All published articles of this journal are available on ScienceDirect.
Diagnosis and Management Approaches for Non-cavitated Carious Dental Lesions- A Narrative Review
Abstract
Background:
Dental caries is one of the most prevalent diseases. Its detection and management should start with a comprehensive treatment plan, with the goals of the elimination of cariogenic bacteria, the reduction of plaque acidogenicity, the encouragement of tooth remineralization, and the repair of damaged teeth.
Objectives:
The aim of this paper was to review the literature regarding the latest updates on the diagnosis and management approaches of non-cavitated carious dental lesions.
Methods:
Studies regarding the diagnosis and management of non-cavitated carious dental lesions were included.
Results:
The subclinical non-cavitated carious lesion might progress to an early enamel lesion, develop into an established dentin lesion, or sometimes end up with a lesion reaching the pulp. The detection and management of caries should be patient-centered, risk-based, and evidence-supported, and should consider the dentists’ expertise and the patients’ needs and preferences. The visual-tactile and radiographic detection of non-cavitated carious lesions are greatly helped by the advances of non-invasive detection tools such as DIAGNOdent, fiber-optic transillumination, quantitative light-induced fluorescence, and DIAGNOcam.
Conclusion:
Accordingly, non-cavitated carious lesions can be arrested by several non-invasive techniques, which are preferred over the invasive options. The clinicians can use sealants plus fluoride varnish on occlusal surfaces, fluoride varnish or resin infiltration on proximal surfaces, and resin infiltration,fluoride gel, or varnish alone on facial or lingual surfaces to manage non-cavitated carious lesions.
1. INTRODUCTION
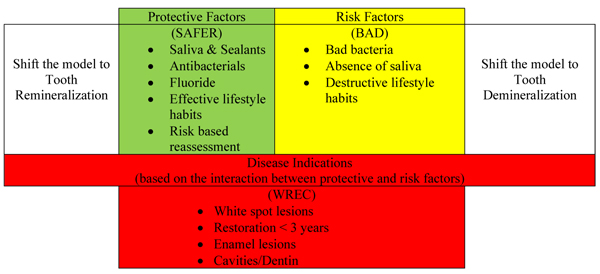
Dental caries is an epidemic and one of the most prevalent and costly diseases due to the increased consumption of sugar [1]. The carious damage of tooth structures depends on sugar consumption, which sometimes causes cavity formation in the three tooth structures: enamel, dentin, and cementum [2]. Young and Featherstone in 2013 stated that caries is a multifactorial disease, and accordingly, they established the caries balance/imbalance model to explain the complex interaction between pathogenic risk factors and protective factors leading to disease indicators (Fig. 1). The model predicts whether the carious lesion can progress, be arrested, or be reversed. For instance, if the protective factors balance the risk factors, the model will shift to a healthy status. On the other hand, if the risk factors outweigh the protective factors, demineralization will start, shifting the model toward caries progression [3]. Fortunately, if this imbalance happens, it can be reversed to avoid surgical treatment of caries, but this should be done before cavitation [4].
The detection and management of caries should start with a comprehensive treatment plan,with the goals of the elimination of cariogenic bacteria, the reduction of plaque acidogenicity, the encouragement of tooth remineralization, and the repair of the damaged teeth .However, the efforts to achieve these goals were limited because most of the clinical approaches were directed towards restoring decayed teeth with surgical approaches [4]. Additionally, dental carious lesions should be categorized based on whether the lesion has cavitated or not, in order to make the correct decision about restoration. All non-cavitated lesions can be arrested and remineralized through preventive therapy [4]. Non-cavitated lesions are better diagnosed by clinical examination. In addition, radiographic examination and other diagnostic tools likefiber-optic transillumination can be used to diagnose caries, as well as to prevent the breakage of the enamel surface [5]. Non-restorative treatment is a form of what is called causal treatment, which is implemented to delay or replace invasive restorative treatments with a causal approach, to decrease discomfort for children and promote oral health over time [6].
The aim of this paper was to review the literature regarding the latest updates on the diagnosis and management approaches of non-cavitated carious dental lesions.
2. METHODS
A search was carried out on Pubmed and Google Scholar using the keywords: “non-cavitated”; “non-invasive”; “micro-invasive”; “carious dental lesions”; and “caries management”. These words were used separately and in combination during the search.More information was retrieved from the American Academy of Pediatric Dentistry (AAPD) guidelines, the American Dental Association (ADA) guidelines,and from the publications of the World Health Organization (WHO). The references these sources used were then investigated further. The search time was between November 2018 and March 2020.
