All published articles of this journal are available on ScienceDirect.
Evaluating the Failure of Resin-based Materials on the Proximal Cervical Dentin
Abstract
Background:
Resin-based materials are the popular restorative material in dentistry. The majority of these materials are light cured with a major disadvantage: marginal leakage.
Objective:
To evaluate the gap width of different resin-based materials at the cervical dentin when achieved mechanical force.
Methods:
Class II cavities were prepared on extracted premolar teeth with the gingival margin 1 mm below the Cementoenamel Junction (CEJ). In the first three experimental groups, three different lining materials (flowable resin composite, bulk-fill flowable resin composite, and resin-modified glass ionomer cement) were placed at the cervical dentin with a thickness of 1 mm. The rest of the cavities were restored with conventional resin composite. The other two groups were restored with conventional resin composite (control) or high viscosity bulk-fill resin composite, respectively. All groups were thermocycled and underwent vacuum pressure 2.6 KPa for 30 min in a Scanning Electron Microscope (SEM).
Results:
There was no gap formation at the cervical dentin on the external surface when restored with high-viscosity bulk fill resin composite. Almost all gaps occurred at the interface between restorative materials and the hybrid layer. The flowable bulk fill resin composite showed a significantly smaller gap width on both the external and internal surfaces compared to the other groups (p< 0.05). The resin-modified glass ionomer cement showed the largest gaps in the cervical dentin (p < 0.05).
Conclusion:
The different types of resin-based materials demonstrated a different failure of gap width under mechanical force. It clearly occurred at the restorative material-hybrid layer interface.
1. INTRODUCTION
Resin-based materials are the most popular restorative material in dentistry, due to the similarity of their color to teeth, their desirable mechanical properties, and their usefulness in preserving tooth structure. The majority of these materials are light cured, which is convenience for operators. However, the major disadvantage of these light cured resin-based materials is polymerization shrinkage, which causes shrinkage stress. Shrinkage stress accumulates in the restorative materials resulting in gap formation, post-operative sensitivity, secondary caries, and bond failure [1, 2]. Loading force from daily chewing also increases stress in the restorative materials.
Many studies have reported marginal leakage at the cervical margin of proximal cavities located on the root dentin resulting from polymerization shrinkage stress of the restorative materials [3, 4]. In these circumstances, the low modulus materials such as flowable resin composite [5-9] or low polymerization shrinkage materials such as Resin modified Glass Ionomer Cement (RMGIC) [10-12] are commonly recommended as lining materials (an intermediate layer) at the cervical margin to reduce the effect of polymerization shrinkage stress [5-9, 11-13]. In addition, the cervical margin relocation technique using lining materials is a useful procedure for conservative indirect treatment. However, there have been debates regarding exactly which materials are best suited for these techniques [14-16].
Recently, Bulk Fill resin Composite (BFCo) materials have been developed to simplify many clinical procedures. These materials have a high degree of light transmission due to the reduction of light scattering at the filler-matrix interface [17, 18]. Compared to other materials, BFCos undergo less polymerization shrinkage stress. Consequently, BFCos have been applied in bulk up to 4-5 mm, resulting in improved marginal adaptation [17, 19-21]. However, the performance of bulk fill resin composites for restoration at the cervical dentin has not been conclusively evaluated, and that is the purpose of the current study.
This study evaluated and compared the failure of five different resin-based restorative materials when used for cervical dentin restorations, based on gap width measurement. The restorations were performed with three lining materials and conventional resin composite using the class II open sandwich technique. For the hypothesis, there were no differences in the gap width of different materials at the cervical dentin.
