All published articles of this journal are available on ScienceDirect.
Concrescent Teeth: Extraction Implications - A Case Report
Abstract
Background:
Concrescent teeth belong to the group of double teeth with disturbed anatomy of shape and structure. The concrescence consists of the aggregation of root cementum of adjacent teeth. This anomaly usually concerns the upper teeth in the lateral part of the jaw. Concrescent teeth can be treated conservatively, endodontically, orthodontically and surgically.
Objective:
The aim of this article is to present the case of the concrescence of upper teeth, a second molar tooth with an impacted third molar, and to draw the attention of clinicians to this rare anomaly that may cause medical and legal problems.
Case presentation:
This article presents the case of a 53-year-old woman who reported to the dentist’s office to extract tooth 17 due to chronic periodontitis and an impacted and abnormally placed tooth 18.
Result:
During the extraction, concrescence of the teeth was noted. The teeth were removed, and the alveoli were surgically treated. The postoperative period was uncomplicated.
Conclusion:
In this paper, the authors draw the attention of clinicians to the fact that the occurrence of concrescent teeth in clinical practice is rare and that it is difficult to diagnose this anomaly on the basis of routine radiological diagnostics based on 2D images. They also point to the necessity of a thorough physical examination and a thorough assessment of teeth before extraction, the extension of imaging diagnostics by conical CT scan in justified cases, and informing the patient about possible complications. In order to avoid serious complications, the extraction of the concrescent teeth should be performed by an experienced specialist in dental or maxillofacial surgery.
1. INTRODUCTION
Dual teeth are rarely found in everyday dental practice, and the most common among them are concrescent, fused and geminated teeth. In permanent teeth, this abnormality occurs in about 0.1% of patients, whereas in deciduous teeth, it represents 0.15 - 1.2% of cases [1-3]. According to the Cawson’s classification, the concrescent teeth relate to anatomical disorders of the shape and structure of teeth [4]. Tooth concrescence consists of the cementum connection within the roots, i.e., the connection between the root of one tooth and the crown of the other, an unerupted tooth; however, it is much less frequent [5]. Despite such a fusion, two separate cavities and two root systems are found because the dentin of both teeth does not fuse [6]. The cause for the teeth concrescence is not fully understood. It is suggested that this disorder may be caused by crowding of teeth, chronic pulp inflammation associated with caries, or excessive forces used in orthodontic treatment [6]. This may cause bone resorption in interdental spaces and, consequently, teeth bonding, resulting from the build-up of root cementum [6]. Teeth concrescence may also occur during their development [2, 7-9]. This abnormality most often occurs within the permanent upper teeth in the lateral region of the jaw [6, 7, 9-11]. There was no correlation found between the incidence of concrescent teeth and age, sex or race [8].
When performing basic radiological diagnostics, it is difficult to diagnose this disorder. Radiological symptoms indicating teeth concrescence may be the lack of bone septums between the gaps of these teeth periodontia, projection of the roots of adjacent teeth over each other, and incorrect placement of one of the teeth [12, 13]. It is then recommended to extend the diagnostics and perform CT scans to obtain a multi-faceted, three-dimensional assessment of the structure and topography of teeth.
Dental anomalies related to the concrescent teeth, irregularities in their localisation, or transposition teeth may affect not only the chewing pattern but also the dysfunction of the entire stomatognathic system. Accurate diagnosis of these abnormalities is of great importance in planning individual dental treatment [14, 15].
The aim of this article is to present the case of the concrescence of upper teeth, a second molar tooth with an impacted third molar, and to draw the attention of clinicians to this rare anomaly, which can cause not only diagnostic and therapeutic problems but also legal ones.
