All published articles of this journal are available on ScienceDirect.
Surgical Orthodontic Treatment for Skeletal Class I with Facial Asymmetry and Occlusal Cant: A Case Report
Abstract
Background:
Cases of facial asymmetry with chin deviation and canted occlusal plane represent a challenge in orthodontic treatment.
Case Report:
We report successful surgical orthodontic treatment for skeletal Class I with severe facial asymmetry. Miniscrew anchorage was used to decompensate the canted occlusal plane in presurgical orthodontic treatment with a fixed appliance by the intrusion of the maxillary right molars and extrusion of the left molars. Then, orthognathic surgery consisting of bilateral sagittal split osteotomy for asymmetric mandibular setback was performed. Treatment resulted in marked improvement of facial asymmetry.
Conclusion:
The use of miniscrew implant anchorage may represent a superior presurgical orthodontic treatment and expand the possibility of treatment by one-jaw surgery.
1. INTRODUCTION
Cases of facial asymmetry with dental midline and chin deviations represent challenges in orthodontic treatment [1]. The facial and dental midline have an essential role in facial esthetics [2], and their deviation is one of the typical features of facial asymmetry cases. The facial asymmetry cases are frequently associated with not only mandibular deformation but also maxillary deformation [3, 4]. Frontal occlusal plane canting of the maxilla is a common finding in patients with facial asymmetry [5, 6]. Therefore, nongrowing patients with severe facial asymmetry should be treated using a combined orthodontic/orthognathic two-jaw surgical approach rather than a mandibular one-jaw surgical approach or orthodontic camouflage to achieve significant correction of the craniofacial asymmetry [6-8].
The use of a Temporary Anchorage Device (TAD), such as a miniplate or miniscrew implant, has been widely accepted in clinical orthodontics [9, 10]. The orthodontic treatment using TAD enables extensive tooth movement, including molar intrusion and distalization [11], which are extremely difficult to achieve with conventional fixed appliances alone. Therefore, presurgical orthodontic treatment with fixed appliances combined with the use of TAD may expand treatment options. Recent case reports have described the successful use of a miniscrew implant to correct a canted maxillary occlusal plane in conjunction with orthodontic/orthognathic surgery therapy [12, 13]. If the maxillary asymmetry is limited to a mildly canted occlusal plane, correcting the occlusal plane using a fixed appliance combined with miniscrew implant anchorage makes minimally invasive treatment possible by simpler one-jaw mandibular surgery rather than complex mandibular-maxillary two-jaw surgery.