2. MATERIALS AND METHODS
2.1. Sample Preparation
This study was approved by the Ethics Committee (IRB No. 578/59). The maxillary premolar teeth of patients age 20 years and older were collected after extraction for orthodontic reasons. These teeth were stored in 0.1% Thymol solution. Slot cavities were prepared with a 4-mm bucco-lingual width. A fissure diamond bur (#835 FG 016 Jota, Switzerland) with a high-speed handpiece was used to finish the gingival wall 1 mm cervically to the Cementoenamel Junction (CEJ) in order to keep the gingival margin on the dentin. The width of the gingival wall was 1.5 mm in the mesio-distal width. Each dental bur was replaced with a new one after five-cavity preparations. The prepared teeth were then horizontally sectioned at the occlusal surface using a low-speed water cooled diamond cutting disk to obtain tooth samples of 5-mm occluso-cervical height. A tofflemire matrix holder and the metal band were then placed around each tooth. The teeth were then randomly divided into 5 groups (N=50). Each of the five groups received different treatment, as shown in Table 1.
In Groups I, II, IV and V, the cavities were etched with 37% phosphoric acid (Scotchbond™Etchant, 3M ESPE) for 15s and then rinsed with a water jet for 20s and gently air-dried. The bonding agent (Adper™Single Bond2, 3M ESPE) was then applied according to the manufacturer’s instructions. For Group III, GC conditioning liquid was applied into the cavities for 10s, followed by rinsing with a water jet for 20s and gentle drying.
The thickness of the lining materials was 1 mm. The depth was checked by a periodontal probe and light cured for 20s with an LED light curing unit (Mini LED ACTEON, France) with light intensity at 2,000 mW/cm2. The cavities were restored incrementally in 2-mm layers for a total thickness of 4 mm and also light cured for 20s on each layer. Only in Group IV, the cavities were filled twice with 4-mm and 1-mm layers of BFCo.
After the Tofflemire matrix holder and the metal band were removed, all samples were light cured for 20s at the buccal and palatal aspects. Then all samples were stored in distilled water at 37ºC for 24h and subjected to thermal cycling for 2,000 cycles with a temperature range of 5ºC to 55ºC, a dwelling time of 15s, and a transfer time of 7s [22,23]
2.2. Evaluating the Gap Width at the External and Internal Surfaces
The samples in Groups I, II, and III were coated with two layers of nail varnish, except for 1 mm around the lining materials. The samples in Groups IV and V were similarly coated, but with 1 mm around the cervical dentin margin. All samples were immersed in 50% ammoniacal silver nitrate solution (pH=9.5) for 24 h in the dark and then thoroughly rinsed with distilled water and immersed in the photo-developing solution for 8 h under fluorescent light to reduce the diamine silver ions to metallic silver grains [24].
| Material at the Gingival Margin (1 mm thickness) | Material on the Coronal Walls (4 mm thickness) | |
