All published articles of this journal are available on ScienceDirect.
Behavioral Modification of an Uncooperative Preschool Child with Sickle Beta Thalassemia Disease in a Dental Clinic: A Case Report
Abstract
Background:
Treating medically compromised pediatric patients with dental anxiety can be challenging, especially when general anesthesia and sedation are not an option. This paper reported a case of an uncooperative preschool child who was medically compromised and presented in the dental clinic with Severe-Early-Childhood-Caries (S-ECC). The dental behavior management of such a case was not previously discussed in the literature.
Case Presentation:
This paper explains the dental management and behavior modification carried out for a 5-year-old male child who was diagnosed with sickle beta thalassemia disease (Sβ-thalassemia), S-ECC, had a negative dental behavior, and was successfully and efficiently treated under a dental setting. The patient presented with his mother, who was concerned about her child’s decayed teeth and sought dental treatment as soon as possible to avoid any risk of infection. Dental examination revealed multiple dental caries and high caries risk. The patient’s behavior can be classified as definitely negative with high level of anxiety. The mother showed permissive parenting and the father exerted an authoritative parenting style. Dental management focused mainly on child behavioral modification via utilizing the difference between the parenting styles. Middle way of treatment, the child showed behavioral improvement, which was progressing toward the end of the treatment. Teeth were successfully restored with composite and metal crowns.
Conclusion:
With several behavior management techniques and understanding the parenting styles, the patient's behavior improved, and the treatment plan was successfully used on a dental chair without the need for more advanced management under general anesthesia.
1. INTRODUCTION
Sickle beta thalassemia (Sβ-Thalassemia) is an autosomal recessive condition that affects the hemoglobin that carries oxygen to the body. Affected individuals have a different mutation in each copy of their HbB gene; one gene causes the cells to become sickled and the other is associated with β-thalassemia, a blood disorder that reduces the production of hemoglobin [1]. There is a 1:4 chance of having a child with Sβ-Thalassemia if one of the parents has HbS mutation and the other parent is a carrier of β-thalassemia [2]. The prevalence of Sβ-thalassemia was reported to be less than one-third to zero percent of sickle-cell cases [3, 4].
Clinical features may vary from a sickle cell anemia-like condition to an asymptomatic condition depending on the inherited type of β-thalassemia (βo, β+, β++) [5]. General features include anemia, repeated infections, frequent episodes of a painful crisis of the lumbar spine, femura, ribs, sternum and the abdomen being the most common sites affected, slight enlarged spleen or liver, jaundice, delayed puberty and slowed growth [6]. Factors such as dehydration, acidosis, infections might precipitate sickling crisis [7].
Special precautions should be taken while treating those patients in the dental office to prevent crisis events; therefore, all possible sources of infection should be removed, medications that might cause acidosis such as those containing salicylic acid, some conscious sedation drugs and stress should be avoided [7]. General anesthesia (GA) is considered a risky option in such patients due to the possibility of developing a crisis [8]. Hence, those patients are better managed using non-pharmacological behavior management techniques and nitrous oxide inhalation sedation [7].
Anxiety in the dental clinic is triggered by different factors and is of internal and external origin. Factors such as direct or indirect, previous negative dental or medical experience are considered external [9], while internal factors include those related to the person and his/her personality [10]. Moreover, studies reported that more than 30% to 90% of thalassemia children develop anxiety and other psychological disorders [11-13]. Pediatric dentists should have the skills to modify the child’s behavior efficiently. For this purpose, there is a considerable need to identify factors that positively alter the anxiety state and enhance negative behavior during dental treatment. Applying different non-pharmacological techniques of behavioral management to modify the behavior of an uncooperative child is strongly recommended before choosing more complicated alternatives such as sedation or general anesthesia [10]. Literature looked at the effect of parental presence on child’s behavior during their dental visit. A study by Sabbagh and Sijini carried out on parental separation among Saudi children reported that the main reason for parents preferring parental separation was improving their child’s behavior [14]. The literature lacks the experience of successfully and efficiently dentally treating a child diagnosed with Sβ-thalassemia, Severe-Early-Childhood-Caries (S-ECC), and had a negative dental behavior in a dental setting.
