All published articles of this journal are available on ScienceDirect.
Necessity of Antibiotic usage after Simple Tooth Extraction in Patient with Healthy Systemic Condition in Herat, Afghanistan
Abstract
Background/Purpose:
Over-intake of antibiotics like amoxicillin, penicillin, ceftriaxone, gentamycin, ampiclox, metronidazole and last but not least, tetracycline is a practical hazard in aid-supported settings such as Afghanistan where not only one can get access to them easily, but also they are generously being prescribed without consideration for necessity or side effects. Prescribing antibiotics after simple tooth extraction has remained a questionable topic in dental academia, especially in the third world countries. Among dental procedures, extraction is the most common procedure for the prescription of antibiotics. This study is aimed to determine the necessity of using antibiotics after simple tooth extraction in people with a normal systemic condition and establish its role in reducing pain and discomfort, swelling, and dry socket.
Materials and Methods:
This double-blinded RCT study was performed in two dental surgeries; Erfan Specialized Dental Clinic and Mena Oral and Dental Care Centre. In all 237 patients, selected systematically, randomized, tooth extraction was performed following the same protocols and materials before and after tooth extraction. Two types of prescriptions (one with antibiotics and one without antibiotics) were prepared in a box. After tooth extraction participants were asked to pick one prescription by chance. All data were collected and analyzed with the SPSS-25 program.
Results:
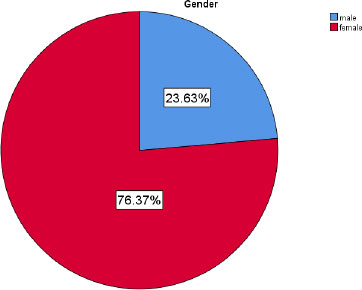
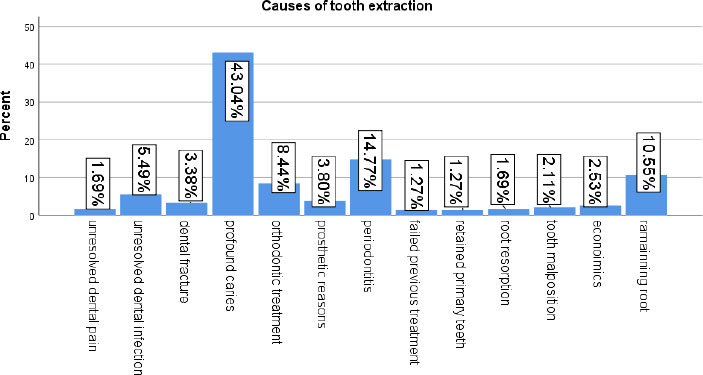
Among all participants 76.37% were female and 23.63% were male. Regarding reasons that led to tooth extraction, 43.04% of teeth were extracted due to profound caries, making it the most common reason followed by periodontitis 14.77% and root remnants 10.55%. Pain and discomfort peaked in the first 10 hours after extraction and gradually decreased up to 48 hours after extraction.
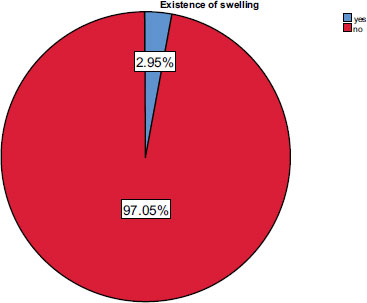
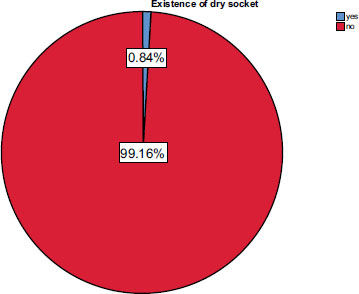
Swelling was observed 2.53% more in antibiotic users than 0.42% in those that didn’t take them and the p-value was significant <0.05. There is no obvious difference between antibiotic usage and dry socket formation, and the p-value was not significant (>0.05).