2. CASE REPORT
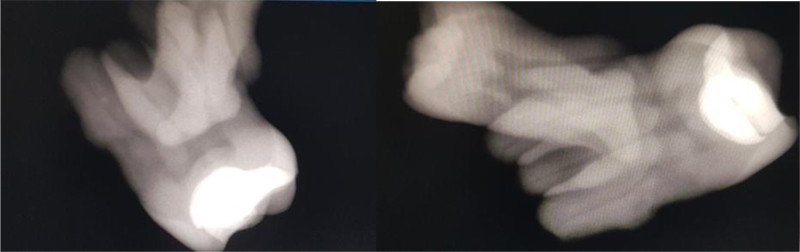
A 53-year-old female patient visited the dentist’s office for a surgical oral cavity sanitation before the planned prosthetic treatment of missing teeth with an upper and lower frame denture. The patient was generally healthy without addictions, and did not take any medication. She did not report any other diseases or orthodontic treatment in the past. In the anamnesis, she reported recurrent inflammations in the area of tooth 17, transient spontaneously or after antibiotic therapy. The extraoral examination did not reveal any pathological changes. An intraoral examination revealed secondary caries around the leaking composite filling, after earlier treatment of carious defect class I according to Black classification [16] in tooth 17, no reaction of the pulp to ethyl chloride, negative periodontium reaction to vertical and horizontal rinsing, and lack of visibility of tooth 18 in the oral cavity. In addition, teeth 14, 11, 24, 34, 44, 47 with composite fillings, tooth 23 with a prosthetic fixation and delivery in place of the missing tooth 22, generalized chronic periodontitis and numerous interdental deficiencies were found. For the purpose of radiological diagnosis and evaluation of the present teeth, a panoramic radiograph was taken (Fig. 1). The image, correctly positioned (palatal line parallel to the horizontal plane, mandibular condyles symmetrical), showed tooth 17 with a contrasting material of the type of filling reaching the pulp’s chamber, lack of contrasting material in the root canals, periodontium widening around the roots of tooth 17 and osteolytic cavities around the apexes which may correspond to lesions of the nature of chronic periodontitis. Tooth 18 was partially impacted, placed with the crown upwards and backwards, with the roots projecting on the tooth 17. The image also showed the presence of contrasting material within the crowns of teeth 14, 11, 23, 24, 34, 44, and 47, as well as missing teeth 16, 15, 12, 21, 22, 25, 26, 27, 28, 48, 46, 45, 35, 36, 37, 38. The alveolar recesses of the maxillary sinuses were properly aerated. Moreover, pathological radiological lesions within the structure of the maxillary and mandible bones were not found. The patient did not agree to extend the diagnostics and perform conical computed tomography (CBCT) due to her economic status.
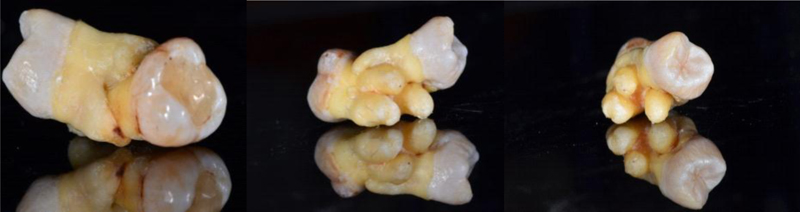
Tooth 17 was qualified for extraction due to chronic periapical tissue inflammation, recurrent inflammatory conditions, and the patient’s lack of consent for endodontic treatment. A decision was also made to extract the impacted, abnormally placed tooth 18 (Figs. 2 and 3).

The patient provided a written consent for the extraction of teeth 17 and 18.
Under infiltration anesthesia, 1.8ml of articaine hydrochloride solution with adrenaline 1:100 000 (Orabloc40mg/1ml+0.01mg/1ml x 1amp. 1.8ml; by Marrodent), a dental ligament of tooth 17 was prepared, and tooth 17 was completely extracted using Berten’s forceps for the upper right molars as well as tooth 18 concrescent with it. The teeth were removed simultaneously due to the dental-connected alveoli. Then, the alveolus of tooth 17 connected to the alveolus of tooth 18 was examined. A negative air and mechanical test showed no connection between the oral cavity and the maxillary sinus. The wound after extraction of the two joined teeth was not too large, and preparing flap was not needed. Wound after extraction of concrescent teeth would not have been smaller if the teeth had been sectioned. The gingival wound’s margins were sutured using non-absorbable polyamide sutures with a monofilament structure, SERALON® 4-0 floss by Serag-Wiessner. We used horizontal mattress sutures. A pressure dressing was applied to the alveolus.
