All published articles of this journal are available on ScienceDirect.
Efficacy of Diode Laser in Treating Oral Papilloma: A Case Report
Abstract
Background:
Oral squamous papilloma is the most common lesion caused by the Human Papillomavirus (HPV). They are benign proliferation, often painless, and with cauliflower or verrucous appearance.
Objective:
The aim of this report is to describe a clinical case of oral squamous papilloma and its treatment with a high-intensity diode laser.
Case Presentation:
A 65-year-old female patient sought care at the Special Laboratory of Lasers in Dentistry (LELO), University of São Paulo, Brazil, complaining of growth of a soft tissue mass in the jugal mucosa. Based on these clinical characteristics and history, Papilloma was the initial clinical diagnosis of the lesion. Although the lesion was small in size, measuring approximately 0.5 cm, the diagnostic method used was biopsy, and for treatment, a high-intensity diode laser at a wavelength of 980 nm was used.
Conclusion:
It can be concluded that Laser Therapy can be used by dental clinicians to treat these kinds of oral lesions and should be considered as an effective alternative to conventional surgery.
1. INTRODUCTION
In the oral cavity, there are a variety of benign lesions caused by the Human Papilloma Virus (HPV), including squamous cell papilloma, verruca vulgaris, condyloma acuminatum, and focal epithelial hyperplasia, but HPV is also responsible for malignant lesions that occur in oropharyngeal cancer [1].
Oral squamous papilloma is the lesion most commonly caused by HPV, and according to the present World Health Organization classification, it is a localized exophytic proliferation with a verrucous or cauliflower-like morphology, the base of which may be sessile or pedunculated [1-7]. Diagnosis involves various techniques (cytology, biopsy, immunohistochemistry, and molecular procedures), as it can be challenging because of the clinical similarity of this entity to other epithelial lesions, such as verruca vulgaris and condyloma acuminatum [8].
The exact etiology of oral squamous papilloma is still unknown, but it has been associated with HPV 6, 11, 16 and trauma [2, 8]. The theory that associates Papillomas with HPV advocates that this virus is capable of invading the nuclei of the cells in the spinous layer, thereby inducing a series of proliferative alterations resulting in tumoral growth [2, 3]. There is no predilection for gender, and it generally occurs in patients between 30 and 50 years old. 6
They are benign proliferations of the stratified squamous epithelium, and this oral mucosa lesion may clinically exhibit a soft consistency and color varying from white to pink according to the level of keratinization and vascularization. The sites of predilection for localization include the tongue, soft palate, and uvula, more rarely, the buccal mucosa, gingiva, and lips, or other locations [1-5,7,9,10]. The differential diagnosis includes the following entities: verruca vulgaris, multifocal epithelial hyperplasia, condyloma acuminatum, and papillary squamous cell carcinoma [1, 2, 6, 7, 11].


The treatment of choice for HPV consists of complete surgical excision, including the base of the lesion and a small area of surrounding tissue to prevent recurrence [1, 3, 4, 7, 12]. This procedure can be performed with a conventional scalpel, an electric scalpel, or using a laser [1, 2, 7, 13]. The use of laser in oral surgery has become widespread over the last few decades, especially because it offers several advantages, including control of bleeding, better tissue manipulation and because it is a well-tolerated treatment [1, 5].
The present study aimed to describe a clinical case of oral squamous papilloma and its treatment with the high-intensity diode laser.
2. CASE PRESENTATION
A 65-year old woman sought treatment at the Special Laboratory of Lasers in Dentistry (LELO), University Of São Paulo, Brazil, complaining of growth of a soft tissue mass in the jugal mucosa. According to the patient’s history, two months previously, a wart-like lesion had appeared on her finger.
Clinically, the patient presented an asymptomatic, white-pink colored increase in volume in the jugal mucosa, measuring approximately 0.5 cm. On palpation, the lesion was soft and resilient. Based on these clinical characteristics and history, Papilloma was the initial clinical diagnosis of the lesion (Fig. 1).
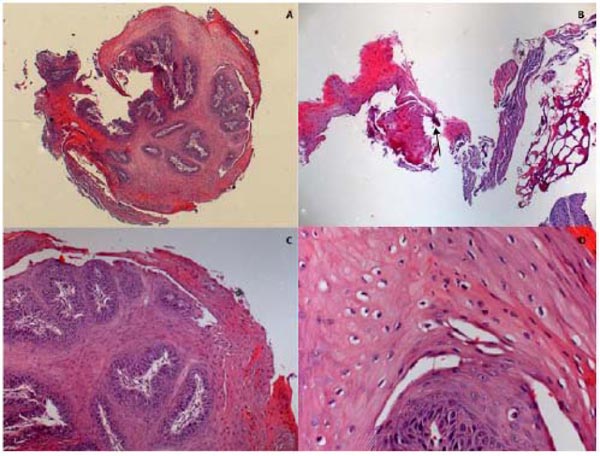
A high-intensity diode laser with a wavelength of 980 nm (Thera Lase Surgery DMC, São Carlos, Brazil) was used in a contact-mode technique under local anesthesia. Irradiation was delivered using a handpiece connected to a single-use fiber (300 μm in diameter) that was set for use in continuous-wave mode, at a power output of 1.5, for excising the lesion. The diode laser provided an optimum combination of clean cutting of the tissue and hemostasis (Fig. 2). The excised tissue was sent for histopathological study to confirm the clinical diagnosis (Fig. 3).
The patient was provided with post-treatment instructions. After a one-week follow-up the wound healed without complications and no signs of infection, and it was not necessary to use the analgesic medication after surgery (Figs. 4 and 5).
This showed that surgical laser could be used effectively, in a non-invasive procedure to treat oral papilloma. After follow-up for a period of two-years, no evidence of recurrence of the lesion has been noted.
3. DISCUSSION
Squamous papillomas are benign mucosal masses commonly induced by HPV-6 and HPV-11. The lesions generally measure less than 1 cm in size and appear as pink to white exophytic granular or cauliflower-like surface alterations. They may be found on the vermilion portion of the lips and at any intraoral mucosal site, with a predilection for the hard and soft palate and the uvula [3-5, 14, 15]. The clinical appearance, history and site of the lesion in the present case were appropriate for common identification of oral squamous papilloma. The oral pathology report confirmed the pre-surgical clinical diagnosis.