In this case report, we describe successful surgical orthodontic treatment for skeletal Class I with severe facial asymmetry. Miniscrew implant anchorage was used to decompensate the dental arch tipping and canted occlusal plane as presurgical orthodontic treatment. Then, orthognathic surgery consisting of Bilateral Sagittal Split Osteotomy (BSSO) for asymmetric mandibular setback was performed.
2. CASE REPORT
2.1. Diagnosis and Etiology
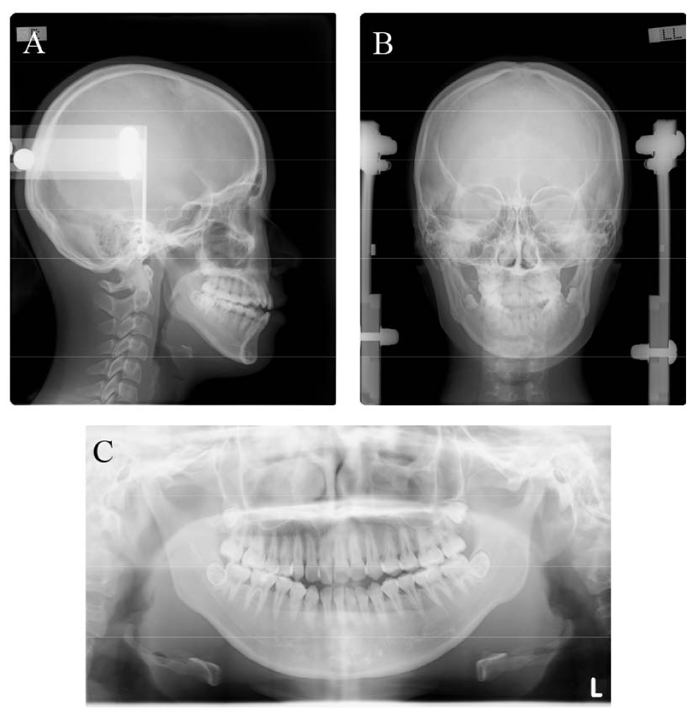
The patient was a girl aged 20 years and 5 months who came for orthodontic treatment with chief complaints of anterior open bite and facial asymmetry (Fig. 1). The patient had no relevant family history and no medical or dental history of dental trauma. She had a straight profile and severe mandibular deviation toward the left according to the mandibular deformation in addition to occlusal plane canting and transverse dental compensation. The soft tissue vertical reference line was constructed as the line perpendicular to the interpupillary line [14]. The maxillary dental midline and the mandibular dental midline were deviated 1.5 mm and 7.5 mm toward the left of the facial midline, respectively. The soft-tissue menton deviated 12.0 mm toward the left. Intraoral examination showed Angle Class III molar relationship on the right and Angle Class I molar relationship on the left with minor crowding of both dentitions. Overjet was 0.2 mm, and the overbite was –2.5 mm.

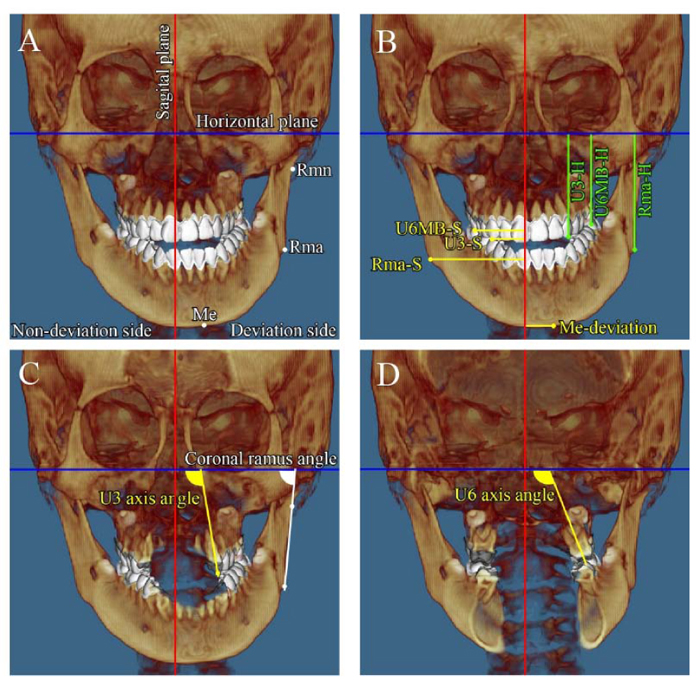
Panoramic radiography showed no horizontal or vertical bone loss and normal root length (Fig. 2). The cephalometric assessment showed a skeletal class I relationship (ANB angle, 3.2°) (Table 1) with a high mandibular plane angle (FMA, 35°) and occlusal plane angle (Occ plane to FH, 15.0°). The mandibular and maxillary incisor inclinations were normal (FMIA, 56.2°; U1-FH, 113.6°). Computed tomography (CT) imaging showed marked menton deviation to the left (13.5 mm) (Fig. 3 and Table 2) and dental asymmetry associated with occlusal plane cant (bilateral differences in tooth height: U3-H, 0.9 mm; U6MB-H, 3.3 mm). In addition, the bilateral differences in coronal ramus angle (coronal ramus angle, 10.3°) and ramus position (Rma-S, 13.6 mm) were significant [15].