|---|---|---|
| Group I (FC+Co) | Conventional flowable resin composite (Filtek Z350 XT flowable resin®, 3M ESPE) |
Nano-filled resin composite (Filtek™ Z350XT Universal Restorative, 3M ESPE) |
| Group II (BFF+Co) | Bulk fill flowable resin composite (SureFil SDR Flow®, Dentsply Caulk) |
Nano-filled resin composite (Filtek™ Z350XT Universal Restorative, 3M ESPE) |
| Group III (GI+Co) | Resin-modified glass ionomer cement (Fuji II LC capsule®, Accord) |
Nano-filled resin composite (Filtek™ Z350XT Universal Restorative, 3M ESPE) |
| Group IV (BFCo) | High viscosity bulk fill resin composite (Filtek™ Bulk fill Posterior Restorative, 3M ESPE) |
|
| Group V (Co) | Conventional nano-filled resin composite (Filtek™ Z350XT Universal Restorative, 3M ESPE) |
|
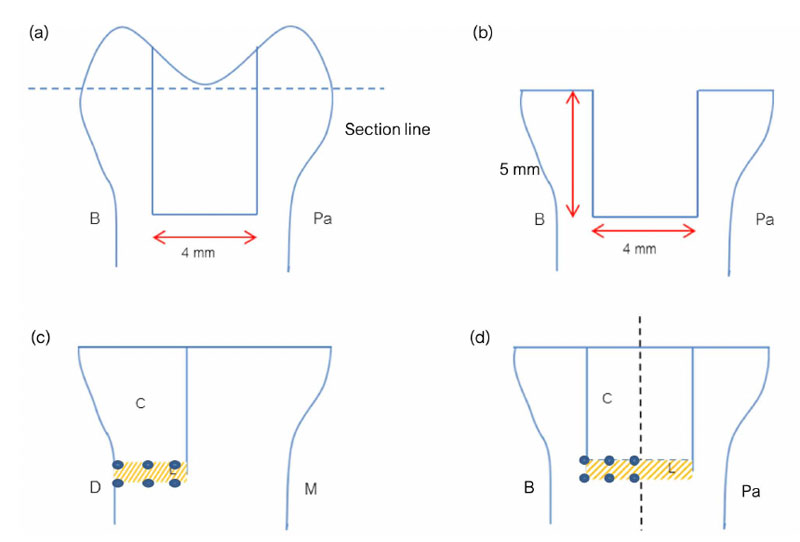
The samples were then fixed in 2.5% glutaraldehyde in 0.1 M PBS buffer at pH 7.4 for 12 h at 4ºC. After being fixed, the specimens were rinsed with distilled water for 1 min and then longitudinally sectioned in the mesio-distal direction through the center of the restorations. All specimens were dehydrated in ascending concentrations of ethanol, followed by hexamethyldisilazane, [25] and then mounted on the aluminum stubs, sputter-coated with gold, and observed under a Scanning Electron Microscope (SEM) using backscattered electron mode (magnification 1000x). In the SEM observation procedure, all specimens underwent a vacuum force of 2.6 KPa for 30 min in the specimen chamber. The gap width of each specimen was measured at the external and internal surfaces, (Fig. 1) and the silver nitrate deposition was also examined. Three photomicrographs were captured for each area to observe and measure.
2.3. Data Analysis
Using the SEM micrographs, the gap width of the external and internal surfaces of each sample was measured at three points. In the same micrographs, the distance of silver nitrate deposition along the gingival floor was measured using ImageJ software and calculated as a percentage. Normal distribution was verified with the Shapiro-Wilk test. The gap width at the cervical dentin and the gap width at the lining material-resin composite interface were measured, and the percentage of silver nitrate deposition was calculated with the Kruskal-Wallis Test and the Mann Whitney U test (p< 0.05). The mean width of the gap measured at three points along the cervical dentin within the same material was compared using the Friedman Test, followed by the Wilcoxon Signed-ranks Test (p < 0.05).
3. RESULTS
3.1. Gap Formation of the Different Materials along the Gingival Margin on the External Surface
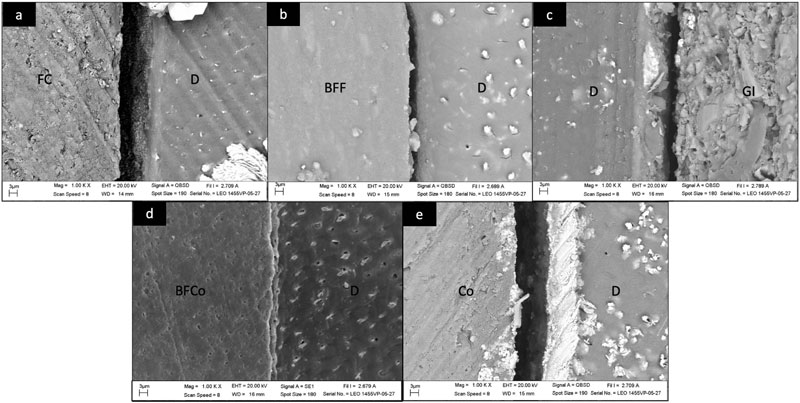
Gap formations were found at the cervical dentin on the external surface between the hybrid layer or the modified hybrid layer (Group III) and the restorative materials (Fig. 2). The hybrid layer was still in contact with the cervical dentin. The width of the gaps varied, depending on the material used, as shown in Table 2.
