All published articles of this journal are available on ScienceDirect.
Perceived Practitioner Barriers to the Management of Orofacial Pain in the Kingdom of Saudi Arabia: A Cross-sectional Study
Abstract
Background:
Orofacial Pain (OFP) is a group of non-dental painful conditions affecting the oral cavity and facial area.
Objectives:
The objective of this study was to explore which barriers to manage the patient with chronic OFP as perceived by general dentists versus dental specialists and to investigate whether if professionals with degrees from their home country versus another country or number of years of professional experience differ in their perceptions.
Methods:
A closed-end questionnaire was hand-delivered to 600 participants [300 general dentists and 300 dental specialists] in four major provinces in Saudi Arabia. Demographic data were expressed as frequency. Proportional t-tests and chi-square tests were used to analyse intergroup differences. Statistical significance for all analyses was set at P-value < 0.05.
Results:
Overall, the response rate was 56.6% (340/600). Around two-thirds of the participants were general dentists (60.9%), while the remainder were dental specialists (39.1%). There was an obvious consensus by the participants that “Low payment/reimbursement” and “Lack of OFP knowledge” were among the most common barriers (85% and 83.5%, respectively). In contrast, “Legal risks” were the least frequently reported factor (38.8%). The most commonly reported barrier by general dentists was “Shortage of patients/lack of demand;” this was significantly different from the experience of dental specialists (87% vs. 72.2%; P- value < 0.01). In terms of the country of graduation or years of experience, there were no significant differences.
Conclusion:
The study demonstrates the existence of many significant barriers other than OFP knowledge, such as reimbursement, facility and demand that could present obstacles and challenges to the management of OFP by general dentists and dental specialists. Most participants believed that dentists should manage this condition and that OFP courses should be included in the dental school curriculum.
1. BACKGROUND
The role of dental practitioner has expanded from treating pain arising from only dental structures “odontogenic pain” to the management of pain in orofacial area arising from regions of the face and mouth that are not related to dental structures “nonodontogenic pain” [1, 2]. Orofacial Pain (OFP) is a group of painful conditions affecting the oral cavity and facial area, which can be somatic, neuropathic or psychological. It includes Temporomandibular Joint Disorders (TMDs), masticatory musculoskeletal pain, cervical musculoskeletal pain, neuro-vascular pain, neuropathic pain, sleep disorders related to oro-facial pain, orofacial dystonias, headaches, intraoral, intra-cranial, extracranial, and systemic disorders that cause OFP, as outlined by the American Academy of Orofacial Pain [3].
OFP can have a significantly negative impact on the quality of life directly & indirectly, as it causes functional limitation in chewing and speaking, and social and physical disability. Moreover, OFP is also associated with psychological discomfort and disability [4], and has a severe impact on daily, social, and work activities [5]. Recognition of these disorders is an essential skill for dental care providers since patients mainly seek dental care due to pain.
Questionnaire Surveys of dentists is one of the commonly used research methods to provide information on their knowledge and attitudes. There are several limitations and potential errors that need to be considered when conducting a survey: coverage error, sampling error, non-response error and measurement error [6]. The response rate of a survey is considered as an indicator of survey quality. It is not the only measure of quality. Non-response bias has grown in importance as a measure of survey quality; non-response and non-response bias are different. Response bias or nonresponse bias occurs when those who respond differently from those who have no interest in the outcome of the survey. Another significant potential error is measurement error, it occurs when inappropriate wording, design or mode of the questionnaire leads to an inaccurate answer. To reduce coverage error, every member of the survey population should have the same chance as any other of being selected into the survey sample to receive a questionnaire. Sampling errors can be reduced when the sample size is increased to ensure that the sample adequately represents the entire population. The trade-off is that the larger the population, the more difficult it is to correctly identify every member and their contact details. Resources for research are always limited. Therefore, there is a balance between the size of the sample and the costs of contacting the sample members effectively [7].
Several surveys have assessed the OFP knowledge levels among dentists, assuming that this is the only barrier to OFP practice and found different knowledge levels between General Dental Practitioners (GDPs) and dental specialists [7-12]. However, several other dentist and patient-related barriers may also exist, but no previous report has addressed this. Therefore, there is a need for a comprehensive understanding of the barriers to providing OFP care.
The objective of this study was to explore which barriers to manage patients with chronic OFP as perceived by general dentists versus dental specialists and to investigate whether if professionals with degrees from their home country versus another country or number of years of professional experience differ in their perceptions.