| Variables | Mean | SD | Pre-Treatment (T1) | Post-Treatment (T2) |
| SNA (degree) | 82.5 | 3.7 | 81.8 | 81.8 |
| SNB (degree) | 79.2 | 3.7 | 78.6 | 76.8 |
| ANB (degree) | 2.8 | 0.8 | 3.2 | 5.0 |
| FMA (degree) | 27.3 | 3.1 | 35.0 | 35.8 |
| U1-FH (degree) | 115.3 | 6.0 | 113.6 | 111.6 |
| L1-MP (degree) | 95.5 | 3.1 | 89.1 | 92.1 |
| FMIA (degree) | 57.2 | 3.9 | 56.2 | 53.6 |
| FH-OC (degree) | 8.8 | 3.4 | 15.0 | 13.5 |
| Overjet (mm) | 2.8 | 1.0 | 0.2 | 2.0 |
| Overbite (mm) | 2.2 | 1.1 | -2.5 | 1.3 |
2.2. Treatment objectives
We made a diagnosis of skeletal class I malocclusion with mandibular deviation along with the maxillary canted occlusal plane. Treatment was performed to correct the facial appearance, improve the skeletal asymmetry, and establish appropriate incisor and molar relationships.
2.3. Treatment Alternatives
To achieve the treatment objectives, two possibilities were considered and discussed with the patient.
The first alternative involved combined fixed orthodontic treatment and orthognathic surgery by LeFort I osteotomy to correct the canted occlusal plane combined with BSSO for the asymmetric mandibular setback and maxillary first premolar extraction on both sides to correct maxillary incisor crowding. Extraction of both mandibular third molars would be necessary.
The second alternative involved combined fixed orthodontic treatment and orthognathic surgery by BSSO for the asymmetric mandibular setback. Maxillary first premolar extraction on both sides to correct maxillary incisor crowding and miniscrew implant anchorage would be used to correct the canted occlusal plane. Extraction of both mandibular third molars would be necessary.
After the two treatment plans had been explained to the patient, she selected the second option and provided informed consent to proceed.
2.4. Treatment Progress
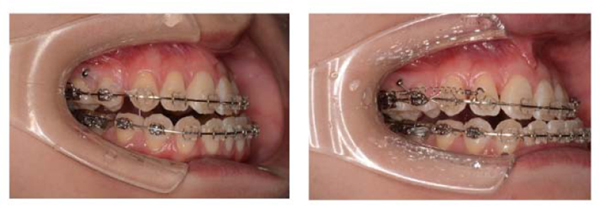
The mandibular third molars (teeth 38 and 48) were extracted under general anesthesia before orthodontic treatment. The mandibular teeth were bonded with preadjusted edgewise brackets (0.022 × 0.028-inch slot), and the mandibular teeth were leveled and aligned using sequential nickel-titanium alloy wires. After extraction of the maxillary first premolars, a 0.022-inch slot preadjusted edgewise appliance was bonded to the maxillary teeth, and leveling and alignment were started using sequential nickel-titanium alloy wires. Next, a miniscrew implant 1.6 mm in diameter and 6 mm in length (Dual-top Auto Screw III; Jeil Medical, Seoul, Korea) was placed in the buccal region between the right maxillary second premolar and first molar (Fig. 4). The maxillary canines were retracted using a 0.016 × 0.022-inch stainless steel wire with elastic chains by application of intrusive force (250 g load). Then the maxillary incisors were retracted using sliding mechanics along a 0.018 × 0.025-inch stainless steel wire with nickel-titanium closed coil springs (250 g load). After presurgical orthodontic treatment for 26 months, orthognathic surgery with BSSO was performed. The mandible was asymmetrically set back 7.0 mm on the right side and 0 mm on the left side. Postsurgical orthodontic treatment was performed for 13 months, and then the fixed appliances were removed after a total treatment time of 3 years and 3 months (Fig. 5), and the patient received a maxillary wraparound retainer and mandibular bonded lingual retainer.