3. DEFINITION OF THE NON-CAVITATED CARIOUS LESIONS
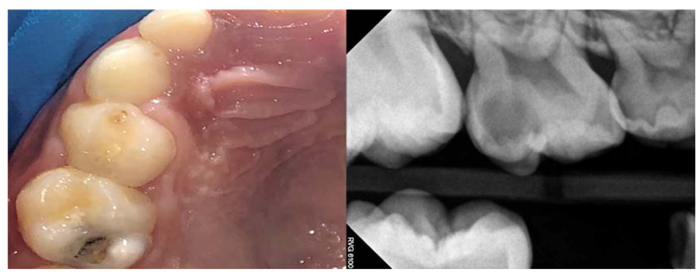
Dental caries have a continuum status. It starts in the very early stage with a subclinical non-cavitated lesion. It then becomes visible when it is converted into an early enamel lesion. After that, caries can develop into an established dentin lesion (Fig. 2), and it sometimes end up with a severe lesion reaching the pulp [7, 8]. It is critical to manage non-cavitated carious lesions as early as possible. However,these lesions have traditionally been detected at the cavitation stage, and their management has focused strongly on operative treatment [9].
4. DIAGNOSIS OF THE NON-CAVITATED CARIOUS LESIONS
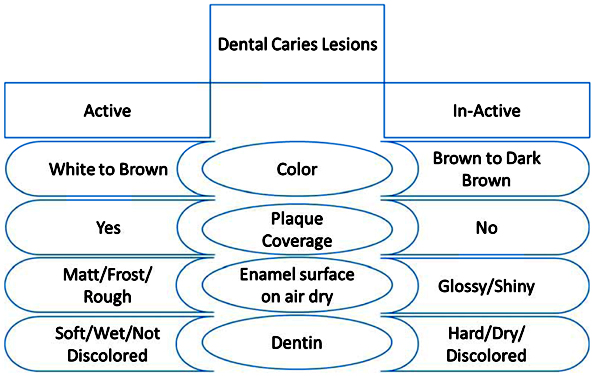
The accurate diagnosis of carious lesions is the key totheir proper management. In addition, current concepts for carious lesion detection have categorized the lesions as cavitated vs. non-cavitated lesionsand asactive vs. arrested lesions (Fig. 3). Fontana et al. in 2013 pointed out that the proper diagnostic process should consider the thresholds for non-surgical and surgical (i.e., restorative) interventions, risk assessment, and review of caries management interventions for caries disease management. Moreover, caries detection and management should be patient-centered, risk-based, and supported by the best available evidence, and they should consider the dentists’ clinical expertise and the patients’ needs and preferences [10].
4.1. Caries Activity
Research has tended to focus on caries activity detection as a part of the modern caries management concept. This eventually aims to personalize each dental treatment plan according to the caries activity status. An active lesion has the possibilities to progress, regress, or be arrested, while an inactive (arrested) lesion is considered to have a lesser likelihood of transition [11]. More importantly,if the inactive non-cavitated carious lesions are not regularly monitored and managed, they threaten to progress into active lesions, resulting in dentine cavities, fillings, or extractions,depending on the severity of the lesion [12]. Caries lesion activity is usually assessed using visual-tactile criteria. Several studies determined the indicators that can be used to assess caries activity,including: the presence of plaque; the location of the lesion; the presence or lack of a shiny surface; and tactile characteristics (roughness) [13, 14]. Assessment of the surface topography and texture of lesions can help in the detection of caries activity. On gentle probing, an active lesion is matte and rough, whereas an inactive carious lesion is shiny and smooth [15]. It is important to establish a standard approach to distinguish between active and inactive carious lesions. However, there are some transitional stages between active and inactive lesions thatalso necessitate the use of a reliable and valid assessment tool.
Ando et al. in 2018 used a quantitative approach to assess carious lesion activity, and their results showed that specular reflection, roughness, and fluorescence change during dehydration can differentiate between sound and demineralized enamel. In addition, reflection and fluorescence can distinguish between demineralized and remineralized enamel [16]. In another in-vitro study, Jablonski-Momeni et al. in 2018 aimed to design a new approach using a camera to detect elevated free calcium ions (photoprotein) on the carious lesion through a light signal called bioluminescence. They measured the reproducibility and accuracy of the bioluminescence system to assess the activity of carious lesions on occlusal surfaces, which showed no significant difference when compared to the visual assessment to detect the activity of carious lesions on occlusal surfaces [11]. However, this approach needs more research before being used in a clinical setting.
The Nyvad classification uses visual-tactile classification to help in the detection of caries activity by assessing the differences in tooth surface topography and lesion texture. Based on initial reliability tests, Nyvad and Baelumin 2018 proposed the Nyvad classification, which showed high reliability in detecting the activity of carious lesions in both primary and permanent teeth [14]. The Nyvad classification aims to detect caries activity during all the stages of the caries development: clinically sound surfaces; non-cavitated carious lesions; and established cavitated carious lesions. The added value by Nyvad classification is that it enables the assessment of the severity of lesions (whether they are cavitated lesions or not) as well as the assessment of lesion activity [14].