Therefore, the aim of this case report was to explain the dental management and behavior modification carried out for a pre-school child who was diagnosed with Sβ-thalassemia, S-ECC and has a negative behavior at the dental office utilizing different behavioral modification management techniques and without the need for general anesthesia.
By understanding this case report and successfully managing such a case, dentists will be more confident in treating these cases in the future under dental setting and therefore reducing the patient’s risk.
2. CASE PRESENTATION
A 5-year-old male patient was admitted as a new patient at the Pediatric Dentistry clinic, King Abdulaziz University Dental Hospital, with his mother in October 2018. The mother’s chief concern was her child’s decayed teeth, as she was advised by her son’s physician to seek dental treatment as soon as possible to avoid any risk of infection. The child had no concerns or pain related to his teeth.
2.1. Medical History
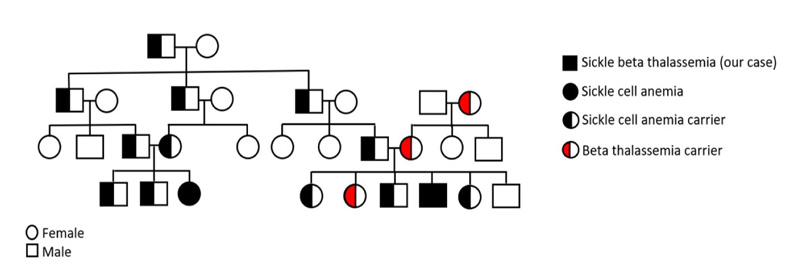
Medical history of the patient revealed sickle beta-thalassemia disease, which was discovered in June 2018 after having an episode of intense recurrent abdominal pain due to stone formation in the gallbladder that necessitated cholecystectomy. The patient was on folic acid tablet 5 mg once a day to control anemia, and oxymethyle penicillin 5 ml twice a day as a prophylaxis antibiotic to protect against infection prescribed by his physician to control the patient’s medical condition. The mother mentioned that her child gets exhausted easily following physical activities. Family medical history showed that the father is a carrier for sickle cell anemia and the mother is a carrier for beta-thalassemia. Four of his five siblings are carriers either of sickle cell anemia or thalassemia as shown in Fig. (1).
2.2. Dental History
The patient had no history of dental pain or abscess and did not have any cold sores. He showed no history of oral habits. The patient did not brush his teeth regularly and his diet was inadequate and needed improvement. Extra-oral examination came in line with the general features of such patients that revealed pale skin, dry lip, and bilaterally palpable cervical lymph nodes. The patient has a slightly convex facial profile with an average mandibular plane angle. Intraoral examination showed slightly pale gingiva and oral mucosa. Oral hygiene was found to be fair (scored between 0.7 and 1.8) according to Green and Vermilion Index [15]. Dental examination revealed occlusal caries on teeth #55, 75, and 85 and proximal caries on teeth #63, 65, 74, and 84 (Fig. 2). The number of carious teeth was more than 6, which is considered severe early childhood caries according to the American Academy of Pediatric Dentistry [16]. The patient had right and left mesial step occlusion.

Radiographic examination was taken following the American Academy of Pediatric Dentistry guidelines [17]. It showed proximal caries on multiple upper and lower posterior teeth including #55, 63, 64, 65, 74, 75, 84, and 85. While some caries lesions were confined to the enamel surfaces, others extended deeper to involve the dentine. However, in all teeth, no periapical pathology was noticed. Based on his medical history, clinical findings, diet, and oral hygiene, the patient was considered high caries risk according to the Caries-risk Assessment Tool (CAT) [17].
2.3. Social History
With regard to the child’s behavior assessment, he was definitely negative according to Frankel’s behavior rating scale [18], and uncooperative defiant behavior according to Wright’s classification [19]. Dental anxiety score was assessed for the patient and his parents before starting the treatment using Modified Dental Anxiety Questionnaire (Table 1). The child's score was high, indicating a high level of anxiety. Various parenting styles are exhibited by each parent where the mother showed a very permissive parenting style, failing to exert control on the undesirable behavior of her child while the father exerts an authoritative parenting style.