2. MATERIALS AND METHODS
A human research ethical approval was consulted and obtained through King Saud University, Faculty of Dentistry (KSU-FD), Riyadh, Saudi Arabia (#IR0164). A cross-sectional survey was performed using a two-part English language questionnaire that included 14 close-ended questions (appendix 1). The first section focused on socio-demographic and descriptive parameters, including age, sex, specialty, experience, type of practice, and country of graduation. The second section assessed potential barriers to the management of patients with OFP and relevant recommendations. There was a cover letter attached to the questionnaire, including information regarding the background and objective of the study. The survey was conducted from February to August 2018.
No prototype questionnaire that specifically assesses barriers to the management of chronic orofacial pain was available. Therefore, five local experts in orofacial pain and dental professionals were asked to list 5 issues that may encounter OFP practitioners to provide the service, which were used to construct the closed-ended questionnaire. Then the questionnaire was pilot tested by 10 dental practitioners to assess its feasibility and to determine the time needed to conduct the survey. Their comments were thoroughly considered in the final modification of the survey. The study was hand-delivered to 600 participants (300 GDPs and 300 dental specialists) in the four major provinces in Saudi Arabia: Riyadh, Makkah, Asir, and Eastern Province. Participants were selected randomly as representative of the Saudi dental community and included governmental hospitals, large private dental practices (> 10 dentists), and dental schools. Inclusion criteria were registered with the Saudi Commission for Health Specialties and a minimum of 2 years’ experience. Prior to data collection, written informed consent was obtained. There was no financial incentive for participants to complete the questionnaire. The study was performed with anonymized data.
Based on the pilot study, the minimum sample size was 330 participants (assuming the alpha level of 0.05 and a statistical power of 85% with an estimated proportional = 0.65). Statistical analysis was performed using SPSS software (IMP SPSS statistics, Version 22, Armonk, NY, 2013). Age, sex, specialty, years of experience, type of practice, and country of graduation responses were expressed as frequency. Proportional t-tests and chi-square tests were used to analyse intergroup differences. Statistical significance for all analyses was set at P-value < 0.05.
3. RESULTS
3.1. Participants’ Demographics
Overall, the response rate was 56.6% (340/600). Around two-thirds of the participants were GDPs (60.9%), while the remainder were dental specialists (39.1%). The response rate of GDPs was 69% (207/300), while of the specialists was 44.3% (133/300). The questionnaires were completed by 168 males (49.4%) and 172 females (50.6%). Seventy-four percent had a Saudi educational background (253/340), and around 52% of participants were < 30 years old. Overall, 71.1% (247/340) had < 10 years’ occupational experience. Participants were either employed in the governmental sector (37.3%), at academic institutes (28.2%), in private practice (20.8%), or in a combination of these. Participants’ demographics are shown in Table 1.
| Sex | Female | 172 (50.6%) |
| Male | 168 (49.4%) | |
| Age | < 30 years old | 177 (52%) |
| 30-40 years old | 105 (30.9%) | |
| > 40 years old | 58 (17.1%) | |
| Graduation Country | Saudi Arabia | 253 (74.4%) |
| Other countries | 87 (25.6%) | |
| Specialty | General practitioner | 207 (60.9%) |
| Endodontics | 23 (6.8%) | |
| Periodontics | 15 (4.4%) | |
| Orthodontics | 15 (4.4%) | |
| Pedodontics | 17 (5%) | |
| Prosthodontics | 28 (8.2%) | |
| Restorative | 12 (3.5%) | |
| Oral Surgery | 13 (3.8%) | |
| Oral Medicine | 10 (2.9%) | |
| Experience | <10 Years | 247 (72.6%) |
| 10-20 Years | 57 (16.8%) | |
| > 20 Years | 36 (10.6) | |
| Dental practice setting | Government | 127 (37.4%) |
| Academic | 96 (28.2%) | |
| Private | 71 (20.9%) | |
| Combined | 46 (13.5%) |
3.2. Perceived Barriers
Participants perceived “Low payment/reimbursement” and “Lack of orofacial pain knowledge” as the most common barriers to practicing OFP care (85% and 83.5%, respectively). In contrast, “Legal risks ” were the least reported issue (38.8). Almost equal proportions of participants considered OFP practice as being (49.4%) or not being (43.5%) “Time consuming”. Detailed responses are listed in Table 2.
