position error was not placing the tongue on the palate, which was 49.68%.
Conclusion:
The quality of panoramic radiographs at RSGM Soelastri UMS in the period from January–December 2021 generally has a rating of 2, according to the NRPB, and there are still errors in patient preparation and positioning.
1. INTRODUCTION
Radiology is a branch of medical science that studies the use of X-rays, radioactive substances, and other forms of radiation energy to diagnose and treat disease. Dental radiography is the process of making pictures of teeth and the tissues around them by exposing image receptors to X-rays. Dental radiography is an important component of comprehensive patient care. In dentistry, radiographs help dentists identify conditions that may not be detected or seen through clinical examination [1]. In dentistry, there are intraoral and extraoral radiographic examinations. There are several intraoral radiographic techniques, such as periapical, bitewing, and occlusal techniques [2]. Extraoral radiographic techniques include panoramic, lateral oblique, true lateral, postero-anterior, occipito-mental, and submento-vertex (SMV) radiographs. Although the intraoral technique provides a good view of the teeth, it is sometimes necessary to clearly see the entire maxilla and mandible without obstruction, which can be obtained using extraoral radiographs [3].
Since they were first used in 1950, panoramic X-rays have become popular and important for making a diagnosis [4]. Panoramic radiography is a special tomographic technique for producing flat views of the surfaces of the arches. Panoramic radiographs visualize the entire maxilla, mandible, temporomandibular joint, and surrounding tissues on one sheet of film [5]. The National Health Service in England and Wales shows that in 1991-1992, the number of panoramic radiographic examinations performed by general dentists was estimated at more than 1.5 million. In 1997, this figure had increased to 1.7 million. This figure continued to increase until 2001-2002 when panoramic radiographs were taken in as high numbers as 2.2 million [6].
Mainly, panoramic radiography is indicated at the first visit for patients who want routine visits to the dentist or have certain needs, such as pain or esthetics [7]. Panoramic radiography is also indicated to assess growth and development in children and adolescents and to visualize the mixed dentition period or the evaluation of third molars. Panoramic radiography can also be used for the post-traumatic examination of the facial bones and the examination of large bony lesions. In addition, panoramic radiographs can also be useful for pre-implant examination as well as for examining craniofacial abnormalities and temporomandibular joint disease [8].

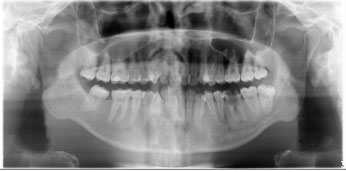
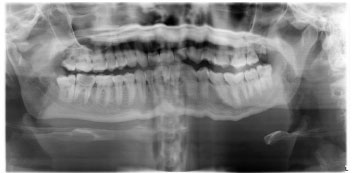
Panoramic radiography has many advantages in examining teeth and maxillofacial structures; besides that, it can image teeth, the alveolar bone, the jawbone, the maxillary sinus, the nasal cavity, and the temporomandibular joint simultaneously in one projection (Fig. 1). The procedure for taking radiographic images using panoramic techniques is fast, easy, and inexpensive [9]. Panoramic radiography provides a low dose of radiation exposure. The dose of radiation exposure in the full-mouth series is five times higher than in the panoramic technique [10]. The effective dose of 18 full mouth radiographs with F-speed film and spherical collimation is 170.7µSv. In the case of square collimation, the dose of 18 full-mouth radiographs with F-speed film is 34.9 μSv. The effective dose of 4 bitewing radiographs with F-speed film and square collimation is 5.0 μSv. The doses from panoramic radiographs with CCD are 14.2 and 24.3 μSv. Panoramic radiography can offer a better dose advantage compared to performing multiple intraoral radiographic examinations [11, 12].
Panoramic radiographs lose value when the quality of the diagnostic radiographs is poor. The low quality of radiographs can lead to misinterpretation, which can lead to misdiagnosis and treatment planning errors. Undiagnosed image quality often requires additional images and re-examination. The quality of the radiograph is influenced by the patient's preparation, patient position, and the subsequent selection of the appropriate amount of radiation exposure. Processing errors can be reduced by using digital processing techniques. Operators should pay more attention to patient preparation and patient positioning to obtain clear and undistorted panoramic views [12].