Group III had the largest gap width (1.63 µm) (p< 0.05), followed by Group V (1.28 µm) and Group I (1.27 µm). Group II presented a significantly smaller gap width (0.68 µm) compared to Group V (p<0.001). Samples in Group IV did not show any gap formation at the cervical dentin on the external surface.
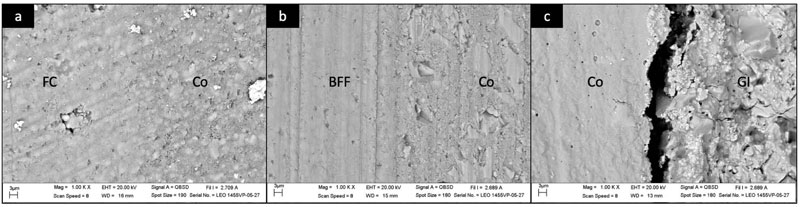
3.2. Gap Formation of Different Lining Materials to Conventional Nano-filled Resin Composite on the External Surface
Gap formation between the lining materials and the conventional nano-filled resin composite on the external surface was found only in Group III (Fig. 3). The width of the gaps is shown in Table 3.
| Type of Material Restoration | N | Gap Width (µm) |
|---|---|---|
| Mean (SD) | ||
| Group I (FC+Co) | 10 | 1.27 (0.23)a |
| Group II (BFF+Co) | 10 | 0.68 (0.16)b |
| Group III (GI+Co) | 10 | 1.63 (0.40)c |
| Group IV (BFCo) | 10 | 0.00 (0.00)d |
| Group V (Co) | 10 | 1.28 (0.28)a |
3.3. Gap Formation and Deposition of Silver Nitrate along the Gingival Margin on the Internal Surfaces
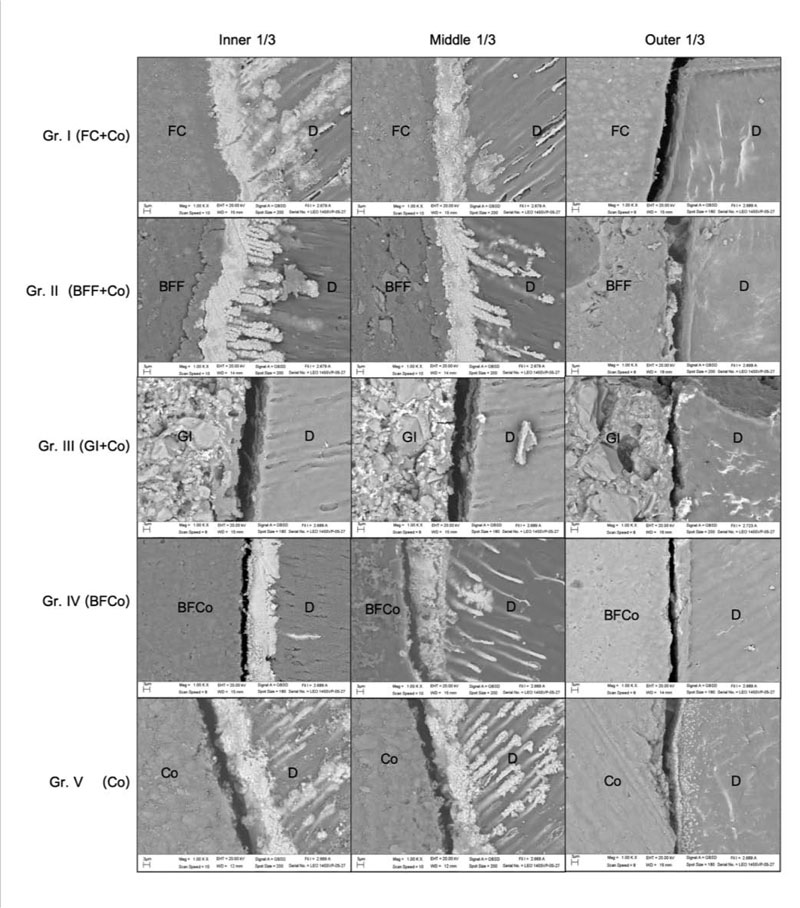
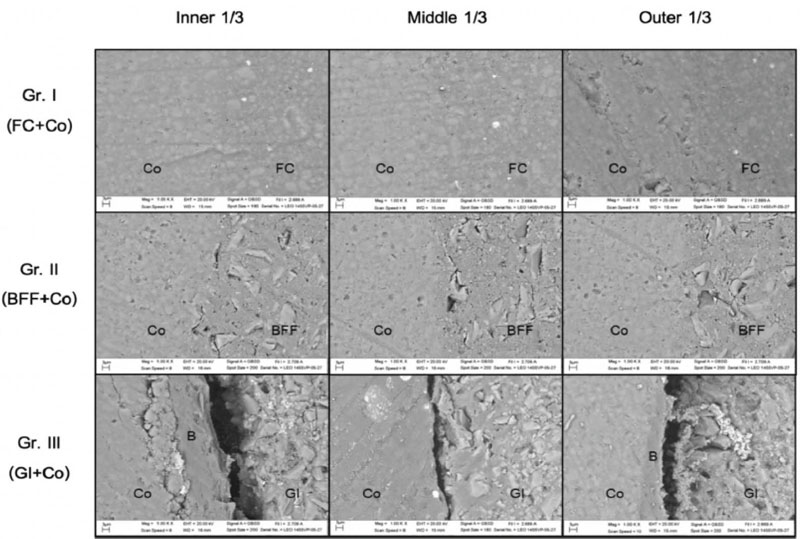
The SEM micrographs in Fig. (4) show the hybrid layer, the pattern of silver nitrate deposition and the gap formation on the internal surfaces. The inner and middle areas of the gingival wall showed thicker hybrid layers and thicker silver nitrate deposition compared to the outer area. In Group III, all samples presented a modified hybrid layer, which was clearly thinner than the hybrid layers of Groups I, II, IV, and V.