The patient left the dentist’s office with postoperative recommendations (maintaining the pressure dressing for 20 minutes, not eating solid food for about 2 hours). Control examinations were performed on the third and seventh day after extraction. The sutures were removed during the second follow-up visit. The course of healing was uncomplicated, and the wound after extraction healed properly. The patient was referred to a prosthetist for continuation of the treatment.
3. DISCUSSION
Teeth concrescence is a rare abnormality in both deciduous and permanent dentition, which may contribute to numerous complications and treatment failures. The etiology of this anomaly is still not completely understood. The literature distinguishes several causes of teeth concrescence. One of them may be the too close location of tooth buds during odontogenesis, which may result from, for e.g., local trauma. Teeth concrescence can be caused by excessive bite forces triggered by abnormal occlusion in patients with malocclusion. As shown by the research conducted by Piancino et al., occlusion disorders can affect muscle activity and alter the chewing function [15].
The next cause is chronic inflammation around the root of the tooth, causing the root cementum of the tooth to build up and, as a result, concrescence with the tooth in its close vicinity [2, 8, 9]. In the prevention of teeth concrescence, the important role of the correct periodontal space with efficient periodontium is also emphasized. The periodontal ligaments maintain the width of the periodontal space at the level of 0.2 - 0.4 mm, depending on Malassez epithelial cells functions, which continuously release the epithelial growth factor (EGF) to this area. EGF in periodontal ligaments stimulates bone resorption only from the alveolar surface [6]. This process, however, does not occur on the surface of the teeth roots because the cementoblasts do not have suitable receptors for EGF, which prevents root resorption. This explains why teeth that are even close together, often crowded, and do not come into direct contact with the surrounding bone. Due to the impairment of the periodontium function and atrophy of its fibers in case of unerupted or impacted teeth, which do not take part in the occlusion for years, alveolar ankylosis and external root resorption may occur. Atrophy of the periodontal ligaments causes the tooth to be closer and closer to the bone, and bone bridges may form between it and the alveolar plate and substitute bone build-up in the site of root cementum resorption. The situation is similar in the case of two separate teeth, when one of them is erupted and the other does not show significant periodontal activity because it is impacted or in infraocclusion. In the case of impairment of the periodontium function associated with a disturbance of the teeth eruption and malocclusion, the root cementum of these teeth does not rebuild, but it just suppresses the next layers approaching the root of the other tooth. The lack of an interdental septum and the lack of periodontium function of one of the teeth may lead to the connection of cementum layers between the dental roots. The cementum of two teeth is initially joined by means of very thin layers of non-mineralised precementum, which then merge and undergo mineralization, leading to teeth concrescence [6].
Generalized hypercementosis and teeth concrescence may also occur in the course of systemic diseases, such as Paget’s disease, thyroid goiter, rheumatic fever, rheumatic arthritis and acromegalia [2, 3, 17]. Paget’s disease also leads to obliteration of the periodontal ligaments and ankylosis, which shows resorption of the external alveolar plate [3]. The described patient and members of her family did not suffer from these general conditions. Moreover, she did not report injuries at the anamnesis. Apart from a single case of the concrescence of two upper teeth, she did not show any other abnormalities in the structure of teeth in the upper and lower dental arch. Therefore, it is difficult to clearly determine the cause of the anomaly.