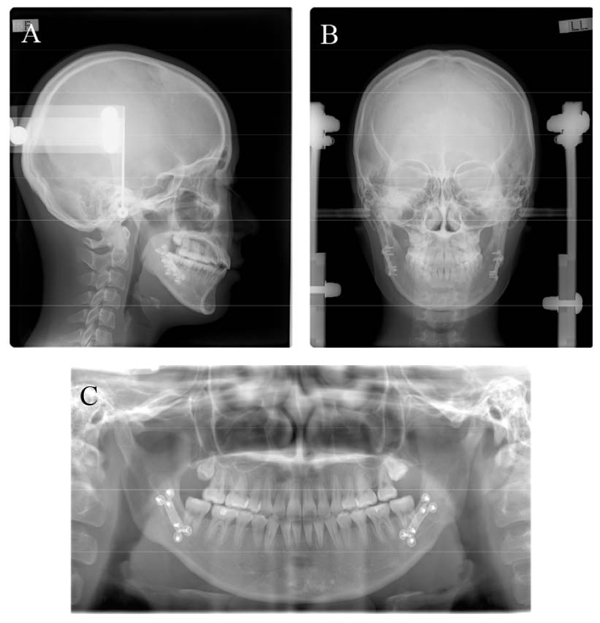
2.5. Treatment Results
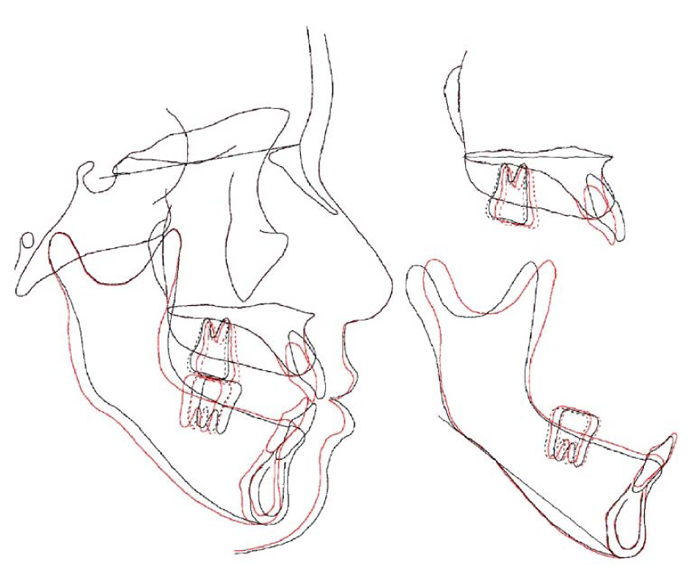
The post-treatment records showed that the procedures resolved the occlusal cant and mandibular asymmetrical setback, improving the facial asymmetry (Fig. 5). The dental midlines were coincident with the facial midline, and proper class I canine relationships on both sides were achieved. The soft-tissue menton deviation was improved from 12.0 mm to 2 mm toward the left of the facial midline (Fig. 6). Panoramic radiography showed acceptable root paralleling without root resorption (Fig. 7). Cephalometric analysis (Fig. 7a and Table 1) and superimposition (Fig. 8) showed that a skeletal class I jaw relationship had been maintained (ANB angle, 5.0°), although the SNB angle was slightly decreased from 78.6° to 76.8° as a result of mandibular asymmetrical setback. The mandibular plane angle was increased slightly from 35.0° to 35.8° (FMA). The mandibular incisors were slightly proclinated from 56.2° to 53.6° (FMIA), and the maxillary incisors were slightly retroclinated from 113.6° to 111.6° (U1-FH).

The intrusion of the maxillary right dentition (N-side: U3-H 0.4 mm canine intrusion, U6MB 1 mm molar intrusion) and extrusion of the left dentition (D-side: U3-H 0.6 mm canine extrusion, U6MB 2.1 mm molar extrusion) resolved occlusal plane canting, contributing to facial asymmetry. Significant improvements were also seen in coronal ramus angle (N-side 78.0°, D-side 80.9°) and ramus position (Rma-H: N-side 55.9 mm, D-side 54.5 mm) after orthognathic surgery with BSSO.