2.4. Dental Management
The patient was seen, examined, treated and managed completely by a postgraduate specializing in Pediatric Dentistry. Dental management included prevention via fluoride application, proper oral hygiene instruction, diet advice, and a proper explanation of the possible effect of oral infection on the child’s general health. Caries was restored using composite restorations (class III on 63, class II on 74 and preventive resin restoration on 55, 64, 75 and 85) and preformed metal crowns (on 65 and 84) (Fig. 3).
| Date of visit | Intervention | Behavior | Behavioral technique | Accompanied with |
|---|---|---|---|---|
|
Visit 1 24/10/2018 |
• Medical and dental history. • Intra- and extraoral examination. • Intra- and extraoral photographs. • Impression taking. • Bitewing radiographs. • Oral hygiene instructions. |
--ve -ve --ve --ve -ve --- |
- Positive reinforcement - Tell – Show – Do - Distraction |
Mother |
|
Visit 2 28/10/2018 |
• Local anesthesia + Rubber Dam • Class IV composite #63 • Oral prophylaxis. |
--ve --ve --ve |
- Positive reinforcement - Tell – Show – Do - Distraction |
Mother |
|
Visit 3 3/2/2019 |
• Local anesthesia + Rubber Dam • Stainless steel crown #65 |
--ve --ve |
- Positive reinforcement - Tell – Show – Do - Distraction - Nitrous oxide - Physical restraint - Voice control |
Mother |
|
Visit 4 17/2/2019 |
• Class I composite #55 | -ve | - Positive reinforcement - Tell – Show – Do - Distraction - Physical restraint |
Father |
|
Visit 5 28/11/2019 |
• Class I composite #85 • SSC #84 |
+ve +ve |
- Tell – Show – Do - Positive reinforcement |
Father |
|
Visit 6 3/3/2019 |
• Class I composite #75 • Class II composite #74 • Oral prophylaxis. • Postoperative bitewing radiographs. • Postoperative photographs. |
+ve +ve +ve -ve -ve |
- Positive reinforcement - Tell – Show – Do - Distraction |
Father |
|
Visit 7 10/9/2019 |
• Examination • Fluoride application • Fissure sealant |
+ve +ve +ve |
- Positive reinforcement - Tell – Show – Do - Distraction |
Father |

2.5. Behavior Management
The child’s behavior was definitely negative in the first visit, and with the commencement of the treatment his behavior was extremely negative. The dental and behavior management was primarily carried out by the dentist. The dental assistant helped and supported the dentist by preparing the instruments, N2O and restrain when needed. The dentist started by meeting the child and parents and welcoming them to the clinic. During the first visit, the dentist took the medical, dental and family history; assessment of the child and parents’ behavior and anxiety; and asked about the chief complaint showing the child and parents empathy, compassion, and genuine concern through communication. The child development stage was evaluated to plan for the dentist's communication behavior management. The child fell under the stage of pre-operational according to Piaget [20], thus he thought on a symbolic level rather than using cognitive operations. The child might pretend that his arms were airplane wings or a stick might become a sword [26]. Distraction and tell-show and do were used with terms such as pillow for cotton roll and umbrella for rubber dam. In addition, during the anesthesia, the dentist asked the patient to count from one to ten; then, from ten to one as a means of distraction.
According to Ericssons stages of Psychosocial Development, this age falls under Stage 3, which is initiation vs guilt [21]. In this stage children begin to assert their power and control over the world through directed play and other social interactions. Therefore, the dentist used the positive reinforcement for the child to feel initiative and accomplished.
During the radiograph and clinical examination, the dentist used tell-show-do behavior technique. He also used distraction method especially while carrying out the radiography by talking to him about football and which football team he preferred. Then the dentist discussed the treatment plan, including possible behavior techniques that could be used, risk and benefits for each treatment proposed and subsequently the consent form was signed by the parents. The patient was scheduled for the first appointment and was short (30 minutes).