| Variable | Agree | Not sure | Disagree |
|---|---|---|---|
| Lack of orofacial pain knowledge | 284 83.5% |
35 10.3% |
21 6.2% |
| Shortage of patients/lack of demand | 276 81.2% |
12 3.5% |
52 15.3% |
| Time consuming | 168 49.4% |
24 7.1% |
148 43.5% |
| Low payment /reimbursement | 289 85% |
29 8.5% |
22 6.5% |
| Legal risks | 132 38.8% |
38 11.2% |
170 50% |
| Lack of facility | 270 79.4% |
19 5.6% |
51 15% |
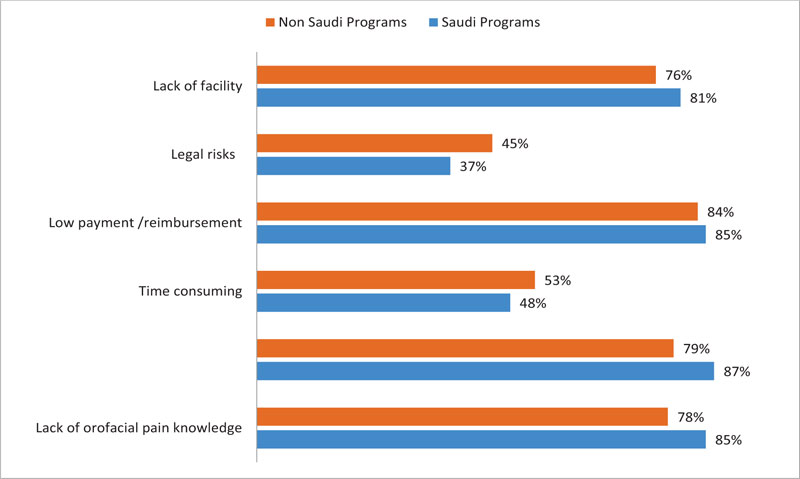
The barrier most frequently reported by GDPs was “Shortage of patients/lack of demand;” this was significantly different from the barriers experienced by dental specialists (87% vs. 72.2%; P-value < 0.01). On the other hand, the greatest barriers experienced by dental specialists were “Lack of orofacial pain knowledge” (86.5%) and “Low payment /reimbursement” (86.5%). However, no other differences were significant between GDPs and specialists. Both groups noted “Legal risks” (41.5% and 34.6%, respectively) as the least important barrier (Fig. 1).
Graduates from Saudi programs mostly reported “Shortage of patients/lack of demand” (87%) as a barrier, whereas the statement “Low payment/reimbursement” was most common among graduates from non-Saudi programs. Both graduate groups reported “Legal risks” (44.8% and 36.8% respectively) as the least common barrier. Differences between the two graduate groups were not statistically significant (Fig. 2).
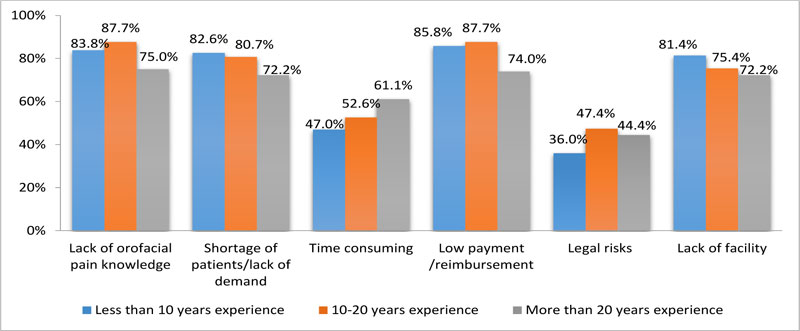
GDPs and dental specialists reported the same barrier factors, regardless of years of experience. Although the differences were not significant, “Shortage of patients/lack of demand” and “Lack of facility” were directly proportional to years of experience. On the other hand, the “Time consuming” response was in Inverse proportion to years of experience (Fig. 3). There were no other significant differences within each group related to sex, country of graduation, or year of experience.
| Variable | Agree | Not sure | Disagree |
|---|---|---|---|
| You believe dentists should manage a patient with orofacial pain | 254 74.7% |
45 13.2% |
41 12.1% |
| You believe a course of orofacial pain should be included in the dental education curriculum | 326 95.9% |
1 0.3% |
13 3.8% |
3.3. Perceived Recommendations
Agreements to the two proposed recommendations were highly significant (P-value < 0.01). Overall, 74.7% of participants agreed that dentists should manage patients with OFP, while 25.3% were not sure about or disagreed with this concept. Most GDPs and dental specialists (95.9%) in the study recommended adding a course on OFP care to dental education curricula (Table 3).

