All published articles of this journal are available on ScienceDirect.
White Spot Lesions: A Serious but Often Ignored Complication of Orthodontic Treatment
Abstract
Objective:
The objective of this narrative review is to present an overview of the prevalence, clinical manifestation, diagnosis, and latest advances on white spot lesions.
Background:
White spot lesions have been defined as the earliest stage of demineralization on enamel surfaces that are easily discernible to the human eye.
Methods:
Relevant articles on white spot lesions were searched and reviewed from March 1975 till May 2021 in Pubmed, Scopus, Google Scholar, and ScienceDirect and were included in this review.
Results:
Even though the orthodontic field has seen several advances over the last few years, this is one complication that persists. White spot lesions are very commonly seen after completion of fixed orthodontic therapy when brackets are debonded. Previously conducted research has shown that there is a high prevalence rate of white spot lesions, which ranges from 50 to 90%. On intra-oral examination, a white spot can be seen as a matte-textured, opaque white lesion. Since the demineralization process takes place below the enamel surface, the outer layer only demonstrates pores that affect the natural light refractory properties of a tooth. This is what leads to the characteristic appearance of these lesions. One of the goals of modern dentistry is to treat non-cavitated lesions by promoting remineralization without the involvement of any invasive procedures.
Conclusion:
Fixed orthodontic therapy is usually a lengthy process and requires active cooperation between the orthodontist and the patient. However, it is the responsibility of the treating orthodontist to examine the tooth surfaces at each appointment to diagnose a developing white spot lesion as early as possible. With recent advances in diagnostic techniques, it has become much easier to identify these initial lesions and prevent their progression to cavitated lesions.
1. INTRODUCTION
White spot lesions (WSLs) have been defined as the earliest stage of demineralization on enamel surfaces that are easily discernible to the human eye. Since one of the principal objectives of orthodontic therapy is to help improve the esthetics of the patient, the occurrence of white spots not only compromises the outcome of the treatment but also predisposes the affected teeth to decay [1, 2]. Even though the orthodontic field has seen several advances over the last few years, this is one complication that persists. White spot lesions are very commonly seen after completion of fixed orthodontic therapy when brackets are debonded (Fig.1) [3]. In this review, relevant articles on white spot lesions were searched and reviewed from March 1975 till May 2021 in Pubmed, Scopus, Google Scholar, and ScienceDirect and were included in this review.
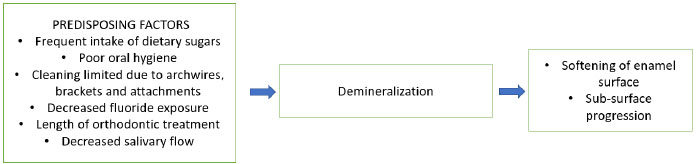
It has been demonstrated in previous studies that during orthodontic treatment, the bonded brackets and archwires make it difficult to maintain proper oral hygiene, which leads to prolonged accumulation of plaque. The cariogenic bacteria release several by-products such as polysaccharides from sucrose and lactic acid, which lead to a decline in pH in a highly localized environment. Once the balance between mineral deposition and loss is disrupted and tips towards demineralization, it eventually leads to the formation of white spot lesions [4]. White spot lesions are usually formed in two stages: the first stage is enamel surface softening due to mineral loss, while the second stage involves the formation of subsurface lesions because of further loss of minerals (Fig. 2).
2. PREVALENCE
Previously conducted research has shown that there is a high prevalence rate of white spot lesions, which ranges from 50 to 90% [5]. In another study, it was seen that the highest prevalence of WSLs was in the canines (48.1%), followed by lateral incisors (32.3%), the central incisors, and first premolars (31.6%) [6]. There was a lesser presence in the second premolars (27.2%), followed by molars, which only reported a low prevalence of 8.9% [6]. Studies have demonstrated that adolescent patients were more prone to developing white spots when compared to adult patients [7]. To support this argument, further research was conducted, which demonstrated that the age of the patient at the start of fixed orthodontic therapy and individual oral hygiene motivation levels of the patients were significant factors affecting the formation and extent of these lesions [8, 9]. The duration of the treatment is another important factor that has been shown to have a role in the development of WSLs [9]. These findings demonstrate that this is a major cause of concern that requires urgent attention from the orthodontic community.