Conclusion:
Antibiotics are not necessary after simple tooth extractions in patients with a normal systemic condition, even in countries like Afghanistan where patients overuse antibiotics, nor do they have any role in reducing pain, swelling, and dry socket after simple extractions.
1. INTRODUCTION
The oral cavity has one of the most different spectrums of bacterial flora within the body; when left unchecked, it can contribute to local and systemic diseases. The potential for the advancement of devastating infections has made antibiotics one of dentistry's most commonly used drugs [1]. Since the discovery of penicillin, the use of antibiotics among medical and dental professionals has increased tremendously [2]. However, with the overuse of penicillin, its effectiveness has decreased as the bacteria began to develop various resistance mechanisms. Bacterial resistance is considered a major concern in healthcare organizations [3], which refers to the ability of bacteria to survive in the presence of the antibiotic intended to kill them or stop them from multiplying. This type of resistance is facilitated and accelerated by the use and abuse of antibiotics. Any use, no matter how small and appropriate, can encourage resistance. Infections such as tuberculosis, pneumonia, and gonorrhea, as well as many foodborne diseases, are becoming increasingly difficult to treat due to resistant bacteria, leading to increased mortality, high hospital costs, and extended hospital stays. In addition, no new class of antibiotics to combat these infections has been discovered since the late 1980s. The problem is exacerbated when inappropriate use occurs, for example, when antibiotics can be purchased over the counter and/or when healthcare providers improperly prescribe them due to a lack of standard treatment guidelines [4]. It is estimated that antimicrobial resistance (AMR) causes 700,000 deaths worldwide each year. Europe has an estimated 4 million antibiotic-resistant infections, with 37,000 deaths and an economic impact of EUR 1.5 billion annually. The US has reported 2 million antibiotic-resistant infections with 50,000 deaths and $20 billion in healthcare spending each year. In addition, it has been estimated that deaths caused by AMR bacteria could reach 10 million per year worldwide by 2050. The importance of rational antibiotic prescribing is critical to contrasting the AMR phenomenon with its economic and negative impact on healthcare systems. In some cases, antibiotics can be avoided without clinical complications. In addition, antibiotics can cause side effects such as toxicity, allergic reactions, and adverse drug interactions [5].
In dentistry, antibiotics can be used for treatment or prophylaxis; Antibiotic therapy assumes the presence of bacterial infection, even if there are no clinical signs or symptoms of infection, and the duration of treatment should be longer. Antibiotic prophylaxis is generally recommended in the absence of infection to prevent the risk of local or disseminated infection. Disseminated infections may arise from bacterial penetration through incisions or wounds to the bloodstream, causing an infection in a distant organ or sepsis. Some groups of patients are more prone to this eventuality, and antibiotic prophylaxis is highly recommended for them. Antibiotic therapy or antibiotic prophylaxis protocols can include the use of antibiotics before, during, and after surgery based on specific treatment plans linked to factors related to the patient’s systemic health status and type of surgery [5].
Dental practitioners in the United States prescribe 10% of outpatient antibiotics, or 24.5 million prescriptions annually [6]. Their use is not always linked to real indications and needs [5]. Tooth extraction is the most common surgical and dental procedure, and most of the antibiotics used in dentistry are prescribed after tooth extraction [7].
Immoderation in the use of antibiotics is a practical hazard in aid-supported settings such as Afghanistan and can be related to the excessive incidence of antibiotic resistance there. Rates of antibiotic prescriptions for outpatients in a district health center in Afghanistan had been exaggerated, double the WHO advice of 30% [8].
Prescribing antibiotics after simple tooth extraction has remained a questionable topic in dental academia. Antibiotics boost postoperative comfort following dental extraction by preventing wound infection and pain. Although bacteremia certainly happens during simple exodontia, it also occurs in many other common dental procedures for which antibiotic therapy is not justified. This is because the body’s host response is more than sufficient to counter this level of bacteremia [1]. In Afghanistan, among dental procedures tooth extraction is the most common procedure where most of the antibiotics used are prescribed and when this ideology is challenged in regard to the research done in other parts of the world, this challenge is faced with the argument that patients in Afghanistan always use Antibiotics either prescribed or self-medicated so in order to get good results it is recommended that they must be used in Afghanistan even after simple extractions. Unfortunately, none of these arguments are backed up by any research but merely by the pressure of patient demand in these parts of the world who have an erroneous concept of doctors and dentists to be more competent if they prescribe more medication unaware of its diverse effects on their bodies.