The role of biofilm microbial metabolites in the caries activity of non-cavitated carious lesions is supported by the results of the histologic study by Ricucci and Siqueira in 2020. They evaluated the presence of bacterial aggregations at the enamel-dentinal junction of teeth with whitespot lesions. Surprisingly, they found that the bacterial biofilms reached the enamel-dentinal junction of teeth with white spot lesions in both active and in-active carious lesions [17]. A recent diagnostic study showed a promising result for a more objective way to determine caries activity.It used the red fluorescence of the dental plaque microbial metabolism in determining the activity status of non-cavitated carious lesions. The study showed above 80% sensitivity and specificity. The authors were able to categorize these lesions accurately based on the red fluorescence, which will assist in the diagnosis and treatment planning of non-cavitated carious lesions [18].
4.2. Caries Detection Criteria
Since the first step in caries management is detection, it is important to know that there are multiple caries detection criteria and classification systems. The story began with Black’s Classification at the beginning of the last century [19]. However, the demands of dental treatment procedures and the development of more management modalities mandated the need for more comprehensive detection criteria and classification systems. For instance, the World Health Organization (WHO) established two indices: DMFT (D=Decayed, M=Missing, F=Filled), based on tooth level; and DMFS (D=Decayed, M=Missing, F=Filled) based on the surface [20]. However, the WHO classification does not account for non-cavitated carious lesions, which will lead to an underestimation of the caries experience.The WHO criteria have been modified to be more sensitive to non-cavitated dental carious lesions [21]. Therefore, the non-cavitated lesions were categorized as (D1), while (D2) was used for cavitated lesions confined to the enamel,and (D3) for those cavitated lesions reaching the dentin. In some cases, (D4) is used to indicate pulpally-involved cases [22].
In 2005, the International Caries Detection and Assessment System (ICDAS) was developed, presenting the most sensitive carious detection criteria based on multiple literature sources and taking into consideration all the pitfalls of the previous criteria and classification systems [23]. According to the tooth status, ICDAS has 7 different codes (from 0 to 6). The tooth needs to be air-dried for 5 seconds before being examined. Code (0) is used for a sound tooth surface with no sign of caries. Codes (1,2) are for initial caries with any distinct changes in the enamel (e.g., opacity or discoloration) but no enamel breakdown. Codes (3,4) are used for the moderate stages in which there is a white or brown spot lesion with localized enamel breakdown. The last two codes (5,6) indicate an extensive cavity with visible dentin.
4.2.1. The International Caries Classification and Management System (ICCMS™)
The International Caries Classification and Management System (ICCMS™) has been developed as a health-outcomes-focused system that aims to maintain health and preserve tooth structure. ICCMS is based on four related stages: history; classification; decision making; and management. First, the history is reviewed to categorize the individual according to the caries risk status. There are different caries risk assessment tools,such as Caries Management by Risk Management (CAMBRA) [3], the Caries-risk Assessment Tool (CAT) [24], and the Caries Risk Assessment Form created by the ADA [25]. Therefore, the patient will be classified according to the caries stage (i.e., initial, moderate, extensive) as well as to the caries activity (i.e., active, inactive). The next stage is to synthesize a diagnosis-based decision according to both the patient's level risk status and the tooth caries status. Eventually, a personalized management plan will be developed to control the status of the patient as well as to manage the caries lesions appropriately [26].
The combined use of the four elements of ICCMS™ and the International Caries Detection and Assessment System (ICDAS) is a highly reliable method to ensure a patient-centered caries diagnosis and management approach [23]. It can replace traditional lesion-centered caries detection and restoration methods. Based on that, the diagnosis and management of non-cavitated lesions (ICDAS code 1 and code 2)were considered in this review.
4.3. Caries Detection Techniques
Significant research over the last 20 years has focused on the detection of early carious lesions. The most common method of caries detection is the visual-tactile approach, which is still the gold standard for detecting carious lesions [9]. However, othernon-invasive detection methods for non-cavitated lesions were developed and found to be more effective and sensitive [27]. These non-invasive techniques for the detection of early caries include the following:
4.3.1. Laser Fluorescence
This is a useful supplemental technique used mainly to detect hidden occlusal lesions below occlusal surfaces. It displays a digital number to indicate the amount of fluorescence, which is not necessarily a measure of lesion size or depth.It can detect the organic molecules that have entered surface deposits or subsurface porosities such as carious lesions. Because laser fluorescence does not detect demineralization directly, results must be interpreted with caution, understanding how the device works and how false-positive readings can be misleading. This technique is best shown by the introduction of DIAGNOdent ® (KaVo Dental GmbH, Biberach, Germany) in the late 1990s [28].