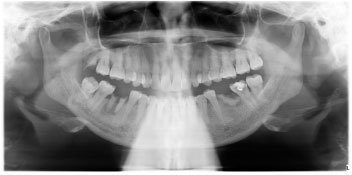
The movement of the panoramic radiography technique, the X-ray source, and the image receptor rotate around the patient's head, creating a curved focal trough. The focal trough, namely the zone where an object enters it, is clearly delineated. Objects in front of or behind the focal trough appear blurred and are largely invisible. The panoramic machine creates a focal trough that encloses the teeth and their surrounding supporting tissues [13]. Focal trough panoramic radiographs are designed to be shaped like a horseshoe according to the shape of the dental arch (Fig. 2) [12]. Therefore, it is very important to prepare the patient well and carefully position the patient's head in the focal trough to create a diagnostically useful panoramic radiograph [13].
The steps for taking panoramic radiographs include the following: a) the operator explains the procedure to the patient for taking radiographs [1]; b) all metallic objects from the neck to the head must be removed [8]; c) The operator fits a lead apron without a thyroid collar and fixation [1]; d) the radiographer positions the patient in 3 main planes, namely the midsagittal, vertical, and anteroposterior planes [14], as shown in Fig. (3); e) the patient is instructed to swallow saliva and place his tongue on the palate [15]; and f) the patient is advised not to move during the procedure [1]. Rondon et al. also explained that successful panoramic radiography requires careful positioning of the patient and proper technique. The proper technical procedure requires the patient to be upright with the shoulders down, the back straight, and the feet together. Frankfort plane should be parallel to the ground and the median sagittal plane perpendicular to the ground, with the chin placed on the chinrest with the tongue against the palate [16].

A study found that out of 1782 radiographs, only 196 (11%) had no errors, and 1586 (89%) showed positional errors. The most common positional error was an error in the position of the tongue that was not attached to the palate (55.7%), and the most rarely encountered was an error caused by the patient's movement while taking pictures (1.6%). Only 11% of panoramic radiographs are in the excellent category, 64.1% of the radiographs are in the diagnostically acceptable category, and 24.9% are unacceptable [17]. In a study done by Khan et al., they looked at 480 panoramic X-rays and found that 100 of them (21%) had no mistakes during preparation or when they were put in place. A total of 380 (79%) radiographs had preparation or position errors. The most frequently encountered preparation error was the patient's mistake in positioning the tongue (62.5%), and the most rarely encountered was the patient's mistake using a nose piercing (8.3%). Only 21% of the radiograph results are included in the excellent category [18]. From October to December 2014, research at RSGM FKG Universitas Airlangga found that 80 panoramic digital radiographs failed and only 20 were of good quality. Position errors were found in as many as 78% of cases, while technical errors were only 2%. Most positional errors have to do with where the patient's tongue is, not where it is on the palate [19].
Soelastri Dental and Oral Hospital, often referred to as Rumah Sakit Gigi Mulut (RSGM) Soelastri, is a special dental and oral hospital owned by the Universitas Muhammadiyah Surakarta and is currently the only class C special dental and oral hospital in the city of Surakarta, Indonesia. Oral and dental hospitals are organized with the aim of providing facilities to improve the quality of service, education, and research in the field of dental and oral health from basic to specialist levels in accordance with the demands of the community and developments in medical and dental science and technology, as well as being a means of referral efforts. RSGM Soelastri's radiology installation itself uses digital processing. Therefore, it is necessary to do research to evaluate the quality and errors of panoramic radiographs at RSGM Soelastri UMS so that they can be identified and corrected in the future.
2. MATERIALS AND METHODS
This type of research uses descriptive, quantitative, and observational methods with a retrospective approach. This research met research ethical standards and complied with the Helsinki Declaration, as evidenced by ethical clearance. A letter of ethical eligibility (Ethical Clearance) was obtained from the Health Research Ethics Commission (KEPK) by RSUD Dr. Moewardi with letter number 478/IV/HREC/2022. The sample in this study was secondary data in the form of panoramic radiographs taken at RSGM Soelastri UMS in January–December 2021, which met the inclusion and exclusion criteria. The inclusion criteria were soft-file panoramic radiographs of permanent dentition patients at RSGM Soelastri taken by certified radiographers, while full edentulous patients were excluded.
In this study, the Slovin formula with a 5% margin of error was used to figure out the sample size. The minimum sample size for the 1218 population was 302. Then, a random sampling of 26 panoramic radiographs was carried out every month using roulette. The total number of panoramic radiograph samples obtained and evaluated was 312.