The incorrect position of tooth 18, whose crown was directed towards the maxillary tuber and the roots overlapped on the roots of tooth 17, may indicate the concrescence of these teeth during their development. This could also occur after the end of teeth development due to the lack of occlusal function of incorrectly positioned and impacted tooth 18 and the related atrophy of periodontal ligaments and their function, which could lead to adhesion with the adjacent tooth 17. On the other hand, the patient was diagnosed with generalized chronic periodontitis and chronic inflammation around the apexes of tooth 17, lasting for several years, which could also result in the concrescence of the teeth.
Most often, the concrescent teeth are observed in the lateral region of the maxilla. In this area, there is often little space for teeth and interdental septum, which may cause the crown of the third upper molar to rotate in a distal direction towards the maxillary tuber and bring its roots closer to those of the second upper molar. The majority of cases, as in the case of the patient described in this paper, are associated with the concrescence of the upper second and third molar [10, 18, 19] or the first molar with the second molar in the maxilla [2]. The concrescence of the third upper molar tooth with an over-dimensional tooth in the jaw may also occur [7]. In the literature, we can also find other locations of the concrescent teeth, such as the concrescence of the third molar and an additional tooth in the mandible [11, 20, 21] and the concrescence of the upper deciduous teeth in the anterior segment of the maxilla [22, 23]. The concrescences in the anterior teeth are extremely rare, especially between two teeth properly functioning in the arch due to the activity of healthy dental ligaments. Even in the case of trauma, when Malassez epithelial cells in the anterior teeth are destroyed, alveolar ankylosis and the replacement root resorption of the tooth rather than concrescence with the adjacent tooth are formed [6].
The presence of concrescent teeth cannot be attributed to gender or age. The literature describes the cases of concrescent teeth in both 83-year-old female [2] and 18-year-old male [7]. The patient presented was 53 years old on the day of surgery.
The image of the concrescent teeth on radiographs of teeth, adjacent to the alveolar process, and panoramic radiograph ones can be uncharacteristic and often difficult to interpret properly. In the case of diagnostic uncertainties, found on radiological images, consisting of overlapping roots of two different teeth, reversing the crown of one tooth in the opposite direction (in our case, backwards and upwards towards the maxillary tuber), and additionally inducing injury to the area, it is recommended to extend the radiological diagnostics. It is possible to take intraoral dental images in various projections. However, 2D radiological images have limited diagnostic usefulness due to image distortion and overlapping anatomical structures. The image evidencing the concrescence of teeth may be the lack of bone septums between the periodontium space of these teeth [20]. In selected cases, it is advisable to perform computed tomography or conical tomography, which can enable accurate spatial imaging of the structure and mutual arrangement of teeth, thus confirming or excluding the existing anomaly. The described patient did not agree to extend the diagnosis and perform CBCT for economical reasons.
Correct diagnosis enables appropriate therapy, which can be undertaken after presenting the treatment plan to the patient and obtaining acceptance. Concrescent teeth can be treated conservatively, endodontically and surgically. Despite the different anatomy of the canal system of these teeth, in cases of irreversible inflammation or pulp necrosis, it is possible to treat them endodontically. However, when planning to leave both teeth in the oral cavity, it should be considered that these teeth have a common communicating dental ligament, so endodontic treatment must be carried out for both teeth at the same time, even if the pathology concerns only one of them. It is also possible to separate the concrescent teeth. Simple separation while maintaining the proximity of both teeth may cause their repeated concrescence, so it is necessary to orthodontically separate the teeth or remove one of them. Displacement of the teeth without separating them, together with the bone of the alveolar process, is not easy as it requires very high orthodontic forces, and may lead to root resorption. After separating the teeth, they can be moved in the usual way. In the process of tooth displacement, the concrescent teeth can also act as a retention point for the braces. When the position of one of the teeth prevents endodontic access, this is an indication for the separation and extraction of one tooth or even both of the concrescent teeth [9]. If the concrescence includes the apex hole or a tooth qualified to be left in the oral cavity requires conservative treatment, it should be performed before the teeth separation procedure. The tooth left after the separation is usually repaired with the newly formed cementum at the site of separation. This lasts two to three weeks. In the meantime, the root can be partially resorbed and covered with new cementum. After one to three months, the separated teeth can be moved if there is a clinical necessity [6].