Some studies showed that the DIAGNOdent has no significant difference when compared to the use of magnifying loupes in the detection of smooth surface spot lesions. Therefore, it was recommended to the modification of the manufacturer recommended cut-off values and the combined use of DIAGNOdent with ICDAS II to enhance its diagnostic efficiency [29, 30]
However, Alammar and Sadaf evaluated the accuracy of DIAGNOdent in detecting non-cavitated proximal carious lesions in permanent teeth when compared to bitewing radiographs. Their results showed excellent sensitivity (95%) and good specificity (89%), which were both greater than those of the bitewing radiographs in detecting enamel proximal caries lesions. DIAGNOdent showed less sensitivity (62%) in detecting dentin carious lesions. They concluded that it had higher accuracy in detecting proximal carious lesions than bitewing radiography [31]. This is in accordance with the results of another study that evaluated the accuracy of DIAGNOdent to detect occlusal non-cavitated carious lesions under fissure sealants. Its results revealed that the diagnostic accuracy of the DIAGNOdent is acceptable for use as a supplemental tool in clinical evaluation and monitoring of enamel non-cavitated carious lesions under fissure sealants [32].Based on that, DIAGNOdent can be considered to detect occlusal or proximal lesions but with caution because of its decreased sensitivity with the dentin lesions.
4.3.2. Electrical Conductance (EC)
This technique is used to show whether there is a lesion or not. It has a considerable ability to detect lesions with a low level of false positives [33].Its main limitation is that it does not show the extent or the position of the lesion, however it is likely a useful tool for the clinician if combined with other observations when deciding on an intervention or restorative treatment plan.
4.3.3. Fiber-optic Transillumination (FOTI)
This is a diagnostic tool with a beneficial clinical application in dentistry, as well as being minimally invasive and well-accepted by both patients and care providers [34]. FOTI is mainly used in caries diagnosis and has proven to be a valid indicator of the histological presence or absence of bacterially infected tooth structuresin many research studies [35]. Strassler and Pitel in 2014 claimed that it can be used as a supplemental diagnostic aid to detect anterior and posterior interproximal caries and occlusal caries. Moreover, multiple research studies showed that it can be a valid indicator of the histological presence or absence of bacteria in the tooth structure when in-vitro sections were examined under the microscope. These studies showed the same specificity and sensitivity of the FOTI when compared to radiographs [36] [34].Based on that its effectiveness is questionable especially with the uncooperative child patient.
4.3.4. Quantitative Light-induced Fluorescence (QLF)
This is based on the phenomenon of material absorbing energy at certain wavelengths and emitting light at longer wavelengths. Non-cavitated dental carious lesions have an increased porosity due to mineral loss. As a result, when the light is projected at the tooth structure, it will scatter, resulting in the loss of the tooth structure’s natural fluorescence.In contrast, a sound tooth structure will pass the light with the same wavelength. This technique enabled the detection of demineralized tooth structure through its opaque fluorescence [37].Jung et al. in 2018 designed a scoring system for the Quantitative Light-induced Fluorescence (QLF) to standardize the fluorescence properties of occlusal non-cavitated carious lesions. They assessed the visual and tactile examinations using the International Caries Detection and Assessment System (ICDAS) criteria compared to quantitative Light-Induced Fluorescence-Digital (QLF-D) image examinations. They divided the occlusal non-cavitated carious lesions into four stages, 0,1,2, and 3, based on the progression level of the lesion and the fluorescence QLF-D. Sensitivity, specificity, and Area Under the Receiver Operating Characteristics (AUROC) showed that it is excellent in detecting occlusal caries. In addition, they found admirable, reliable intra- and interexaminer agreements. Based on their results, they were able to conclude that it is possible to use and apply the scoring system to fluorescence images, which will serve as an excellent diagnostic tool for non-cavitated carious lesions [38].This standardizing technique made QLF more effective in the clinical setting as well as research setting.
4.3.5. DIAGNOcam
This is a novel technology for caries diagnosis based on Near Infrared Digital Imaging Transillumination (NIDIT). It has the potential to give various clinical indications to improve the clinical detection of caries. It is indicated mainly for the detection of proximal caries and, less importantly, for occlusal caries, fissures, and secondary caries [39]. Moreover, Tassoker and his colleagues used visual-tactile examination (ICDAS-II), DIAGNOdent pen, and DIAGNOcam to detect non-cavitated carious lesions before and after planned extraction for molar teeth and compared them to the histologic sectioning as the gold standard. They were able to conclude that the DIAGNOcam is the most accurate diagnostic method [40].More research is needed to extend the use of DIAGNOcam in the clinical situations especially with the occlusal lesions.