In panoramic radiographs, observations were made by judging the quality of the radiographs by filling out a checklist of radiographic quality criteria in Microsoft Excel. Then, it was assessed with a value of 0–7, in which each radiograph was assessed based on 7 criteria. Each criterion has a maximum score of 1. One radiograph will have a total maximum score of 7 (Table 1). Then, an observation was made to see the frequency of panoramic radiograph errors due to errors in preparation and patient position by placing a checklist ( ) on the errors that occurred (Table 2).
) on the errors that occurred (Table 2).
| Quality Criteria | Indicator | Score | |
| 0 | 1 | ||
| Contrast | Black areas (air spaces), white areas (enamel, dentin, and bone), and gray areas (soft tissue) are distinguishable (0/1). | - | - |
| Completeness of objects | Superior (orbital floor), inferior (inferior mandibular border), and left and right lateral (cervical spine) boundaries are clearly visible (0/1). | - | - |
| Distortion of size and shape | The anterior teeth are not narrowed; they widen horizontally, and the ramus, posterior teeth, and condyles are evenly enlarged so that they are symmetrical. There is no overlap of the structure of the object, and the shape of the occlusal plane is good (0/1). | - | - |
| Sharpness | The outer boundary of an object is clear and not obscured (0/1). | - | - |
| Resolution | The boundary between the periodontal ligament and the lamina dura and dentinoenamel junction is clearly visible (0/1). | - | - |
| Right-left marker | There is a label marker right and left (0/1). | - | - |
| Artifacts/ghost image | No internal or external artifacts or ghost images (0/1). | - | - |
| Radiograph Error | Kind of Mistake | Indicator | Checklist | |
|---|---|---|---|---|
| Yes | No | |||
| Patient preparation errors | Incorrect placement of protective aprons. | The protective apron casts a radiopaque shadow on the anterior side of the mandible. | - | - |
| Error not removing metallic object. | A radiopaque ghost image that may interfere with information for diagnosis. | - | - | |
| Patient positioning errors | The patient is too forward. | Blurred, shortened, and narrowed front teeth. The proximal areas around the mandibular premolars and ramus overlap. | - | - |
| The patient is too backward. | The dental arch, especially on the anterior teeth, will look blurry and widen horizontally. The condyles appear to be on the lateral margins, and the mandible and spine are also missing. | - | - | |
| The patient's chin is too high or looking up. | The hard palate and floor of the nasal cavity appear to overlap the maxillary teeth. Detail in the maxillary incisor region is also reduced. Maxillary incisors look blurry and enlarged. In the radiograph, you can see a “reverse smile line”, or one that is curving downward. | - | - | |
| The patient's chin is too low or down. | Mandibular incisors look blurred, and detail on the roots of the anterior teeth is also reduced. The mandibular condyle is not visible on the radiograph. There is an “exaggerated smile line” or an image curved up. | - | - | |
| The patient's head is asymmetrical. | The ramus and posterior teeth will look unevenly bigger, and they will look bigger on one side. The right and left condyles appear asymmetrical. | - | - | |
| The patient is not standing straight. | Radiopaque view of the patient's spine appearing in the midline and extending inferiorly. | - | - | |
| The patient moves. | Panoramic radiographs show the effects of stretched or ruptured anatomy in the zone of movement. | - | - | |
| The patient's tongue is not on the palate. | A dark air space is seen between the dorsum of the tongue and the palate (palatoglossal air space), which obscures the apical region of the maxillary teeth. | - | - | |
Data analysis was performed to describe the variable quality of the radiographs by calculating the number of criteria fulfilled for each radiograph so that the results are presented in percentage form, which was then compared with the NRPB value, as shown in Table 3 [20]. Errors in the radiographs are then presented in the form of a frequency distribution table and calculated in percentage form.
| Rating | Criteria | Interpretation |
| 1 | There were no errors discovered, and the quality criteria were met completely (100%). | Excellent |
| 2 | Fulfilling more than 50% of all quality criteria, only a few errors were found that did not affect the interpretation in determining the diagnosis. | Diagnostically acceptable |
| 3 | Fulfilling less than 50% of all quality criteria may influence the interpretation of radiographs and the determination of the diagnosis. | Diagnostically unacceptable |
3. RESULTS
The results showed that the fulfillment of the criteria for radiograph quality was highest with right and left markers, as shown in Table 4. A total of 312 panoramic radiographs, or 100%, met these criteria. It is important to label the right and left sides of the radiograph properly and clearly. Table 4 also shows that the size and shape distortion criteria, which is the lowest quality criterion, have been met. After the analysis was carried out by looking at the number of criteria fulfilled on each panoramic radiograph, it was compared with the NRPB value (Table 5). Table 5 shows that 173 (55.45%) panoramic radiographs are included in rating 2.