Therefore, this study is aimed to determine the necessity of using antibiotics after simple tooth extraction in people with a normal systemic condition and to prove that even in countries like Afghanistan where antibiotics are over-prescribed by practitioners or self-medicated by patients due to their availability over the counter they are not required. This study compares patients post-extraction symptoms with and without antibiotic use.
2. MATERIALS AND METHODS
In this research, 237 patients were selected through systematic randomization from two different dental surgeries clinics, Erfan Specialized Dental Clinic and Mena Oral and Dental Care Centre in a standard surgery setting. This sample size was selected based on the number of patients that were treated for extraction in the duration of 3 months prior to the beginning of trials in both surgeries, which gave an idea and randomized selection of how many patients can be treated here for the 3 months of trials by these surgeries. In Erfan Specialized Dental Clinic, Dr. Ozair Erfan and in Mena Oral and Dental Care Centtre Dr.Manizha Khan was responsible for random allocation sequence, enrollment of participants, taking consents, followups and record keeping.
The trials started in August 2022 and ended in October 2022 for a period of 3 months. The study design was parallel, and the steps were according to that. To minimize error, both researchers followed strict protocols for sampling, procedure, and record keeping and the participants selected were through allocation concealment and the tool used was closed envelopes.
Inclusion criteria comprised patients of both genders above the age of 17, with an education level of at least primary school, healthy otherwise and requiring simple extraction of permanent teeth in a single setting without any flap or surgical intervention and didn’t take any antibiotics prior to extraction. Patients who suffered from systemic diseases or compromised immunity required complicated extractions with open flap, took antibiotics up to 3 days before extraction and/or were pregnant patients were excluded. The patients didn’t comply with the criteria or didn’t comply with the rules after extraction were removed from the trials. Criteria of exclusion from the trial after the extraction were in the ability of the patient to provide the required data correctly and taking other medications besides the one allotted to them. Initially, education was not considered as inclusion criterion, but when the trials began, it was noted that illiterate patients were not able to fill the forms correctly, so they were excluded and having education of at least primary level was added as inclusion criteria. Moreover, initially, all third molars were excluded from the included teeth but when the trials began, third molars for simple extractions were included because the vast majority of teeth for simple extractions were third molars.
The criteria for tooth extraction were set and recorded for each patient as the reason and clinical findings of the tooth at the time of extraction in their files. This criterion included extensive decay, mobile teeth due to progressed periodontitis, fracture due to trauma or otherwise, retained primary teeth, root remnants, orthodontics, wisdom tooth, making removable dentures and teeth which could be saved by root canal therapy but the patient couldn’t afford it and insisted on extraction. At the end of the experiment, the tooth extracted based on the reason was calculated by SPSS.
The procedure initially began by considering inclusion criteria and the eligibility of the study subjects was assessed, then the participants were recruited into the study after consent. Patients were informed in detail about randomized sampling, and written consent was obtained and forms were signed. Prior to the beginning of the research agreement of the Ethical Committee of Herat University, Herat, Afghanistan was obtained by protocol number 07-24102022. Systemic randomization closed envelope double-blinded technique was used where two types of prescriptions were prepared beforehand, dividing participants into groups A and B. Allocation was either to test drug arm or control arm.