Based on reliable scientific evidence, the combination of the visual methods and the other diagnostic aids can accurately diagnose non-cavitated carious lesions [9]. For instance, a recentcomparison between different detection techniques of non-cavitated carious lesions showed that bitewing radiography stillhas the highest accuracy [41]. To diagnose carious lesions accurately, the detection process needs to be systematic and standardized, taking into consideration whether the carious lesion is active or not.
5. MANAGEMENT APPROACHES FOR NON-CAVITATED CARIOUS LESIONS
The management of non-cavitated carious lesions has two approaches. The invasive (mechanical) approach uses the traditional “drill and fill” concept to restore the carious lesion even though the lesion can be reversed or arrested before it is cavitated. The non-invasive approach uses preventive-directed procedures such as sealants and fluoride-containing materials [2].
5.1. Invasive Approach (Mechanical)
In the beginning, caries were diagnosed with visual, tactile, and radiographic methods,which have shown moderate specificitybut low sensitivity [42].The mechanical approach, using “drill and fill” procedures with ahigh-speed rotary cutting instrument to manage caries,has been used for decades in dentistry. Moreover, dentists have been guided for more than a century by the concept of extension for prevention, which was introduced by G. V. Black [43]. In addition, the use of a sharp instrument to detect carious lesions leads to breakage of the enamel surface and starts the cavitation of the tooth, which is not a reversible stage [44]. Most dentists usually choose to restore lesions that appear to exceed the dentino-enamel junction in the radiograph.However, most of these lesions can be treated with preventive therapy, since they are not yet cavitated. Restored teeth are more vulnerable to recurrent caries, which will decrease their longevity.As a result, a surgical approach can lead to the unnecessary removal of tooth structures and eventually lead to more extensive treatment, such as root canal therapy [4].
While considering the non-invasive or micro-invasive modalities, it is worth emphasizing that there will be cases in which the invasive approach is needed to arrest the progression of caries. The caries risk status of the patients as well as the finances, transportation, behavior, and compliance of the patients are all determinants of which approach is preferable [43].
5.2. Non-invasive Approach (Minimally or Micro-invasive)
The adoption of non-invasive approaches in the management of these lesions can preserve dental tissues, thus increasing tooth longevity [43]. Ekstrand et al. in 2012 emphasized in their study the fact that deciding on the correct option for restoring smooth surface carious lesions should be based on whether the lesion is cavitated or not. The preventive therapy for non-cavitated lesions should aim to arrest and remineralize the lesion [45].
Consequently, the non-invasive approach to manage dental caries is defined as the clinical, evidence-based prevention and cause-related approach to dental caries, along with comprehension of the histopathological carious process as well as the development of diagnostic technologies and adhesive, bioactive restorative materials [46].
Dorri and his colleagues in their Cochrane systematic review in 2015 differentiated between non-invasive and micro-invasive (minimally invasive) approaches. These treatments aim to control the biofilm through practices carried out at home by the patient (e.g.,tooth brushing,flossing) or through professionally applied treatments that enhance mineralization of the carious lesion, like topical fluoride. In contrast, the micro-invasive approach includes conditioning the tooth surface with organic acids,which will eventually cause the loss of few micrometers of tooth enamel (e.g.,sealants and resin infiltration) [2]. According to Santamaria et al. in 2017, non-invasive biofilm-control-based caries management modalities for treating carious primary teeth are becoming common, which provides potential benefits for conserving tooth structure by delaying or minimizing the need for operative procedures [47].
This is supported by the recommendation of the consensus statement released jointly by the European Federation of Conservative Dentistry, the European Organisation of Caries Research, and the German Society of Conservative Dentistry. They recommended considering non-invasiveas well as micro-invasive measures to managenon-cavitated carious lesions,while taking care to tailor the treatment plan for every patient according to his caries risk status [48].
5.2.1. Self-management and Home Measures
The process of controlling caries starts at home. This depends on three factors:a tooth-friendly diet; fluoride use at home; and regular teeth brushing to manage the biofilm. All these factors can reduce the caries risk on the individual level. Fluoridated toothpaste in particular can also arrest non-cavitated carious dental lesions [49]. The prescribed dose of 5000ppm fluoride in toothpaste was recommended by the ADA to arrest non-cavitated carious lesions only in the root surface caries of permanent teeth only.However,using a 0.2% sodium fluoride mouthrinse once per week was strongly recommended to arrest non-cavitated carious lesions on the occlusal surfaces of primary and permanent teeth [50].