In some cases, it is not possible to treat the teeth conservatively or to separate them and leave at least one of them; in this case, the two teeth should be removed [9]. The procedure is most commonly performed under local anesthesia [1-3, 10, 11], rarely under general and endotracheal anesthesia [19]. In the case of the patient presented in our study, the endodontic treatment of both teeth was not possible due to partial impact and abnormal position of tooth 18. Moreover, the patient did not consent to the separation and removal of tooth 18 and endodontic treatment of tooth 17. Therefore, the decision was made to extract teeth 17 and 18 under local anesthesia.
The procedure of concrescent teeth extraction is burdened with the risk of various complications during the extraction, for e.g., fractures of the maxillary tuber, connection of the oral cavity with the maxillary sinus, or mandible fractures [9, 20]. In the case described, the concrescent teeth 17 and 18 were removed by the alveolus of tooth 17. No oroantral fistula occurred, and flap plastic surgery was not required. Wound healed properly in the postoperative period. The surgical procedure was performed by an experienced specialist in dental surgery, which involved the removal of the concrescent teeth; it resulted in being minimally invasive and without complications.
Estabilishing a correct diagnosis of the concrescent teeth is of great importance in choosing the right form of treatment and enabling the patient to make an informed decision and agree to the procedure. Moreover, it allows to properly plan the type and extent of the procedure, taking into account, among others, the possibility of various complications during the extraction of the concrescent teeth [9, 20]. The information regarding the possibility of such an anomaly should be included in the written consent and signed by the patient before the planned extraction. This may protect the dentist from the legal responsibility of the procedure, to which the patient did not give informed consent; in this case, it was the removal of a neighboring, concrescent tooth. The lack of patient consent for a more accurate imaging diagnosis (CBCT) is an additional difficulty, both in planning the treatment and in carrying out the procedure itself, increasing the risk of complications and patient claims. The knowledge, practical skills and experience of the surgeon performing the procedure may help avoid these problems. However, in the absence of a proper diagnosis, and therefore, a full and proper consent of the patient to perform the surgical procedure, the concrescent teeth should be retained or their photographs taken as evidence in case the patient claims.
CONCLUSION
In the case of suspicion of the occurrence of concrescent teeth before the implementation of treatment, it is advisable to perform conical tomography, which will facilitate correct diagnosis and selection of effective treatment after obtaining the patient’s conscious consent to the proposed treatment. Unfortunately, due to difficulties in access to wider radiological diagnostics and economic possibilities of the patient, it is not always possible to perform it. Often, the diagnosis of the concrescent teeth is made only after extraction. Therefore, dentists need to be aware of this abnormality in both deciduous and permanent dentition and of the related complications that accompany such procedures, which should also be communicated to the patient. After analyzing the case described and the literature data, it has been deemed necessary to emphasize that the procedure of removal of the concrescent teeth should be carried out by an experienced specialist in dental or maxillofacial surgery.
AUTHORS’ CONTRIBUTIONS
ŁW contributed to the conceptualization of the study, collection of the material, did the surgical procedure, designed graphical part of the manuscript, and wrote the manuscript; KŁ conceptualized the study, conducted the literature survey, and wrote the manuscript; BA took part in conceptualization of the study, literature survey, and writing of the manuscript; JB contributed to conceptualization of the study, literature survey, and writing of the manuscript; BA, JSz and JB provided their final approval for the version of the manuscript to be published.
ETHICAL STATEMENT
The authors confirm that ethics approval is not required for this case report.
CONSENT FOR PUBLICATION
The participant involved in this study provided her written informed consent.
STANDARDS FOR REPORTING
CARE guidelines and methodologies have been followed in this study.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