Group I and Group II shared similar patterns of silver nitrate deposition and gap formation. At the inner and middle areas, the silver nitrate was deposited on the entire width of the hybrid layer and on the resin tags penetrating the dentinal tubules. At the outer area, a thin layer of silver nitrate formed within the hybrid layer and gaps occurred between the hybrid layer and the restorative materials.
Group IV and Group V shared their own similar patterns of silver nitrate deposition and gap formation. The silver nitrate was deposited discontinuously on and within the hybrid layer. Gaps were formed between the hybrid layer and the layer of restorative materials in all three areas.
| Type of Lining Material | N | Gap Width (µm) |
|---|---|---|
| Mean (SD) | ||
| Group I (FC+Co) | 10 | 0.00 (0.00)a |
| Group II (BFF+Co) | 10 | 0.00 (0.00)a |
| Group III (GI+Co) | 10 | 0.44 (0.35)b |
| Restoration material types | N | Gap width (µm); Mean (SD) | ||
|---|---|---|---|---|
| Inner | Middle | Outer | ||
| Group I (FC+Co) | 10 | 0.00 (0.00)a,A | 0.21 (0.29)a,A | 1.83 (0.41)a,B |
| Group II (BFF+Co) | 10 | 0.00 (0.00)a,A | 0.00 (0.00)b,A | 1.21 (0.17)b,B |
| Group III (GI+Co) | 10 | 3.40 (1.83)b,A | 1.37 (1.03)c,B | 1.85 (1.54)a,AB |
| Group IV (BFCo) | 10 | 0.53 (0.64)c,A | 0.23 (0.41)ab,A | 0.56 (0.43)c,A |
| Group V (Co) | 10 | 1.85 (1.30)d,A | 0.69 (0.57)c,B | 1.86 (0.88)a,A |
The SEM micrographs of Group III show the modified hybrid layer. The silver nitrate was deposited on and within the modified hybrid layer and on the resin modified glass ionomer cement. There was a gap formation between the glass ionomer material and the modified hybrid layer in all three areas.