All medications used were from the same brand. (Group A) prescriptions included:
1. Amoxicillin capsule (GSK, Pakistan) 500 mg TID n=20
2. Ibuprofen tablet (Brufen, Abbott Laboratories, Pakistan, LTD) 600 mg BID n=10
3. Chlorhexidine solution 0.2% (Protect Mouthwash with Fluoride 110ml, Pakistan) BID n=1.
Prescription for (Group B) encompassed:
1. Ibuprofen tablet (Brufen, Abbott Laboratories, Pakistan, LTD) 600 mg BID n=10
2. Chlorhexidine solution 0.2% (Protect Mouthwash with Fluoride 110ml, Pakistan) BID n=1
Participants were asked to pick one prescription by chance from the box. Information regarding the patient’s condition post-extraction was recorded in a questionnaire by the patient and collected from them promptly. It was ensured beforehand that the patient understands the questionnaire and can complete it on h/her own. Information on the questionnaire recorded patients’ pain and discomfort after 2, 6, 12, 24, 48, and 72 hours of extraction. Patients were called in for a follow-up check-up after seven days to evaluate the site of extraction and record information for any signs of edema, infection, and dry socket.
To contain the same standard of extraction, all researchers followed the same procedure, and the same brand of anesthetic drug (Medicine Inj, 2% Lidocaine with Epinephrine 1/100,000 HSC Co.Ltd, Korea) was used as a local anesthetic. Before extraction, Chlorhexidine, 2.0% mouthwash, was used by patients for 30 seconds. Extraction forceps and elevators were only used.
All the gathered information from the questionnaires was added to SPSS 0.25 software, and results were obtained.
3. RESULTS
3.1. Participants
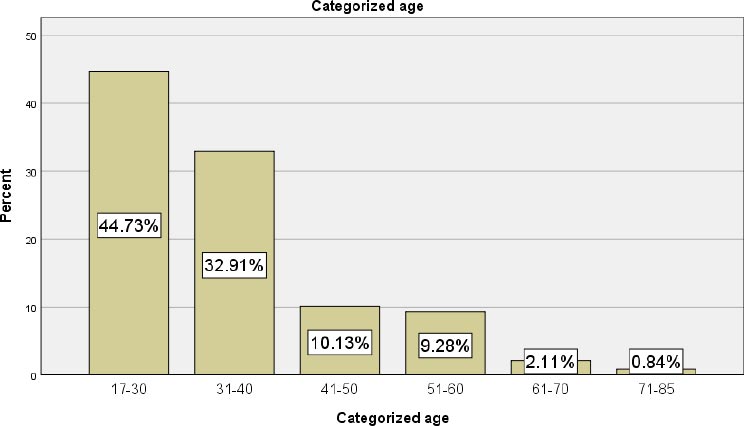
Two hundred thirty-seven participants were included in this study. Among them, 23.63% were male and 76.37% were female (Fig. 1). According to age, all participants in this study were categorized and divided into six groups. 44.73% were between 17-30 years, 32.91% were 31-40 years, 10.13% were 41-50 years, 9.28% were 51-60 years, 2.11% were 61-70, and 0.84% were between 71-85 years old (Fig. 2). We had to exclude the patients who self-administered over-the-counter antibiotics and patients who did not cooperate with us to continue the research. The period of trials was from August 2022 to October 20222. The trial ended when we completed the sample size and the study goals.