| Quality Criteria | Number of Samples | ||
|---|---|---|---|
| 0 | 1 | ||
| 1. | Contrast | 32.37% | 67.63% |
| 2. | Completeness of objects | 5.13% | 94.87% |
| 3. | Distortion of size and shape | 81.73% | 18.27% |
| 4. | Sharpness | 35.90% | 64.10% |
| 5. | Resolution | 64.10% | 35.90% |
| 6. | Right-left marker | 0.00% | 100% |
| 7. | Artifacts/ghost image | 3.21% | 96.79% |
| Rating | Number of Samples | Percentage |
|---|---|---|
| 1 | 55 | 17.63% |
| 2 | 173 | 55.45% |
| 3 | 84 | 26.92% |
| Total | 312 | 100% |
In addition, the results showed that 55 panoramic radiographs with a rating of 1 (excellent) found no errors, while 257 panoramic radiographs with ratings 2 and 3 still found errors. A total of 257 panoramic radiographs were evaluated to see the errors that occurred. Errors in panoramic radiographs are divided into 2 types: errors during preparation and errors in patient position. Errors on panoramic radiographs were dominated by patient position errors in 249 radiographs (Table 6).
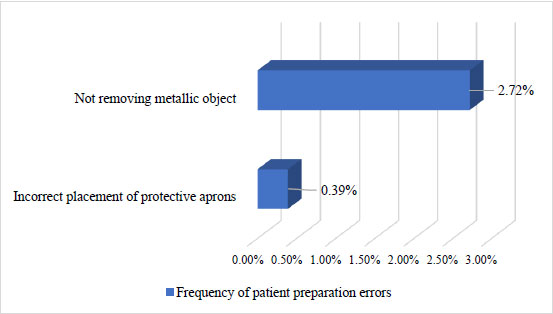
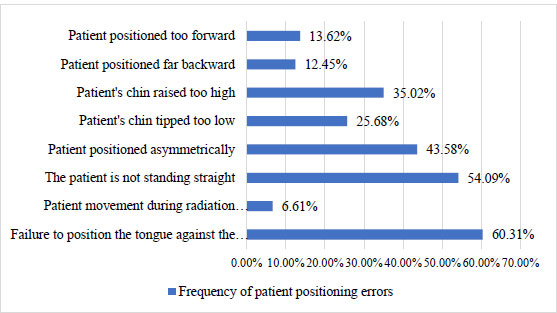
Fig. (4) shows that mistakes in preparing the patient happen most often when metal objects are not taken out. This happens in 2.72 percent of all radiographs, while mistakes in putting on protective aprons only happen in 0.39 percent of all radiographs. Fig. (5) shows that the most common patient positioning error is not putting the tongue on the palate. This happens in 60.31 percent of all radiographs, which is as many as 155 radiographs. The next order of frequency of position errors that often occur is that the patient does not stand straight (54.09%), the patient's head is asymmetrical (43.58%), the patient's chin is too high (35.02%), the patient's chin is too low (25.68%), the patient is too far forward (13.62%), the patient is too far backward (12.45%), and the patient moves (6.61%). The rarest error was found in positional errors, namely patient moving errors; only 17 radiographs experienced these errors.
| Months | Patient Preparation Errors | Patient Positioning Errors | Incorrect Patient Preparation and Positioning |
|---|---|---|---|
| 1 | 0 | 21 | 1 |
| 2 | 0 | 20 | 1 |
| 3 | 0 | 24 | 0 |
| 4 | 0 | 21 | 1 |
| 5 | 0 | 21 | 1 |
| 6 | 0 | 22 | 2 |
| 7 | 0 | 21 | 0 |
| 8 | 0 | 19 | 1 |
| 9 | 0 | 19 | 0 |
| 10 | 1 | 20 | 0 |
| 11 | 0 | 19 | 0 |
| 12 | 0 | 22 | 0 |
| Quantity | 1 | 249 | 7 |
| Total radiographs | 257 | ||
4. DISCUSSION
In digital radiography, labeling “L” (left or left) or “R” (right or right) can be done during the image editing process on a computer. RSGM Soelastri itself has used digital radiography so that the right and left marker labels have been automatically added to the panoramic radiographs. All panoramic radiographs must have a mechanism to signal automatically. Important labels are placed at the ends of the images so as not to interfere with the information for diagnosis [13].