| - | Non-Deviation Side | Deviation Side | ||
| Variables | Pre-Treatment | Post-Treatment | Pre-Treatment | Post-Treatment |
| Menton deviation (mm) | - | - | 13.5 | 3.8 |
| Coronal ramus angle (degree) | 76.0 | 78.0 | 86.3 | 80.9 |
| Rma-S (mm) | 41.6 | 45.4 | 55.2 | 48.4 |
| Rma-H (mm) | 57.7 | 55.9 | 53.2 | 54.5 |
| U3-S (mm) | 13.2 | 16.0 | 21.3 | 21.4 |
| U3-H (mm) | 44.9 | 49.5 | 49.0 | 49.6 |
| U3 axis angle (degree) | 96.2 | 100.7 | 104.6 | 103.2 |
| U6MB-S (mm) | 21.5 | 23.8 | 30.9 | 28.5 |
| U6MB-H (mm) | 46.2 | 45.2 | 42.9 | 45.0 |
| U6 axis angle (degree) | 92.5 | 100.3 | 112.8 | 101.5 |
3. DISCUSSION
The most common feature of facial asymmetry is the dental midline and menton deviations from the facial midline. A previous study classified the dental-facial midline according to the deviation of the maxillary and mandibular dental midline relative to the facial midline [2]. They found that the maxillary and mandibular dental midline were not coinciding in almost 3/4th of their study subjects, as shown in the present case. In the present case, the combination treatment with fixed orthodontic treatment using miniscrew anchorage and orthognathic one-jaw surgery therapy markedly improved the dental-facial midline (both dental-midlines were coincident with the facial midline). In addition, the soft-tissue menton deviation was improved from 12.0 mm to 2 mm toward the left of the facial midline. A previous study reported that human sensitivity for perceiving facial imbalance increases when the skeletal deformation is close to or larger than 4 mm [4]. According to the results, it can be considered that the present treatment was effective in improving the dental-facial midline and menton deviations.
Facial asymmetry has a marked influence on physical appearance, and numerous dysmorphic syndromes are associated with severe mandibular asymmetry [16]. Such cases have multifactorial problems, including skeletal deformation and dental compensation [3, 4, 16]. Therefore, accurate evaluation of facial asymmetry by three-dimensional analysis with CT is required to achieve successful treatment outcomes [6, 17]. In this case, detailed CT imaging showed severe facial asymmetry associated with occlusal plane cant (bilateral differences in tooth height; U3-H, 0.9 mm; U6MB-H, 3.3 mm), transverse dental compensation (bilateral difference in U6 axis angle: 20.3°), and mandibular deformation. Two-jaw orthognathic surgical approaches are usually used to treat facial asymmetry with severe maxillary deformation, including dental asymmetry [6–8]. As maxillary deformation in the present case was limited to a mildly canted occlusal plane and transverse dental compensation, a one-jaw surgery approach (BSSO) was applied to correct the mandibular facial asymmetry. The canted occlusal plane and transverse dental compensation were resolved by a combination of a fixed appliance with miniscrew implant anchorage during presurgical orthodontic treatment. A satisfactory treatment outcome with a symmetrical facial appearance was achieved.
The use of a miniscrew implant as anchorage has become widely accepted in clinical orthodontics in the last few decades [9, 10], enabling extensive tooth movement and expanding orthodontic treatment options [11]. This patient had severe facial asymmetry with mandibular deformation in addition to the occlusal plane canting and transverse dental compensation. Our presurgical orthodontic treatment with fixed orthodontic appliances combined with miniscrew anchorage allowed straightening of the transverse occlusal plane by the intrusion of the maxillary right dentition and extrusion of the maxillary left dentition. These changes would not have been possible without the anchorage. Therefore, the combined method was the best choice in the present case.
The use of miniscrew implant anchorage for presurgical orthodontic treatment enables minimally invasive approaches. The present case of facial asymmetry was treated through a simpler one-jaw mandibular surgery rather than a complex mandibular-maxillary two-jaw surgery. It is of great benefit to the patient if maxillary surgery is unnecessary, lowering the degree of surgical invasion as well as medical costs [18].
CONCLUSION
The combination treatment with fixed appliance using miniscrew anchorage and orthognathic one-jaw surgery is effective for patients with facial asymmetry and canted maxillary occlusal plane.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for the publication of this case report, including accompanying images.
STANDARD FOR REPORTING
CARE guidelines and methodology were followed to conduct the study.
AVAILABILITY OF DATA AND MATERIALS
None.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