3.2. Educational Level among all Participants
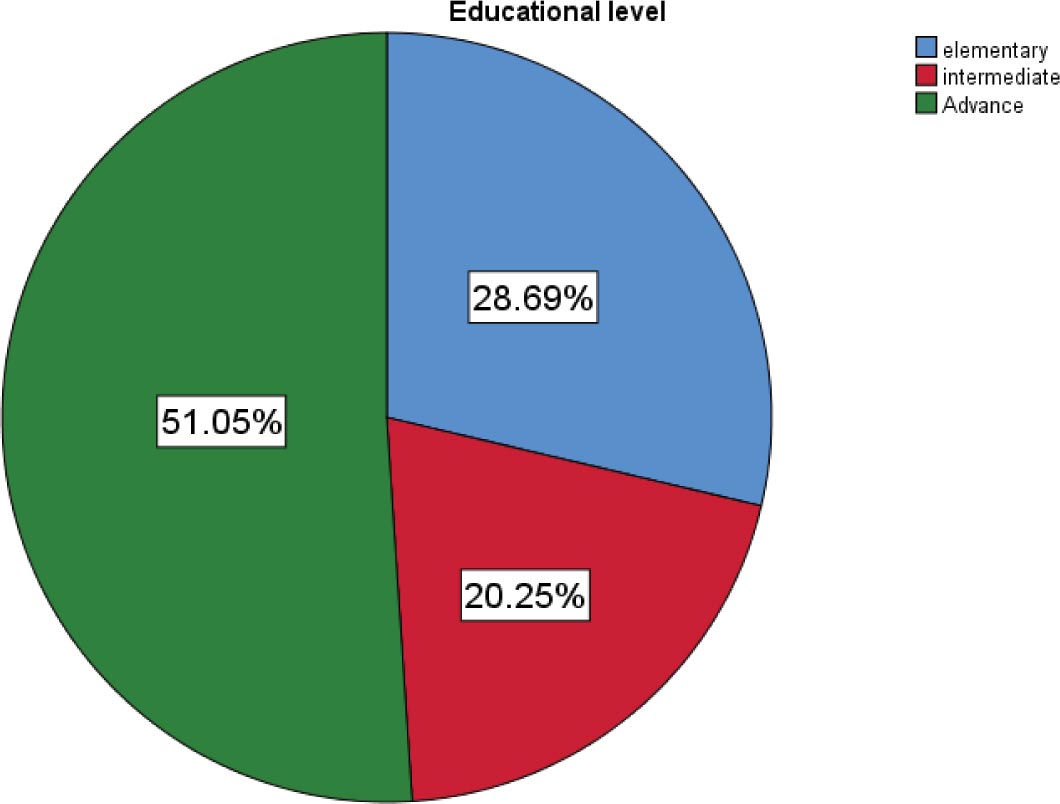
Educational level of all 237 participants 51.05% were advanced, 20.25% intermediate, and 28.69% were at the elementary level (Fig. 3).
3.3. Distribution of Extractions Performed in Dental Surgeries
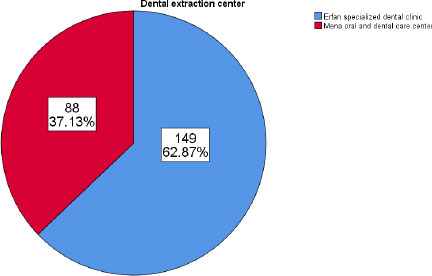
Among all 237 participants, 62.87% were extracted in Erfan Specialized Dental Clinic, and 37.13% were extracted in the Mena Oral and Dental Care Centre (Fig. 4).
3.4. Reasons for Tooth Extraction
In relation to the reasons for tooth extraction, most teeth were extracted due to profound caries 43.04% some due to periodontitis 14.77% and the least percentage of 10.55% due to the presence of the remaining root (Fig. 5) .
Comparing age to cause of tooth extraction, most of the elderly participants who extracted their teeth were suffering from periodontitis, and the p-value was significant (<0.05) but comparing gender and cause of tooth extraction, most of the participants who extracted their teeth for orthodontic reasons were female, and the p-value was significant (<0.05).
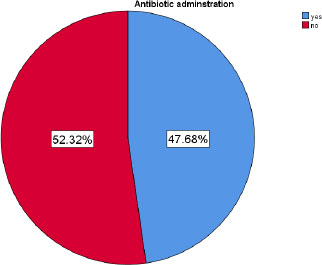
3.6. Antibiotic Administration
Among all 237 patients, 47.68% used antibiotics, and 52.32% didn’t use antibiotics after simple tooth extraction (Fig. 6).
3.7. Existence of Swelling After Extraction
In relation to the existence of swelling after tooth extraction, only 2.95% of all the participants exhibited signs of swelling. In 97.05% of them, no evidence of swelling after the tooth extraction period was noted (Fig. 7).
3.8. Dry Socket Existence
Among all 237 participants, just 0.84% had some evidence of dry socket, and most of them, 99.16%, had no signs or symptoms of dry socket existence (Fig. 8).