One of the disadvantages of panoramic radiographs is the high rate of distortion. Even a slight positional error can cause image distortion [21]. Limited dimensions of the focal plane on panoramic radiographs result in small errors in position causing distortion due to uneven vertical and horizontal magnification, tooth overlap, and loss of sharpness [17]. Image magnification can be affected by several factors, such as the patient's position, the shape of the patient's jaw, gender, and the anatomy of the jaw [22]. The operator must pay special attention to the preparation and positioning of the patient to obtain sharp and undistorted radiographic images [18].
As shown in Table 5, rating 2 indicates that the radiograph meets more than 50% of all quality criteria. This is like a study conducted by Khan et al., in which 480 panoramic radiographs rated 2 had the highest rating, namely 310 (64.5%) panoramic radiographs [18]. In the study of Dhillon et al., similar results showed that rating 2 (diagnostically acceptable) occupies the highest number, namely 1142 (64.1%) of 1782 panoramic radiographs [17].
If the radiograph meets less than 50% of all quality criteria, it gets a rating of 3 (diagnostically unacceptable). This study obtained a rating of 3 of 84 (26.92%) panoramic radiographs. Aside from causing radiographs to lose their diagnostic ability, inadequate radiograph quality can also cause patients to receive unnecessary radiation exposure because they need to take repeat radiographs [23]. There are three guiding principles in radiation protection: justification, optimisation, and limitation. The principle of justification requires dentists to ensure that radiation exposure provides more benefits than the risk of harm to the patient. The principle of optimisation is using all means to reduce unnecessary exposure, or the ALARA principle (As Low As Reasonably Achievable). The third principle is limiting the dose, ensuring that no individual receives a very high dose [24]. Regulation of the Nuclear Energy Monitoring Agency (BAPETEN) Number 15 of 2014 Article 25 states that the effective dose for the public is 1 mSv in 1 year. The panoramic radiography unit at RSGM Soelastri UMS has a radiation exposure of 15 µSv each time.
The Guidance Notes for Dental Practitioners on the Safe Use of X-ray Equipment define standards, namely rating 1 of at least 70%, 2 of no more than 20%, and 3 of no more than 10% [12]. Therefore, based on these standards, panoramic radiographs at RSGM Soelastri UMS still need to be improved. In the studies of Dhillon et al. and Khan et al., it was also found that the quality results of panoramic radiographs were still below the specified standards [17, 18]. This is a challenge to be able to meet the standard. Although the panoramic radiography technique is relatively more comfortable and easier to use, this technique is very sensitive to position errors. Apart from the skill required from the operator when providing information, communication, and education to the patient and when positioning the patient, this technique also requires cooperation between the patient and the operator [21].
The error of not removing the metallic object was the most frequent error in the preparation error, which was 2.72% (Fig. 6). This is similar to the previous study, namely that the total error of not removing the jewellery was only 2.1% of all errors. Metallic jewellery such as earrings, necklaces, and hair clips can cause ghost images, which can appear as fuzzy radiopaque images [25]. Ghost images can cover anatomical details and pathological details or changes [13]. Ghost images formed from foreign bodies can lead to misdiagnosis, such as odontoma superimposition, fracture lines, and maxillary sinus pathology [23]. The operator should give the patient clear instructions to remove metallic objects from the head and neck area to minimise the occurrence of this error, but sometimes even though the operator has given instructions, the patient still does not remove it. Therefore, it is very important that the operator always follow the standard operating procedure (SOP) when taking panoramic radiographs, besides, of course, building cooperation between the patient and the operator.

The results showed that patient positioning errors were more common than preparation errors. Most panoramic units are equipped with a laser beam to facilitate placement of the midsagittal plane, Frankfort plane, and anteroposterior plane of the patient in the focal trough [13]. Anteroposterior plane errors occur when the patient is positioned too far forward or backward [25]. On the radiographs of patients who are too forward, the front teeth will appear blurry, shortened, and narrow. The proximal parts around the premolars and ramus columns will overlap with each other (Fig. 7) [16]. Radiograph images in patients who are too far back will show that the anterior teeth appear enlarged and blurred on panoramic images [17]. Errors in the patient's position in the vertical plane cause the patient's chin to be too low or high [18]. When the patient's chin is too low or high, it will cause the occlusal plane to look too curved or flat [23]. It also causes a flattened occlusal plane, stretched condyles, and loss of sharpness of the maxillary incisors (Fig. 8) [17]. Incorrect position of the patient's chin, when placed too low, causes the mandibular incisors to look blurred. The amount of detail on the roots of the anterior teeth is also reduced. The mandibular condyle is not visible on the radiograph. There is an “exaggerated smile line” or an image that is curved upwards on the radiograph (Fig. 9) [1].

