All published articles of this journal are available on ScienceDirect.
Fracture Resistance and Failure Mode of Endocrown Restorations with Different Remaining Walls and Finish Lines
Abstract
Objective:
Endocrown is a conservative treatment plan for endodontically treated teeth. The aim of this study was to evaluate the fracture resistance of four different preparation designs of endocrown restorations in mandibular molars.
Methods:
Thirty-six endodontically treated molars were divided into two groups (L, MD). In group L, the lingual wall and in group MD, mesial and distal walls were removed up to 1 mm above the CEJ. For each group, 2 subgroups (n=9) were considered: B) 2mm occlusal reduction with but joint finish line, S) axial reduction with radial shoulder finish line, in addition to 2mm occlusal reduction. Digital impression was performed, followed by designing and milling the lithium disilicate blocks. After cementation of the restorations and thermocycling, fracture resistance and failure mode were investigated.
Results:
Groups LB and LS, showed significantly higher fracture resistance compared to groups MDB and MDS (P=0.02). However, the type of finish line did not have a significant effect on the fracture resistance in the experimented groups (P=0.232).
Conclusion:
Unlike the finish line type, the number of remaining axial walls had a significant effect on fracture resistance. Although most of the fractures were catastrophic, they occurred due to forces much greater than usual.
1. INTRODUCTION
Endodontically treated teeth (ETT) are more susceptible to fracture due to a lack of structural durability and dehydration [1]. The amount of remaining tooth structure plays a significant role in the strength of these teeth after rehabilitation [2, 3]. By evolution of adhesive dentistry, endocrowns have become a vital treatment option for ETT compared to post-core crowns with acceptable long-term outcomes [4, 5]. However, considering less extension of preparation, preservation of tooth structure and elimination of the need for crown lengthening, endocrowns are a more conservative treatment option. The most common ceramic for restoring ETT with endocrown is Lithium disilicate glass-ceramic due to its mechanical properties and etching ability [6]. Different designs have been presented for axial walls to increase the retention and resistance form. Alamin et al. reported no significant difference between deep chamfer and butt-joint margins in terms of fracture resistance [7]; Einhorn et al.’s study revealed the same results [8]. On the other hand, Taha et al. revealed higher fracture resistance in groups with ferrule rather that butt-joint margin [1]. Also, there is little information about the effect of endocrown design on the biomechanical properties of ETT. Therefore, the aim of this study was to evaluate and compare the fracture resistance of 4 different designs of endocrown restoration in mandibular molar teeth. The null hypothesis was that neither the number of remaining axial walls nor the type of finish line would influence the fracture resistance of the endocrown restorations.
2. MATERIALS AND METHODS
This study was approved by an ethical committee of the Dental Faculty, Azad University, Tehran, Iran (IR.IAU.TMU.REC.1399.181). The sample size was calculated for a significance level of α = 0.05 and power of 0.8 (n=9 in each group). In this experimental in vitro study, 36 sound human mandibular molars (with completely formed apices, without caries in the cervical region and also without cracks which were confirmed by 2.5× magnification dental loupes) were included. The mesiodistal, occlusocervical and buccolingual dimensions of selected teeth were measured by a digital caliper (500 series Mitutoyo, Tokyo, Japan) and only the teeth within 1 mm of the mean size were included. The teeth were kept at room temperature in a solution containing 0.1% thymol (Caelo, Hilden, Germany). After cleaning the teeth with water and pumice powder and also a dental ultrasonic scaler, they were stored in distilled water throughout the study. Endodontic treatment was performed by the same practitioner based on a similar sequence. Root canals were prepared with rotary files (SP1 V-Taper, China), and rinsed with 1% sodium hypochlorite. Finally, rinsing with 5 ml of 17% EDTA and 5 ml NaOCl 1% was performed. The root canals were dried with paper cones (Diadent, Seoul, Korea) and filled with gutta-percha/AH26 sealer (De Trey Dentsply, Kontanz, Germany) using the lateral condensation method. The gutta-percha at the orifice of the canals was removed and compacted with a hot plunger in the vertical direction. The access cavity was temporarily filled and the specimens were stored in 100% humidity at 37 °C for 1 week. A thin layer of latex powder approximately 0.3 mm thick was coated around the roots to simulate PDL [9]. The specimens were mounted in resin blocks (PMMA, Acropars 200, Iran), using a dental surveyor parallel to the long axis, so that the resin surface was about 3 mm below the CEJ. To standardize the preparation, a custom-made device was attached to the surveyor in order to hold the rotary instrument, so that the bur was perpendicular to the horizon. The desired angle for axial preparation was adjusted on the surveying table (IMPLA, Schutz Dental Group, Germany) and the specimens were rotated on the table until the axial walls were prepared with a similar taper. The occlusal surface was reduced 2mm and a round-end tapered diamond bur (80 µm grit, SBR 5 smooth cut, GC, Tokyo, Japan) was used to produce an 8-degree taper in the axial walls of the access cavity. The specimens were then randomly divided into 4 groups (n=9 in each, LB, LS, MDB, MDS) (Fig. 1).