5.2.2. Fluoride Varnish
The effect of fluoride varnish on primary tooth occlusal enamel caries was evaluated by Autio-Gold and Courts in 2001 in a randomized sample of children. The experiment group received fluoride varnish at the baseline and after four months, while the control group received no professional fluoride applications. Nine months later, the experiment group showed that 81.2% of lesions became inactive, 2.4% progressed and 8.2% did not change. With this statistically significant difference, the authors concluded that the fluoride varnish applications may be an effective measure in reversing active pit-and-fissure enamel lesions in the primary dentition [51].
In contrast, Johansson et al. in 2014 evaluated the effect of fluoride varnish on occlusal caries in primary molars in a split-mouth study.However, they stopped the selection of carious lesions due to the continued progression of caries, which would lead to ethical conflicts [52]. In addition, Turska-Szybka and his team found that the fluoride varnish alone showed lower results when compared to a combination of fluoride varnish with other non-invasive materials on smooth surface non-cavitated lesions [53].This can bring the use of fluoride varnish alone to manage the non-cavitated carious lesions into question especially in the occlusal lesions although, it is easily applied and more acceptable by children.
5.2.3. Acidulated Phosphate Fluoride (APF) Gel
The acidulated phosphate fluoride gel was assessed as a caries-preventive agent in a high-risk group of school children. Agrawal and Pushpanjali in 2011 conducted the study in two schools randomly selected from a list of schools catering to an underprivileged area. Children who had three or more incipient (occlusal, lingual, or buccal), cavitated primary, or secondary carious lesions were enrolled in the study. Follow-up examinations were performed at 6 and 12 months, which showed a significant difference in incipient carious lesions between the experimental and control groups. Accordingly, they suggested that a biannual APF gel application is an effective preventive measure in reversing incipient carious lesions [54].However, this was a field trial, and there might be unseen confounding factors affecting the results, which might change if the gel was applied individually. Moreover, its acidity and application technique make it not the most preferable material approach.
5.2.4. Casein Phosphopeptide-Amorphous Calcium Phosphate (CPP-ACP)
Bailey et al. in 2009, conducted a clinical trial on post-orthodontic whitespot lesions to test whether more lesions would regress when CPP-ACP paste was combined with fluoride toothpaste and supervised fluoride mouthrinse for 12 weeks. Their results showed that asignificant31% of lesions regressed with CPP-ACP paste [55]. However, Altenburger et al. in 2010 evaluated the effectiveness of CPP-ACP on the fluorescence of initial carious lesions in pits and fissures.They randomly recruited 32 participants, who showed DIAGNOdent values between 15 and 29 in premolar and molar teeth, and instructed the study group to use CPP-ACP in addition to 1450ppm fluoride toothpastedaily. The result of this trial showed significantly less laser fluorescence after 15days, while it did not significantly differ when evaluated visually [56]. Moreover, other clinical trials measured the effectiveness of CPP-ACP application in preventing dental caries in primary teeth and reversing white spot lesions afterdifferent follow-up periods, and they found that it had no significant effect when compared to the use of fluoridated toothpaste alone [57, 58].
The results of the above-mentioned studies are supported by the conclusion of the recent systematic review done by Fernández-Ferrer et al. in 2018 and by the recommendations of the ADA,which concluded thatCPP-ACP toothpaste has no positive effect on enamel lesions and discouraged its use if other measures are accessible [59, 50]. Despite these results, it could be considered as an adjunctive tool in the dentist’s box if he has no other choice.
5.2.5. Pit and Fissure Sealants
Florio et al. in 2001 and Honkala et al. in 2015 studied the efficacy of fissure sealants as a method of treatment for incipient occlusal caries. After one year, both studies found the fissure sealants showed a significantly higher arrest of caries when compared to fluoride varnish. They concluded that fissure sealants were able to arrest the progression of occlusal caries and were better at preventing caries progression than fluoride varnish alone [60, 61].
This is compatiblewith the result of a split-mouth study designed to evaluate the efficacy of infiltrating, sealing, or fluoride varnishing on occlusal surfaces with initial caries lesions. Lesions were randomized, then infiltrated with resin and varnished, sealed and varnished, or only varnished. By following up with radiographs, the investigators concluded that infiltration and sealing occlusal surfaces with initial carious lesions on primary molar teeth had high efficacy in arresting caries progression [62].
In addition, Wright et al. in 2016 reviewed the available clinical evidence regarding the effect of dental sealants for the prevention and management of pit-and-fissure occlusal carious lesions in primary and permanent molars. With moderate-quality evidence, theyfound that the participants who received sealants had a reduced risk of developing carious lesions in occlusal surfaces of permanent molars compared with those who did not receive sealants, after 7 or more years of follow-up. They concluded that sealants are effective in preventing the progression of non-cavitated carious lesions [63]. The only disadvantage of the sealant on the occlusal lesions is that it is technique-sensitive and needs close follow-up and maintenance.