Not placing the tongue on the palate is the positional error with the highest frequency, as shown in Fig. (10). More than half, or as many as 155 (60.31%), of all radiographs experience this error. The consequence of this error is the superimposition of the air image under the tongue at the apical level of the maxillary teeth [26]. On the radiograph, a radiolucent band will appear around the maxillary teeth so that it can reduce the quality of the diagnosis of the tooth roots and surrounding structures. When the tongue is not positioned to touch the palate, radiolucent areas can obscure lesions in the maxillary anterior teeth [23]. This error often occurs due to patients who find it difficult or confusing when ordered to raise their tongues to the palate [25]. Another explanation is that the patient usually misunderstands the instructions and only puts the tip of his tongue on the palate, or the patient simply does not pay close attention to the instructions given by the operator [27]. This error is difficult for the operator to control because, despite careful instructions, patients do not always place their tongues in the correct position [21]. Quite a few studies have shown similarities with the research results of this study, which show misplacement of the tongue is the most common positional error [21, 25, 27, 28].


The research by Bissoon et al. and Khator is different from this study; the position error that is often encountered is the rotation of the patient's head [26, 29]. In this study, the patient's head errors were asymmetrical and ranked third with the highest frequency of positional errors, namely 112 or 43.58% of all radiographs. An example of an asymmetrical patient head position error is shown in Fig. (11). This error will show uneven enlargement on one side and abnormal height and width of the condyle [18]. Rotation of the head causes a discrepancy in the horizontal enlargement of the integral structure and affects the interpretation of the diagnosis [23]. The patient may have been positioned straight by the operator, but when the machine starts moving, the patient may turn his head to see what is happening, as shown in Fig. (12) [21]. The operator must explain to the patient the procedure for taking radiographs that will be carried out [1]. The purpose and type of equipment to be used for image capture must be carefully explained to the patient [16]. It is even better to demonstrate the movement of the machine to the patient while explaining the need to remain still during the procedure. This is especially important for children who may be anxious. Children need to be instructed to look ahead and not follow tube head movements with their eyes [13].

The second sequence of errors most often found in the study is the patient's position, which is not upright (Fig. 13). A total of 139 radiographs, or 54.09% of all radiographs, experienced this error. This is similar to previous studies, which found that patient posture errors are the second most common error after not placing the tongue on the roof of the mouth, often found on panoramic radiographs [17, 18]. This error causes the appearance of a superimposed cervical spine in the middle of a panoramic radiograph film [18]. There was a tendency for patients to bend over when holding the handle of the machine. Therefore, the operator must ensure that before taking the radiograph, the patient's neck and back are straight [17].
The operator must pay attention to the preparation and positioning of the patient. The higher frequency of errors in preparation and positioning on panoramic radiographs indicates a bigger problem than we think. This also raises questions about the standard of training for operators [18]. Operator skills, better communication with patients, and giving patients time to position themselves can reduce the number of errors and produce high-quality panoramic radiographs. They can also reduce unwanted radiation exposure to patients [29].
CONCLUSION
In conclusion, the quality of panoramic radiographs at RSGM Soelastri UMS was rated “Excellent” at 17.63%, “Diagnostically Acceptable” at 55.45%, and “Diagnostically Acceptable” at 26.92% from January to December 2021. Out of 257 panoramic radiographs with ratings 2 and 3, errors were still found, which were divided into preparation errors of 1.22% and patient position errors of 98.78%.
LIST OF ABBREVIATION
| NRPB | = National Radiological Protection Board |
| SMV | = Submento-vertex |
| RSGM | = Rumah Sakit Gigi Mulut |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The research ethical clearance test was obtained from the Health Research Ethics Commission (KEPK) at RSUD Dr. Moewardi, with letter number 478/IV/HREC/2022.
HUMAN AND ANIMAL RIGHTS
This research did not involve the use of animals. All research procedures conducted on human participants were carried out in strict accordance with the ethical standards set by the responsible committee for human experimentation, both at the institutional and national levels, with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
FUNDING
The present study received financial support from Hibah Integrasi Tri Dharma Perguruan Tinggi (HIT) Universitas Muhammadiyah Surakarta (Agreement Contract No. 605/A.3-III/FKG/VIII/2022).
CONFLICT OF INTEREST
The authors have disclosed that they have no conflicts of interest to declare.
ACKNOWLEDGEMENTS
Declared none.