The lesions are commonly asymptomatic [4, 5], as was seen in the present case, this is why they are frequently only diagnosed during routine clinical control exams. The main therapeutic indication is surgical resection, and because of their superficiality and their clear demarcation in comparison with healthy tissues, papillomas are almost always easily removable [1, 12, 15].
Concerning the size of the biopsy, previous researches [1, 13, 15] have shown that the adequate size must be not less than 3 mm. Our biopsy was 0.5 cm in size and although it was small, it could be sent for histopathologic analysis.
The advantages of Laser therapy include minimal postoperative pain and edema, high precision in tissue destruction, excellent hemostasis, elimination of the need for sutures, and very good control of bleeding, thus leaving the surgical field free at all times [1, 2, 10, 13-16]. The findings of this study were in agreement with the above mentioned statement because no pain medication was required after the excision procedure, and wound healing was notable and rapidly achievable. This technique is also practical because diode laser devices are portable and have a significantly lower cost than other high-power lasers, namely Nd: YAG, Argon, and CO2 lasers.

Considering these advantages, the diode laser was chosen as an alternative procedure for the removal of the oral papilloma lesion in the present case.
To obtain successful results, it is important to pay attention when using a high-intensity diode laser to choose the correct power and time settings because it can generate excessive tissue coagulation, leading to severe thermal damage of the normal tissues around the lesion [1, 12, 13] Complications that may occur during treatment include perforation of the mucosa covering the lesion, necrosis, nerve damage, and glandular stenosis. The authors suggested that the fiber tip of the laser should not be held in the same place for too long, and the surface should be cooled to avoid ulceration.
In 2013, a study evaluated the therapeutic efficacy of Diode Laser therapy in treating HPV lesions. During 2001-2012, of the 170 patients, 95,4% of the cases had complete healing that occurred in the first 30 days. They concluded that the choice of the diode laser in treating HPV lesions was not only a valuable tool for their eradication, but also especially because it reduced the occurrence of relapses. Moreover, these authors showed that success could be achieved thanks to the photo-thermal effect that acted synergistically, causing irreversible damage to the diseased cells, and freeing the area of intervention from the presence of the papilloma virus.
Regarding recurrences, authors concluded the recurrence rate was low, and it usually occurred before the elapse of 15 months of follow-up. They found no differences in recurrence rates for oral squamous cell papilloma between groups after surgical treatment with the use of a surgical scalpel and two different lasers (CO2 or Er,Cr;YSGG).
CONCLUSION
The patient presented an asymptomatic, white-pink-colored increase in volume in the jugal mucosa. Although the lesion was small in size, measuring approximately 0.5 cm, the diagnostic method used was biopsy, and for treatment, a high-intensity diode laser at a wavelength of 980 nm was used. The present case report demonstrated that diode laser therapy should be considered an alternative to conventional surgery. The several advantages it offered guaranteed a safe, quick and effective surgery with excellent hemostasis, devoid of sutures, wound sterilization, no recurrences and no requirement of anesthetic for pain control during and post-intervention.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
The authors hereby declare that they have gathered all necessary consent forms from the patient showing her full authorization to use her clinical information in the journal. The patient acknowledges that her name and initials will not be published publicly, and extra efforts will be made to keep identities anonymous and confidential. Nevertheless, this anonymity cannot be absolutely guaranteed.
STANDARDS OF REPORTING
CARE guidelines and methodology were followed.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