In groups LB and LS, the lingual wall was removed up to 1mm above the CEJ. Butt-joint finish line was prepared for group LB and in group LS, axial reduction with 6-degree taper besides a radial shoulder finish line was prepared. In groups MDB and MDS, mesial and distal walls were removed up to 1 mm above the CEJ, and finish line preparation was similar to groups LB and LS. Finishing and polishing were done with a similar bur in shape (Polishing bur, 25 µm grit, SBR5 f smooth cut, GC, Tokyo, Japan) and abrasive disc (Soflex 238 2 C, 2382F, 3M EPSE, St. Paul, USA). Eventually, the pulpal floor was covered with glass ionomer (GC, Tokyo, Japan), keeping a depth of 4mm. After digital impression (Medit i500 Intraoral scanner, Medit, Seoul, Korea), designing (Designing software, Exocad, Amann Girrbach َ, Koblach, Austria) and milling (Milling machine, Motion 2, Amann Girrbach, Koblach, Austria) of the restorations (lithium disilicate, Rosetta SM, Hoss, Gyeonggi-do, Korea) were done (considering 30 µm for cement space). The sitting of the endocrowns was checked by a fit checker (Panasil, Kettenbach, Germany). Endocrowns were cleaned in ultrasonics containing isopropanel alcohol 99% for 3 minutes. Teeth were also cleaned with pumice powder (without fluoride) for 15 seconds and rinsed with water for 15 seconds. Also, surface treatment was performed using 37.5% phosphoric acid (Ultradent, South Jordan, UT, USA). Then, the inner surface of the restorations was etched with 9.5% hydrofluoric acid gel (Ultradent, South Jordan, UT, USA) for 20 seconds, followed by applying silane (Ultradent, South Jordan, UT, USA) for 60 seconds. Cementation was done using Dual Cure resin cement (Rely X Unicem 2 Automix, 3M ESPE, Seefeld, Germany). To ensure a similar standard seating pressure, a 5-kg weight was used to maintain the endocrowns in place during the setting of the cement. After the first 2 seconds, the excess cement was removed from the margins and then they were light-polymerized for 40 seconds with a light-curing (Coltolux LED, Coltène/Whaledent, Cuyahoga Falls, OH, USA) unit set at 600 mW/cm2. The specimens were kept in distilled water at 37°C water for 24 hours, and then, were subjected to 2500 rounds of thermal cycling (Haakew 15, SD Mechatronik, Feldkirchen- Westerham- Germany) between 5°C and 55°C with a dwelling time of 20 seconds. Finally, the samples were subjected to a static compressive loading parallel to the long axis on the central fossa with a crosshead speed of 0.5 mm/min in the universal testing machine (UTM, Zwick Z050, ZwickRoell, GA, USA) by means of a 4-mm steel bar until the failure occurred. The amount of failure force (N) was recorded at the time of fracture. Specimens were evaluated visually to identify the failure mode based on the Burke classification as follows: CL I: Minimal fracture or crack in the crown, CL II: Less than half crown lost, CLIII: Half of the crown displayed or lost, CLIV: More than half of crown lost, CLV: Severe fracture of the tooth and/or crown [10].
3. RESULTS
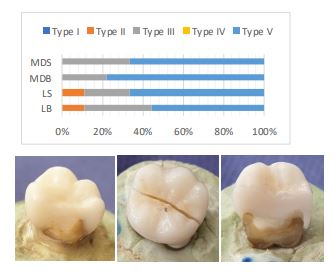
The mean fracture resistance values for tested groups are depicted in Table 1. The lowest values were detected in MDB and MDS groups respectively. On the other hand, lower fracture resistance in the specimens without two axial walls compared to specimens with three remaining walls was statistically significant (P=0.02). However, the type of finish line did not have a statistically significant effect on the fracture resistance in the experimented groups (P=0.232). Furthermore, the interaction of the finish line type and the number of remaining axial walls were insignificant (P=0.687). Based on the Bruke classification, the most failure modes observed within the specimens were type III and V (Fig. 2).