Nitrous oxide and physical restraints were used after the parent’s consent with no desirable effect. The N2O was named the astronaut equipment and the restrain (papoose) was named the child's special bed with a blanket to keep him warm. By the 4th appointment, the father started to come with his child, together with the continuous use of tell, show, and do in addition to the use of positive reinforcement, distraction, voice control and rewards, the child showed behavioral improvement, which was progressing toward the end of the treatment (Table 1).
Dental Anxiety forms for both parents and the child were filled at their last visit, showing a dramatic reduction of anxiety of both the mother and the child, while the father’s anxiety did not change, as shown in Table 2.
Table 2.
| S.No | Mother’s anxiety | Father’s anxiety | Patient’s anxiety | ||||
|---|---|---|---|---|---|---|---|
| Before | After | Before | After | Before | After | ||
| 1 | Going to visit dentist | 2 | 2 | 1 | 1 | 5 | 2 |
| 2 | Setting in waiting room | 3 | 1 | 1 | 1 | 4 | 2 |
| 3 | Tooth going to be drilled | 4 | 2 | 1 | 1 | 5 | 3 |
| 4 | Tooth going to be polished | 2 | 1 | 1 | 1 | 5 | 3 |
| 5 | Local anesthesia injection | 5 | 2 | 1 | 1 | 5 | 3 |
| Total score of dental anxiety | 16 | 8 | 5 | 5 | 24 | 13 | |
| Level of anxiety: 1 -5 (1: not anxious, 5: extremely anxious) Categories of anxiety < 10: low anxiety | 10-18: moderate anxiety | > 18: High anxiety |
|||||||
2.6. Outcome and Follow-up
The parents continued to have a good and thankful relationship with the pediatric dentist. In addition, the patient had regular outpatient dental care. He received regular fluoride application every 3-months and fissure sealant on all permanent first molars after they were clinically fully erupted, according to the American Academy of Pediatric Dentistry (AAPD) guidelines [17]. Moreover, for the last two years, although the patient continued to present on follow-up visit with fair oral hygiene, he did not develop any new carious lesions. His oral hygiene scored good (0.6) according to Green and Vermilion Index) and dietary intake was improved at the end of the treatment and follow-up visits. Oral hygiene and anticipatory guidance were regularly instructed and reinforced to parents and patients during follow-up visits.
3. DISCUSSION
The child behavior during dental procedures is multifactorial and can be affected by different factors such as the child’s, age, personality characteristics, temperament, cognitive level, fear and anxiety, previous medical experience, and parental dental anxiety [22]. In this specific case, the external factor that influenced the child’s behavior was his medical history and multiple exposures to the medical environment. The child’s medical condition was recently discovered, which could contribute to the mother’s permissive parenting style. This style is usually displayed with the parent having little or no control of the child, providing few to no control of the child, providing few to no commands and making little to no attempts at limiting the child’s bad behavior [23]. It was previously reported that children with permissive parents exhibit significantly more caries and negative behavior in the dental clinic compared to those with authoritative parents [23].
Sickle beta thalassemia is a rare inherited disease that causes the formation of abnormal hemoglobin and reduced production of beta globin chains. Oro-facial manifestations seen in sickle beta anemia varies depending on the severity of the condition. This may include: lateral displacement of the orbits, saddle nose and frontal bossing, malar prominence, and maxillary protrusion with increased overjet and overbite. These appear to be due to hyperplastic expansion of the marrow cavity. Other dental features include macroglossia and atrophic glossitis, pallor mucosa. Radiographically, absence of inferior alveolar canal, short roots, and taurodontism are not uncommon findings. Finally, caries rate is high in thalassemia patients, mostly because of oral hygiene neglect and impaired salivary function [1]. Some of these features were evident in our case such as slight lateral displacement of the orbits and frontal bossing. Moreover, the paleness of skin and mucosa and dry lips can be easily distinguished.