Gap formations were found along the gingival wall of the samples between the hybrid layer or modified hybrid layer and the restorative materials. The width of the gaps varied, depending on the restoration material and the area in the cavity, as shown in Table 4.
Considering the outer area of the gingival wall, Group IV had a significantly smaller mean gap width (0.56 µm) than the other groups (p< 0.05). In the middle area, Group II had no gap formation. Group III had the largest mean gap width (1.37 µm), which was not significantly different from the gap width of Group V (control) (p> 0.05). As for the inner area, Groups I and II did not have any gap formation. Here again, Group III had the significantly largest gap width (3.40 µm) among all the groups (p< 0.05).
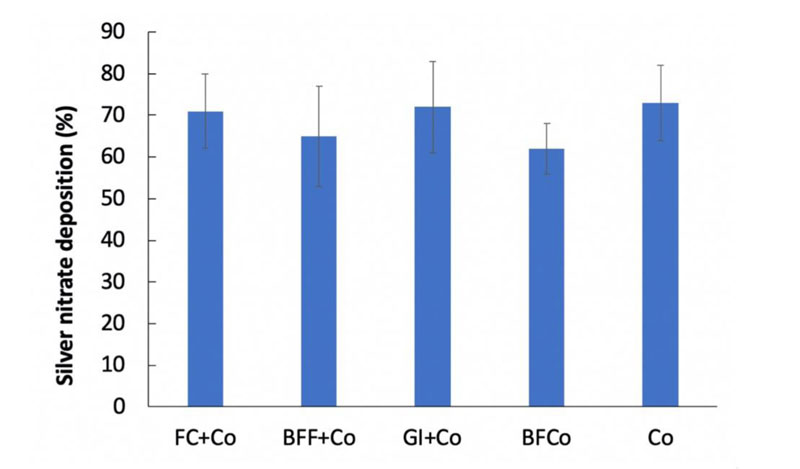
The distances of the silver nitrate depositions along the gingival wall are shown in Fig. (5), expressed as percentages of the total length. Group V (control) had the largest silver nitrate deposition (73.26%), followed by Group III (72.56%), Group I (71.46%), Group II (65.01%), and Group IV (62.66%). There was no significant difference in the distance of the silver nitrate deposition among groups (p > 0.05).
Table 5 shows correlations related to silver nitrate deposition and gap width. Silver nitrate deposition had moderate correlation (Pearson correlation 0.4-0.59) with the gap width at the outer area of the internal surface, and weak correlation (Pearson correlation 0.2-0.39) with the gap width on the external surface. The gap width at the outer area of the internal surface had a moderate correlation with the gap width on the external surface.
| Correlation between variables | p-value | Pearson correlation |
|---|---|---|
| Silver nitrate deposition – Gap width at the outer area of the internal surface | 0.003 | 0.416 |
| Silver nitrate deposition – Gap width on the external surface | 0.02 | 0.328 |
| Gap width at the outer area of the internal surface – Gap width on the external surface | 0.003 | 0.418 |
| Type of lining materials | N | Gap width (µm); Mean (SD) | ||
|---|---|---|---|---|
| Inner | Middle | Outer | ||
| Group I (FC+Co) | 10 | 0.00 (0.00)a,A | 0.00 (0.00)a,A | 0.00 (0.00)a,A |
| Group II (BFF+Co) | 10 | 0.00 (0.00)a,A | 0.00 (0.00)a,A | 0.00 (0.00)a,A |
| Group III (GI+Co) | 10 | 0.46 (0.64)b,A | 0.32 (0.52)b,A | 1.03 (1.09)b,A |
3.4. Gap Formation of Different Lining Materials to Conventional Nano-filled Resin Composite on the Internal Surface
Groups I, II, and III had lining materials (flowable resin composite, bulk fill flowable resin composite, and resin-modified glass ionomer cement, respectively) underneath the nano-filled resin composite restorations. The SEM photographs of Group I and Group II showed no gap formation between the respective restoration materials of that group. (Fig. 6). In contrast, gap formation was found in Group III, with the largest gap in the outer area (1.03 µm). The size of the gap was not significantly different among the three areas (p>0.05) (Table 6).