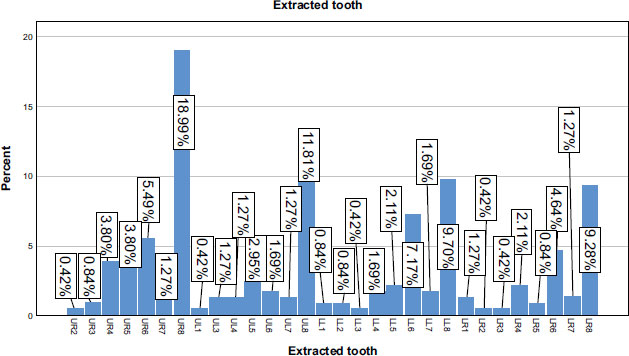
3.9. Extracted Tooth
Based on the type of extracted teeth, the teeth that were frequently extracted were the upper right wisdom tooth 18.99%, then the upper left wisdom tooth 11.88%, the lower left wisdom 9.70%, and the lower right wisdom 9.28%, respectively (Fig. 9).
| Gender | Educational Level | Categorized Age | |||
|---|---|---|---|---|---|
| Male | 56 | Elementary | 68 | 17-30 | 106 |
| Female | 181 | Intermediate | 48 | 31-40 | 78 |
| Total | 237 | Advance | 121 | 41-50 | 24 |
| System | 1 | Total | 237 | 51-60 | 22 |
| - | - | - | - | 71-85 | 2 |
| - | - | - | - | Total | 237 |
| - | - | - | - | System | 1 |
| - | Value | Asymptotic Significance (2-sided) | Exact Sig. (2-sided) | Exact Sig. (1-sided) |
|---|---|---|---|---|
| Pearson Chi-Square | 4.183a | .041 | - | - |
| Continuity Correctionb | 2.759 | .097 | - | - |
| Likelihood Ratio | 4.566 | .033 | - | - |
| Fisher's Exact Test | - | - | .056 | .046 |
| Linear-by-Linear Association | 4.165 | .041 | - | - |
| N of Valid Cases | 237 | - | - | - |
| - | Value | Asymptotic Significance (2-sided) | Exact Sig. (2-sided) | Exact Sig. (1-sided) |
|---|---|---|---|---|
| Pearson Chi-Square | 2.213a | .137 | - | - |
| Continuity Correctionb | .604 | .437 | - | - |
| Likelihood Ratio | 2.981 | .084 | - | - |
| Fisher's Exact Test | - | - | .226 | .226 |
| Linear-by-Linear Association | 2.204 | .138 | - | - |
| N of Valid Cases | 237 | - | - | - |
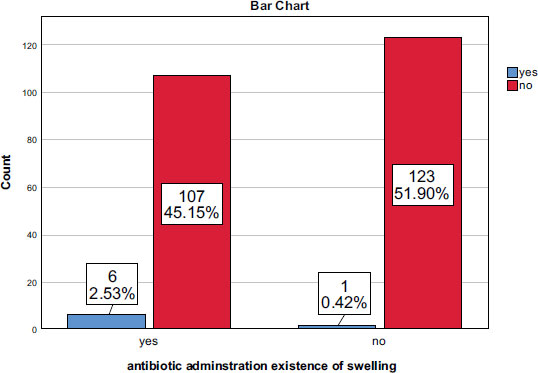
3.10. Antibiotic usage and the Existence of Swelling
Crosstabulation between usage of antibiotics and swelling shows that most antibiotic intake cases had swelling (2.53%) more than non-antibiotic intake cases (0.42%) (Fig. 10) and the p-value was significant (<0.05) (Table 1).
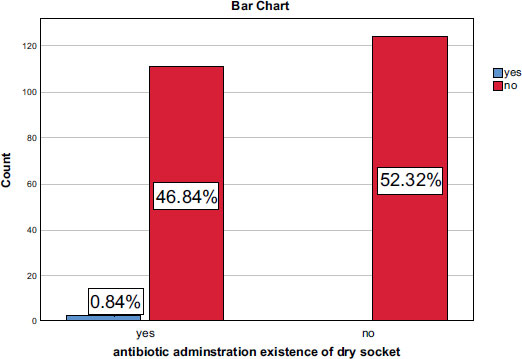
3.11. Antibiotic usage and the Existence of a Dry Socket
The Crosstabulation between the usage of antibiotics and dry socket formation shows that there is no obvious difference between antibiotic usage and dry socket formation (Fig. 11) and the p-value was not significant (Table 2) (>0.05).