3. CLINICAL MANIFESTATION AND DIAGNOSIS
On intra-oral examination, a white spot can be seen as a matte-textured, opaque white lesion. Since the demineralization process takes place below the enamel surface, the outer layer only demonstrates pores that affect the natural light refractory properties of a tooth. This leads to the characteristic appearance of these lesions [10]. Once these pores are formed, they are prone to absorbing colors from food items, and gradually their color starts to change from white to yellow to brown eventually. These mostly develop in proximity to orthodontic brackets and the gingival margins. White spot lesions are usually well-demarcated from their surrounding areas and must be differentiated from lesions caused due to fluorosis. Long-standing white spot lesions or initial caries require cavity preparation and restorations. Gorelick et al. classified white spot lesions based on their size and intensity to help diagnose them (Table 1) [11].
| Class | Size and Intensity |
|---|---|
| Class 1 | No white spot lesion |
| Class 2 | Mild white spot lesion |
| Class 3 | Severe white spot lesion |
| Class 4 | Cavitation and white spot lesion |
Once white spot lesions are formed, these need to be treated at the earliest to avoid their progression to decay. One of the goals in modern dentistry is to treat non-cavitated lesions by promoting remineralization without the involvement of any invasive procedures [12]. Various re-mineralizing agents have been researched for their benefits in helping treat white spot lesions. Some agents that have shown the most promising results in managing white spots are topical fluoride agents. Calcium sucrose phosphate works by providing a high concentration of free calcium and phosphate ions to affected areas, thereby acting as a re-mineralizing and cariostatic agent at the same time [13, 14]. On the other hand, fluorides are readily available in many forms, such as gels, pastes, mouth rinses, and even cement. Fluorides, if used as toothpaste, can be used in concentrations more than 1000 ppm, and studies have shown that a dentifrice with a fluoride concentration of more than 5000 ppm is very effective [15].

After fixed orthodontic treatment is complete and the brackets are removed, it is normal for white spot lesions to regress as the enamel surface is exposed to the mineral content of natural saliva. However, the extent of regression is dependent on the duration of the treatment as well as the severity of the lesion and occurs gradually over the next few months [16]. If the lesion still appears prominent after 6 months, then the lesion usually requires in-office treatment with procedures such as bleaching or micro-abrasion. Bleaching is only advised in patients with good oral hygiene, but it has been reported to increase sensitivity and reduce enamel hardness [17]. Micro-abrasion involves chemical and mechanical enamel surface treatment with an abrasive slurry containing hydrochloric acid. It is effective in the management of smaller lesions with a depth of less than 0.2mm [18]. Another minimally invasive method that has been proven to be useful in the treatment of white spot lesions is the use of resin infiltration [17].
4. LATEST ADVANCES IN THE DIAGNOSIS OF WHITE LESIONS
With the advent of digital dentistry, there have been several technological advances in the diagnosis and management of demineralized lesions that have taken place. Diagnosing initial carious lesions before they progress to larger cavities is of prime importance, and several recent advances can help identify initial lesions. Quantitative light-induced fluorescence is a recent method that employs the use of fluorescent light to identify demineralized areas [19-21]. Since these areas allow a faster spread of light, there is decreased fluorescence in the affected regions. Using this method, it is not only easy to identify the lesion but also measure its size as well as the density. Fiber optic transillumination-digital fiber-optic transillumination (FOTI-DIFOTI) is another new technique in which infra-red light (780nm wavelength) is used to identify white spot lesions without the use of ionizing radiation [20]. Laser fluorescence has been demonstrated to be useful in the diagnosis of demineralized areas located on flat enamel or occlusal surfaces. Devices using this method emit visible light (638-655nm wavelength) released by a diode laser [22]. This visible light is absorbed within the tooth structure and emits fluorescent light, which can be detected by a photodiode. One shortcoming of this method is that while it can help identify initial demineralization, it was not as effective at locating progression. Another recent method developed for early identification of white spot lesions is near-infrared light transillumination (NILT), which uses optical fibers to transmit light (780nm wavelength) to the tooth via the root [23, 24]. The light is gradually transmitted through the crown, and a charge-coupled device sensor is then used to create an image that can depict sub-surface lesions. A new technique known as Fluorescence Induced Theragnosis is very useful in diagnosing and helping manage white spot lesions, initial caries, and biofilm identification [25, 26].
CONCLUSION
Fixed orthodontic therapy is usually a lengthy process and requires active cooperation between the orthodontist and the patient. However, it is the responsibility of the treating orthodontist to examine the tooth surfaces at each appointment to diagnose a developing white spot lesion as early as possible. The unfortunate reality is that these are complications that can develop into decay requiring extensive restorations but are often ignored during patient follow-up visits. They are only located when they are prominently discolored or they progress to a cavity requiring restorative or endodontic treatment. The wide prevalence of such lesions in patients receiving orthodontic treatment as a result of negligence is something that we must take seriously and take corrective action.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