4. DISCUSSION
The gap formation represented the failure of the dental restorative procedure. The location of gaps corresponded in all groups, which showed at the interface between the restorative materials and the hybrid layer in the groups of resin composite materials. Besides the common concern of chemically hydrolytic degradation in the hybrid layer, this study showed the mechanical-activated failure occurring as the adhesive failure between the resin composite materials and the hybrid layer. The silver nitrate deposition in this study was the method to localize the hybrid layer in each specimen.
Regarding the gap formation on the external surface, the gap widths of the conventional nano-filled resin composite (control), resin-modified glass ionomer cement, and conventional flowable resin composite were 1.28, 1.63, and 1.27 μm, respectively. All three of these widths are larger than the diameter of microorganisms, including Streptococcus mutans (0.5-1 μm) [26], so such gaps have a high likelihood of becoming niches for microorganisms creating dental plaque later. This small gap is also difficult to get cleaned mechanically. On the other hand, flowable bulk fill resin composite had a gap width of 0.68 μm, smaller than microorganism, and there was no gap formation whatsoever in the high viscosity bulk fill resin composite group. Therefore both flowable bulk fill resin composites and high viscosity bulk fill resin composites should have a lower likelihood of plaque formation and cavity occurrence because of their smaller gap formation.
A gap occurring on the external surface and a gap occurring on the internal surface will affect the failure of resin-based materials in different ways. External surfaces are continually confronted by oral microorganisms and various chemical agents present in the oral cavity. Restoration materials should ideally provide a strong barrier to protect against their invasion. The adaptability of the restorative materials on the external surface can shut down access and accumulation of pathogens. On the other hand, a gap on the internal surface is vulnerable to hydrolytic degradation resulting in dehydration and breakdown of the adhesive materials [27]. Moreover if the gap on the internal surface extends to the external surface, this creates not only a niche for pathogens but also provides dangerous access into the pulp tissue and accelerates hydrolytic degradation of the restorative materials.
Turning to the adaptability of the resin-based materials at the internal surface, the gap width of the outer area showed a similar trend to that seen on the external surface. The flowable bulk fill resin composite and high viscosity bulk fill resin composite had the smallest gaps among all the restorative materials. Therefore, both of these materials are good candidates for use as lining materials in the open sandwich technique or the cervical margin relocation technique.
In all groups, the gap width of the external surface was smaller than that of the outer area of the internal surface. This might be the surface adhesion effect of the bonding agent. After applying the bonding agent, the air blow was applied to make a thin film of the bonding agent. Some bonding agents might accumulate adjacent to the matrix band and easily bond to the resin composite materials.
The smaller gap widths resulting from restoration with the bulk fill resin composites, either flowable or high viscosity bulk fill resin composites, are similar to some previous studies [19, 20, 22]. Bulk fill resin composites have demonstrated low polymerization shrinkage stress and a high degree of light transmission [28-30], because light scattering at the filler-matrix interface is minimized by either reducing the filler contents or increasing the filler particle size [17, 19]. In the case of SureFil SDR Flow®, modified urethane dimethacrylate is added to this resin composite’s organic component, together with photoactive reagents, thereby reducing shrinkage stress [31]. Similarly, high molecular weight Aromatic Dimethacrylate (AUDMA), as well as Additional Fragmentation Monomer (AFM), are added to Filtek™ Bulk Fill to reduce polymerization stress and strain [32]. These modifications may well account for the small gap formations obtained.