|
Fracture Resistance Groups |
Min. | Max. | Mean | Std. |
|---|---|---|---|---|
| LB | 1287.00 | 3348.00 | 2153.11a | 815.95 |
| LS | 1273.00 | 3925.00 | 2323.11a | 822.43 |
| MDB | 1045.00 | 1573.00 | 1359.88b | 151.02 |
| MDS | 1050.00 | 2651.00 | 1700.44b | 467.28 |
4. DISCUSSION
In this study, the fracture resistance of mandibular molars with 2 or 3 remaining axial walls as well as two types of finish lines (butt-joint or shoulder) were investigated. Regarding the design preparation, the null hypothesis was partially rejected. Unlike the finish line type, the remaining walls had a significant effect on the specimens’ fracture resistance. Due to the advantages of endocrowns (fewer clinical procedures, conservative removal of dentinal tissue, less chairside time, lower laboratory costs, better distribution of masticatory stresses at the tooth-restoration interface, elimination of the need for crown lengthening surgery due to the lack of ferrule, no need to remove root canal filling in teeth with improper root length or shape), they are becoming more popular in treating ETT. Bindle and Mormann reported only one failure out of nineteen endocrowns after twenty-eight months of follow-up due to recurrent caries [11]. Biacchi and Basting reported higher fracture strength for teeth restored with endocrown compared to conventional crowns supported by glass fiber posts and composite core [12]. Although ferulization was not considered in the previous study, it could affect the results. Based on Belleflame et al.’s study, endocrowns revealed a high survival rate (98.8%) during 10 years of follow-up [5]. Also, a recent systematic review showed that the fracture strength of endocrowns restoring posterior teeth was similar to or higher than conventional crowns [4]. In the present study, monolithic lithium disilicate was used which is the choice material in making endocrowns. To investigate the fracture resistance, the force was applied to the occlusal surface perpendicular to the long axis of the specimens, simulating the forces in the molar region. Based on the obtained results, it was observed that specimens with three axial walls had significantly higher fracture resistance than ones with two walls. The amount of residual tooth tissue and its preservation is one of the key factors in the success of restorative treatment; the more remaining tooth structure, the better the biomechanical properties and fracture resistance would be. Tribst et al. examined the effect of residual dental structure on the stress distribution of ETT reconstructed with endocrowns by the FEA method and emphasized the importance of preserving the remaining dental tissue [3]. Arunpraditkul et al. presented higher fracture resistance in premolars with 4 remaining walls rehabilitated with post-core-crown than specimens with 3 residual walls [2]. On the other hand, a greater remaining tooth structure means a further surface for adhesive bonding and better stress distribution in the area of contact between the restoration and the tooth. Also, tooth strength is directly related to the amount of residual tooth tissue which increases retention and crown resistance against rotation [1]. Therefore, the coronal structure of the ETT should be preserved as much as possible.
Based on the results of this study, it was observed that there is no significant difference between groups with butt-joint or shoulder finish lines, which was in line with Alamin et al. study [7]. Einhorn et al. demonstrated higher fracture resistance in specimens with a ferrule, however, failure stress considering the surface area available for adhesion was not different in any study groups [8]. Also, Taha et al. study revealed greater fracture resistance for the shoulder margin than butt-joint in Enamic endocrowns [1]. The result of Ahmed et al.’s study displayed significantly higher fracture resistance considering circumferential ferrule compared to the flat occlusal table for the Lithium disilicate group, while it was not different for the Zirconia group [13]. Biomechanically, compressive loads are distributed and resisted with butt-joint margin and shear forces through the axial wall with shoulder finish line [1]. Although the mean fracture loads in the current study were higher for the cervical shoulder, this difference was not significant which could be due to exerting compressive load along the axial axis of the teeth. Hence, it is recommended to evaluate the results under angled static loading or cyclic loading or follow-up of clinical cases in further studies. However, the mean fracture loads for the test groups were much higher than the maximum chewing force in the molar region [14]. On the other hand, it is noteworthy that a more complex preparation design like adding ferrule would result in more discrepancies in the intaglio surface of endocrown restorations [8, 15].
The survey of failure mode in the specimens demonstrated catastrophic fractures in most of them (type III and V of Burke classification). Although type II fracture was detected only in LB and LS groups, type III and IV were dominant in all groups; the important point was that fractures all occurred due to forces much greater than normal chewing loads. In this study, thermocycling was performed to simulate clinical conditions, although considering cyclic loading and fatigue conditions would simulate it better. On the other hand, oral conditions are a combination of dynamic forces, thermal and chemical procedures acting on the teeth and restorations: therefore, prospective clinical trial studies are the most valuable studies. In addition, investigation of the internal and marginal adaptation of endocrown restoration for each preparation design should be considered.
The specimens in group LB and LS depicted more similar results compared to groups MDB and MDS. It implies that the amount of remaining tooth structure is more influential than the finish line type. In group MD, the specimens with shoulder finish lines displayed more fracture resistance, although it was not significant. Therefore, in case of further destruction, selecting the appropriate finish line would become more important. It is noteworthy that the addition of an axial wall in form of a shoulder finish line would increase the bonding surface, while reducing the remaining tooth structure.
CONCLUSION
Within the limitations of this in vitro study, it was concluded that ETT with 3 remaining coronal walls displayed significantly higher fracture resistance than teeth with only 2 remaining coronal walls. Adding an axial wall with a shoulder finish line to the preparation design, had no significant effect compared to the butt-joint margin. Therefore, preservation of tooth structure is of great importance in the preparation of ETT for endocrown restoration. The butt-joint finish line would be recommended to maintain the coronal structure and achieve the aforementioned goal.
LIST OF ABBREVIATIONS
| ETT | = Endodontically Treated Teeth |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by an ethical committee of the Dental Faculty, Azad University, Tehran, Iran (IR.IAU.TMU.REC.1399.181).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