The sealant has asubstantial limitation which is that it is not applicable in the proximal lesions.However, in a recent, randomized clinical trial with 2 years of follow-up, an innovative approach was used to manage proximal carious lesions using the separation and sealing techniques. The investigators aimed to seal the proximal incipient carious lesions at the same visit, using a metal separator between the proximal surfaces of the posterior permanent teeth. They measured the efficacy of the sealing in arresting caries and evaluated the acceptance of 48 patients. They pointed out that the separation enabled for more accurate diagnosis,whether there was cavitation or not. They found that the test group showed a significant caries arrest, and the separation was well accepted by the patients. Therefore, they recommended single-session separation for the diagnosis and sealing of proximal caries lesion [64]. This study might change the traditional way that we use sealants for occlusal surfaces only, but it needs more investigation. This can extend the use of sealants to proximal lesions.
5.2.6. Resin Infiltration
Caries infiltration with a resin material is a micro-invasive technique widely used to arrest non-cavitated proximal carious lesions of both primary and permanent teeth, and it is used as an alternative to invasive restorations.However, it has to involve early detection of lesions and appropriate monitoring of the caries risk. Its function is based on the penetration of low-viscosity light-curing resins, called infiltrants, into the pores within the enamel lesion. This approach fits perfectly with the concept of minimally invasive treatment because it preserves the tooth structure and it can be achieved in a single visit, as well as creating a barrier inside the lesion by replacing the mineral lost with a low-viscosity light-curing resin [45, 65-67].
In 2011, Borges et al.evaluated non-surgical interventions such as the consumption of gum containing case in phosphopeptide-amorphous calcium phosphate (CPP-ACP), resin infiltration, and fissure sealing. Although in a few cases an invasive approach is needed to arrest caries progression, the non-surgical approach generally provides potential benefits that include conserving structure by delaying intervention or minimizing operative procedures. They concluded that resin infiltration and other non-invasive methods were effective in treating non-cavitated caries lesions, and they recommended the adoption of non-invasive approaches in the management of these lesions to preserve dental tissues, thus increasing tooth longevity [43].
In 2012, Meyer-Lueckel et al. conducted a split-mouth control trial to investigate the 3-year efficacy of resin infiltration (Icon, pre-product; DMG, Hamburg) to arrest the progression of proximal non-cavitated carious lesions, as compared with placebo treatment. In their sample, they studied the lesions that extended radiographically into the inner half of the enamel up to the outer third of the dentin of permanent teeth. The patients were given general advice on oral hygiene practice and diet habits.Following up after 3 years, they concluded that the infiltration of proximal carious lesions can be an efficacious approach to reduce lesion progression [68].
A systematic review was conducted by Domejean et al. in 2015, aiming to evaluate the in-vivo scientific evidence of the ability of resin infiltration to arrest proximal non-cavitated carious lesions. They found significant differences in caries progression between their test and control groups, indicating that resin infiltration may inhibit the carious process. Therefore, they concluded that resin infiltration appeared to be an effective method to arrest the progression of non-cavitated carious lesions [69].
More evidence was found by Dorri et al. in 2015 in their systematic review and meta-analysis, which included randomized controlled trials of at least six months’ duration to compare micro-invasive treatments (i.e., sealants and resin infiltrating) for managing non-cavitated proximal dental decay in primary teeth, permanent teeth, or both, versus non-invasive measures (i.e., fluoride varnish and floss). They performed a meta-analysis, which pooled the most sensitive set of data, showing that micro-invasive treatment significantly reduced the odds of lesion progression compared with non-invasive treatment (e.g., fluoride varnish) or oral hygiene advice (e.g., to floss).They analyzed eight trials held in seven different countries that randomized 365 participants in a split-mouth design. These studies evaluated the effects of micro-invasive treatments in permanent dentition and on primary dentition, with a follow-up period ranging from one to three years. The main outcome of all these studies is the evaluation of lesion progression using radiographs. Within the limitations and the increased risk of bias, the study concluded that the micro-invasive treatment of proximal caries lesions arrests non-cavitated enamel and initial dentinal lesions and is significantly more effective than non-invasive professional treatment or advice [2]. Based on that, resin infiltration is an effective approach to control the non-cavitated proximal carious lesions but not to the occlusal lesions. However, it might not change the lesion radiolucency therefore it still could be mistakenly diagnosed as carious lesion by another dentist if no clear history.