The choice of referring the patient for general anesthesia was not considered due to the possible risks associated with this procedure for his condition. Parents also preferred managing their child in the clinic since the child had carious teeth that could be treated in dental setting and behavioral modification can be attempted. The behavior of the patient had improved and anxiety reduced towards the end of the treatment. This change in behavior could be as a result of different factors. The most important suggested factor behind this change was the presence of the father who has an authoritative parenting style. The father displayed firmness, sat limits, but yet showed compassion and warmth. Some households have bidirectional communication [23]. This was clearly reflected in the clinic as the father's presence was helpful in controlling his child's behavior compared to the mother. In addition, father had low dental anxiety which affected and was imitated by his child. He also responded to his child's anxiety with attention, comfort and support. Parents' responses to child anxiety have been reported to affect his ability to cope with his anxiety. They act as an external positive/negative reinforcement to maintain the child anxious behavior pattern [24]. The father's ability to control the child was supported by a previous study that recommended fathers accompanying their children as they positively affect their children's behavior compared to the mothers [25]. They reported that 90.6% of children accompanied by their fathers and 21.8% accompanied by their mother showed cooperative behavior during dental procedures with statistical significant difference between children’s cooperation.
Other behavioral management techniques such as tell-show-do, voice control, positive reinforcement, communication and distraction also played an important role in enhancing his behavior. Therefore, it is highly recommended to try all best to manage the patient with such medical condition utilizing different means of standard behavior management techniques under local anesthesia setting that tailored according to the stage of the child development. Furthermore, N2O and restrain, if used properly with positive approach, show an effective behavior technique in such uncooperative patient with or without medical disabilities. A previous study had reported that parents preferred N2O with papoose restrain more after their first experience [26]. When selecting a behavior method for medically compromised patient, especially with the possibility of prompting a crisis, the behavior technique should be used with caution. The dentist should have the ability to change his behavior method used smoothly when needed. Furthermore, N2O is preferred in Sβ-thalassemia [27].
This study discussed an important gap in the literature about managing an uncooperative medically compromised patient that is not recommended to be treated under general anesthesia. The case report not only described the child's behavioral changes, but also his parent’s behavior and anxiety reported to affect the child anxiety and behavior [25, 28, 29]. However, the main limitation is that we only reported a single case that could not be generalized to the population. Further cohort study is recommended to reach standardized effective methods in managing such cases where general anesthesia is not a solution
CONCLUSION
The child's stage of development, behavior and medical status should be taken into consideration prior, throughout, and after the delivery of dental care with proper consultation with the physician. It is also highly recommended that the pediatric dentist builds up a good rapport with the patient and their parents, understand the different parenting styles and their possible effect on the child’s behavior to achieve proper behavior management.
LIST OF ABBREVIATIONS
| Sβ-Thalassemia | = Sickle Beta-Thalassemia. |
| GA | = General Anesthesia. |
| CAT | = Caries-Risk Assessment Tool. |
| AAPD | = American Academy of Pediatric Dentistry. |
AUTHORS' CONTRIBUTIONS
Study conception: Hussain Alhasan, Ahmad Samara, Heba Sabbagh.
Data collection: Hussain Alhasan, Ahmad Samara.
Data acquisition and analysis: Hussain Alhasan, Ahmad Samara, Nada Bamashmous, Heba Sabbagh.
Data interpretation: Hussain Alhasan, Ahmad Samara, Nada Bamashmous, Heba Sabbagh.
Manuscript writing: Hussain Alhasan, Ahmad Samara.
The manuscript has been read and approved by all authors.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from the Research Ethics Committee at KAUFD (086-10-17).
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are basis of this research. The reported experiments in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was signed by the mother following discussing the treatment plan. The option of possible use of inhalational sedation using nitrous oxide was also explained. Consultation with the child’s pediatrician was obtained, stating no contraindications to the planned treatment.
STANDARDS FOR REPORTING
CARE guidelines and methodologies were followed in this study.
AVAILABILITY OF DATA AND MATERIALS
Data generated or analyzed during this study are included in this published article.
FUNDING
None.
CONFLICT OF INTEREST
The authors do not have any conflict of interest to declare.
ACKNOWLEDGEMENTS
Declared none.