Regarding the middle and inner areas of the internal surfaces, the hybrid layer in these areas was clearly thicker than in the outer area in all groups except Group III (data not shown). Previous studies have shown that silver nitrate deposits can build up on the shrunken collagen fibers, the spaces around collagen fibers, the hybrid layer, and the hydrophilic adhesive reagent. In the current study, silver nitrate deposition occurred in one of two patterns: either spread heavily in the hybrid layer or scattered lightly in it. These two patterns of silver nitrate deposition might be influenced by incomplete infiltration of the adhesive system into the collagen layer leading to nanometer-sized spaces around the collagen fibrils within the hybrid layer [33-37].
The patterns could also be influenced by the hydrophilicity of the Single Bond 2 adhesive. Adhesives with a high percentage of hydrophilic monomers have demonstrated a high degree of permeability after polymerization, resulting in more silver nitrate deposition [38]. Single Bond 2 adhesive contains HEMA, which is a hydrophilic monomer that improves infiltration of the adhesive into moist substrates. However, HEMA also decreases the water vapor pressure, resulting in water retention at the interface. The result is that the hybrid layer acts as a hydrogel, which promotes silver nitrate deposition [39].
The resin-modified glass ionomer cement showed statistically larger gaps on both the outer and inner surfaces than the other materials. The polymerization shrinkage stress of resin modified glass ionomer cement was about 2 MPa, while it was around 4 MPa in the resin composite materials [40]. All specimens underwent the vacuum force in the specimen chamber. This increased stress in those materials by pulling the restorations from the cavities. This study showed that the bond strength of restorative materials also affects the width of the gap. The resin-modified glass ionomer cement has a chemical bond to tooth structure with the bond strength 8 MPa [41] while it was 19 MPa for the resin composite materials [42]. Therefore the bond strength might have more effect on the gap formation of the restorative materials, when undergone the mechanical force, than the polymerization stress.
At the junction between the lining materials and the nanofill resin composite, there was no gap between flowable resin composite and nanofill resin composite or between bulk fill flowable composite and nanofill resin composite, however, there was gap formation between resin-modified glass ionomer cement and nanofill resin composite on both internal and external surfaces. The fact that resin is the main component of flowable resin composite, bulk fill flowable resin composite, and nanofill resin composite allows these three materials to bond to each other. In contrast, resin-modified glass ionomer cement is a high viscosity cement containing 5% resin. Therefore the bond ability of nanofill resin composite on this glass ionomer cement was not as great as between resin-based materials.
CONCLUSION
When performing the cervical margin relocation or the class II open sandwich techniques, applying conventional flowable resin composite or resin modified glass ionomer cement at the cervical dentin margin did not improve the marginal adaptation when used with the same bonding system as conventional resin composite. On the other hand, using either low viscosity bulk fill resin composite as the lining material (SureFil SDR Flow®, Dentsply Caulk) or high viscosity bulk fill resin composite (Filtek™ Bulkfill Posterior restorative) with the bulk filled technique had improved the marginal adaptability. Conventional flowable resin composite and low viscosity bulk fill resin composite provided good adaptation on the conventional nano-filled resin composite along with the liner-resin composite interface.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Ethics Committee of Naresuan University, Thailand (IRB No. 578/59).
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors are grateful for the Graduate Student Research Grant provided by Naresuan University Graduate School and acknowledge 3M/ESPE, ACCORD Corporation Limited, and Dentsply (Thailand) for their kind support in providing the restorative materials used in this study. The authors also thank Mr. Paul Freund of Naresuan University Writing Clinic (DIALD) for editing assistance and advice on English expression.