6. CLINICAL PATHWAY GUIDELINES
The American Dental Association Council assembled an expert panel to establish a systematic review and make evidence-based clinical recommendations to arrest or reverse non-cavitated and cavitated dental carious lesions using nonrestorative treatment approaches in both children and adult patients [50]. The investigators carried out systematic research in different databases to examine the randomized controlled trials that were carried out on nonrestorative treatments of non-cavitated and cavitated dental carious lesions. The expert panel assessed the certainty in the evidence using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach.This approach was developed to assess the certainty and the quality of evidence by a widely representative group of international guideline developers to create a clear separation between the quality of evidence and strength of recommendations,as well as to evaluate the importance of outcomes of alternative management strategies. Accordingly, the process of extracting recommendations from the evidence is transparent and clear, leading to the interpretation of strong versus weak recommendations for clinicians, patients, and policymakers [70]. Based on that, Slayton et al. in 2018 formulated eleven clinical recommendations, each specific to lesion type, tooth surface, and dentition (Fig. 4). Therefore, regarding non-cavitated lesions, they provided recommendations for sealants, 5% sodium fluoride varnish, 1.23% acidulated phosphate fluoride gel, and 5,000 parts per million fluoride (1.1% sodium fluoride) toothpaste or gel. The authors recommended non-invasive treatments for non-cavitated carious lesions because these approaches have shown to be effective in arresting or reversing carious lesions [50].
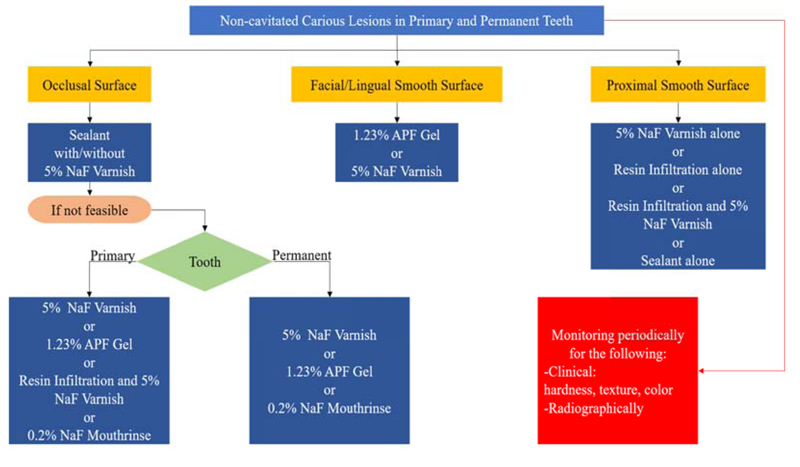
Abbreviations: NaF: Sodium Fluoride Varnish, APF: Acidulated Phosphate Fluoride
7. BENEFITS AND SAFETY OF NON-INVASIVE MANAGEMENT
According to Evans et al. in 2008,radiographic analysis revealed that the progression of lesions through enamel was usually very slow. Moreover, more access to fluoridated water and the use of fluoridatedtoothpaste made caries experience significantly less,and it can be assumed that lesion progression rates have also declined. Based on that, there is no urgency for operative intervention on discoveringnon-cavitated lesions since they potentially can be arrestedand remineralized successfully. If the caries risk of the patient is medium or low, it is beneficial and safe to defer restoration until cavitation is proved, because the negative consequences of acting on false-positive diagnoses are minimized [71]. In addition, fluoride varnishes are safe, easy to apply, and well-accepted by patients. The non-invasive approach also shows that it may offer an efficient, non-surgical alternative for the treatment of decay [51]. A caries management system that was proposed by Evans et al. in 2008 can be used by dentists. It is a strategy composed of ten noninvasive steps to arrest and remineralize early lesions. These steps are found to be empirical, clinical steps for the dentist to follow. Caries management must include consideration of the patient’s caries risk, diet assessment, plaque status, radiographic examination, the status of each lesion, patient management, clinical management, and monitoring. It includes the engagement of the patient/caregiver to tailor an informed treatment plan based on a patient-centered approach and monitoring of the patient’s oral hygiene practice and effective recall system [71].
CONCLUSION
Consideration of the comprehensive planning and management of the carious lesions, whether cavitated or not, is the most reliable way to stop caries activity. Moreover, the visual-tactile and radiographic detection of non-cavitated carious lesions can be complemented by the use of advanced, non-invasive detection tools like DIAGNOdent, fiber-optic transillumination, quantitative light-induced fluorescence, and DIAGNOcam. Accordingly, non-cavitated carious lesions can be arrested by several non-invasive techniques, which are preferred over invasive restorative options.In both primary and permanent teeth, clinicians can use sealants in addition to fluoride varnish on occlusal surfaces, fluoride varnish or resin infiltration on proximal surfaces, andresin infiltration, a fluoride gel, or varnish alone on facial or lingual surfaces to manage non-cavitated carious lesions.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