3.12. Antibiotic usage and Overall Pain and Discomfort
In relation to antibiotic administration and overall pain and discomfort, there is no significant difference between antibiotic usage or non-usage to decrease pain and discomfort after simple tooth extraction.
3.13. Gender
In relation to gender and swelling formation after simple tooth extraction, there is no significant difference. In addition, in relation to gender and dry socket formation, the finding did not show any significant difference. In relation to gender and reason for tooth extraction According to gender and cause of tooth extraction, most of the participants who extracted their teeth for orthodontic reasons were female, and the p-value was significant (Table 3) (<0.05). According to gender and overall pain and discomfort, the difference was not significant.
3.14. Educational Level
In relation to education, the results showed no significant relationship between educational level of the participants and dry socket and swelling formation after simple tooth extraction. But in relation to education and the cause of tooth extraction, the finding shows significant relation. Most of the participants who extracted their teeth due to their economic situation were from elementary educational level, and the p-value was significant (Table 4) (<0.05). The most cause of tooth extraction was profound caries, periodontitis, prosthetic reasons and remaining roots. So, participants with lower education levels had more unsolved and chronic dental problems, leading to extraction.
3.15. Pain and Discomfort
Pain and discomfort peak in the first 10 hours after extraction and gradually decreases up to 48 hours after tooth extraction (Fig. 12).
According to age and cause of tooth extraction, most of the elderly participant's which extracted their teeth were periodontitis, and the p-value was significant (Table 5) (<0.05).
We had no unintended effects or important harms for any group in the study (Table 6).
| - | Value | Asymptotic Significance (2-sided) |
|---|---|---|
| Pearson Chi-Square | 24.921a | .015 |
| Likelihood Ratio | 29.218 | .004 |
| Linear-by-Linear Association | 4.152 | .042 |
| N of Valid Cases | 237 | - |
| - | Value | Asymptotic Significance (2-sided) |
|---|---|---|
| Pearson Chi-Square | 75.202a | .000 |
| Likelihood Ratio | 69.924 | .000 |
| Linear-by-Linear Association | .001 | .978 |
| N of Valid Cases | 237 | - |
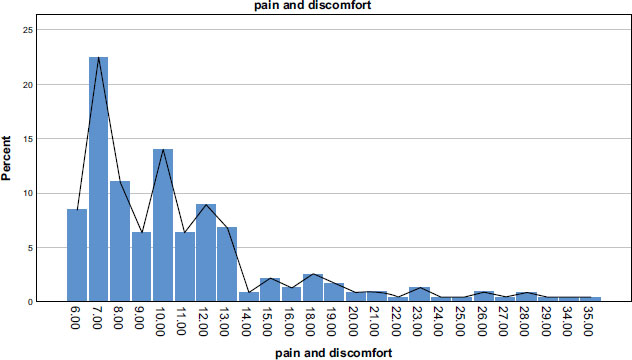
Table 6.
| - | Value | Asymptotic Significance (2-sided) |
|---|---|---|
| Pearson Chi-Square | 128.349a | .000 |
| Likelihood Ratio | 115.147 | .000 |
| Linear-by-Linear Association | .149 | .700 |
| N of Valid Cases | 237 | - |
4. DISCUSSION
The research concluded that among all 237 participants, just 0.84% had some evidence of dry socket. The result obtained from this study is approximately similar to the other countries' research results. In a study done by Momeni H et al. [9], in Iran, the incidence of dry sockets was 0.6%. The same result was reported by Abushaheen et al. [3]. In another study performed by Akinbami BO, Godspower T [10], overall incidence of dry socket was 1.4%.
A study evaluating the efficacy of antibiotics in preventing post-extraction complications in a Chinese population, which was performed on 207 patients between the ages of 18-45, revealed no significant difference between antibiotic usage and dry socket formation [11]. This was consistent with results from Cairo research [1] which did not find a statistically significant difference between antibiotic usage and dry socket formation. This study revealed the same results. In addition, according to gender and dry socket formation, the finding did not show any significant difference. These findings were consistent with the results of many other researches that took place in Iran [9] and Palestine [12] which are similar areas as Afghanistan, which stated that although the prevalence of dry socket in females are more than in males, but did not show any statistically significant differences.
In this study, the findings showed that the existence of swelling after tooth extraction among all participants was 2.95%. Regarding antibiotic usage and the existence of swelling, in this study statistically significant difference was found between the antibiotic group and the non-antibiotic group. The result shows that most antibiotic intake cases had more swelling (2.53%) than non-antibiotic intake (0.42%). This finding contradicts the results of previous studies, such as studies conducted by Xu H, Chao J [11]. and Agrawal M [13], who reported no significant relationship between the use of antibiotics and swelling.
Pain and discomfort peaked in the first 10 hours after extraction and gradually decreased up to 48 hours after tooth extraction. There is no obvious difference between antibiotic usage and overall pain and discomfort in this study, similar to other studies [11, 13], which noted that antibiotics did not show a statistically significant beneficial effect in reducing pain and discomfort.
Most teeth were extracted due to profound caries (43.04%) in the present study. This was followed by periodontal diseases, which accounted for (14.77%) of extractions. These findings are in agreement with numerous other studies, such as those done in Taiwan [14], Palestine [12], Pakistan [15], and Cairo [1]. Conversely, this study findings were in contrast to a study done by Akinbami BO, Godspower T [10], who reported that acute apical periodontitis was the commonest reason for extraction leading to the extraction of 604 (44.4%). This was followed by irreversible pulpitis, which led to 162 (11.9%) extractions.
This study has some limitations. First, to minimize error, we had to do the research in only two centers to follow the same protocols and materials before and after tooth extraction. Second, some patients self-administered over-the-counter antibiotics and we had to exclude them from the study. Third, a number of patients did not cooperate with us to continue the research.
CONCLUSION
In conclusion, antibiotics did not show a statistically significant beneficial effect in reducing pain, swelling, and dry socket after simple extractions in patients with a normal systemic condition. Antibiotics can cause adverse effects such as antibiotic-resistant, toxicity, allergic reactions, and negative interactions with other drugs. Rational prescription of antibiotics is crucial to contrast the antibiotic resistance phenomenon with its economic implications and negative impacts on healthcare systems.
SUGGESTIONS
The authors suggest that in view of the results of this experiment and similar other experiments done in neighboring countries, antibiotics should only be prescribed in cases where the dry socket is observed among patients after a simple extraction. Patients must be advised about the prevention of dry sockets and must be provided with an informatory leaflet before leaving the surgery. We also suggest that in countries like Afghanistan awareness must be raised for this issue not only to patients but also among dentists that in cases of inflammation, anti-inflammatory drugs are a better choice and overuse and prescription of antibiotics must be prevented.
LIST OF ABBREVIATIONS
| AMR | = Antimicrobial Resistance |
| WHO | = World Health Organization |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This research was conducted after the agreement of the Ethical Committee of Herat University, Herat, Afghanistan, was obtained by protocol number 07-24102022.
HUMAN AND ANIMAL RIGHTS
No animals were used that are the basis of this study. We confirm that the reported experiments are in accordance with the Helsinki Declaration of 1975, as revised in 2013 (http://ethics.iit.edu/ecodes/node/3931).
CONSENT FOR PUBLICATION
Informed consent was obtained from all the participants.
AVAILABILITY OF DATA AND MATERIAL
All data and materials are available to the authors https://doctor-6205.business.site/ozairerfan@yahoo.com.
FUNDING
None.
STANDARDS OF REPORTING
CONSORT guidelines were followed in this study.
CONFLICT OF INTEREST
The authors declare no conflict of interest with respective to the research and publication of this article.
ACKNOWLEDGEMENTS
Declared none.
SUPPLEMENTARY MATERIAL
CONSORT flow chart is available as supplementary material on the publisher’s website along with the published article.