4. DISCUSSION
Pain in dentistry is usually related to oral diseases [13] or clinical procedures, such as restoration [14], implant insertion [15], miniscrew placement [16], tooth avulsion [17], combined surgical-orthodontic therapy [18], temporomandibular therapy [19]. Therefore any patient presenting with a chief complaint of toothache should be first evaluated for an odontogenic cause of pain. Odontogenic toothache occurs when there is noxious stimulation affecting the hard or soft tissue of the oral cavity. It can be identified by clinical evidence of abnormality (e.g. fracture, caries, ulcers), ability to be reproduced during the examination and can be eliminated by local anesthesia. Usually, the odontogenic toothache is localized and the quality of pain is dull, aching, or throbbing. It is also characterized by sensitivity to temperature, percussion and digital pressure [20]. However, intraoral pain may be derived from other tissues of the head and neck, which is nonodontogenic in origin. The nonodontogenic toothache is a heterotopic pain that occurs in the absence of any clinically evident cause in the oral cavity. It is a condition with multiple pathophysiological causes and may arise from musculoskeletal, neuropathic, vascular, neurovascular tissue in addition to extra-cranial, intracranial structures and systemic disorders that may cause OFP [21]. The primary distinguishing features of this kind of pain are location, severity, quality, and pattern of occurrence. For example, the neurovascular toothache is characterized by periods of total remission between episodes and generally presented as moderate to severe diffuse throbbing, pulsing, or pounding pain lasts hours to days. Neuropathic toothache, trigeminal neuralgia, is episodically described as a severe sharp, shooting, or burning pain that lasts a few seconds and is restricted to the peripheral distribution of the affected nerve branch. Muscular toothache is usually constant as deep dull aching diffuse pain with a moderate intensity that increases on function [22]. Other clinical characteristics of non-odontogenic toothache, which help to differentiate it from an odontogenic toothache are [23]:
- 1- Local provocation of the site of pain does not increase the pain, whereas local provocation at the source of pain increases the pain not only at the source but also increases the pain at the site.
- 2- Local anesthetic injection of the site of pain does not relieve the pain, while blocking the source by local anaesthesia decreases the pain at the source, as well as the site.
OFP is challenging to diagnose and manage, given the complexity of the pain mechanism and inadequate education on OFP. In this study, most participants (74.4%) believed that the management of OFP conditions forms part of dental professional responsibility, highlighting the importance of addressing this field and its barriers. Most participants (83.5%) reported a lack of OFP knowledge as a major barrier, and 95.9% recommended that OFP should gain more attention in dental curricula. This finding agreed with previous reports. For example, Klasser and Gremillion reported on OFP education in the US since 1973 [24] and found that although OFP education had improved, it still lacked in some respects. Ziegeler et al. found that 83% of German senior dental students reported that OFP was only included in a lecture on another topic [25]. Thirty percent of senior German dental students did not feel confident at all in diagnosing OFP, while 48% were somewhat confident. Klasser and Greene recommended OFP study in pre-doctoral dental education [26]. The International Association for the Study of Pain (IASP) has recently suggested an interprofessional pain curriculum outline, which included multiple topics on OFP [27]. Although the present study confirmed that lack of knowledge of OFP was a major factor, we found no differences between graduates of Saudi and non-Saudi programs. However, Al Khotani et al. found dental professional knowledge in Saudi Arabia was significantly less than that of their Swedish counterparts [10], suggesting gaps in the Saudi dental educational system.
OFP practice is undoubtedly time-consuming in both diagnosis and management; however, this was the only potential barrier showing conflict among our participant groups, with almost equal proportions agreeing (49.4%) and disagreeing (43.5%) that this is a barrier. This may be because OFP could be overlooked as a health problem that requires prioritising by the physician. In addition, years of experience might also have contributed to this conflict. We noted that participants with more years of experience tended to agree more that this was an issue. It is possible that practitioners with more years of experience have encountered more OFP patients, so that they are more aware of how time-consuming OFP practice could be. We also found that 85% of our study sample considered that “low payment /reimbursement” is a significant barrier; this may because OFP care is time-consuming and does not have as high a cost-effort ratio as other dental procedures.
Most of our participants underestimated OFP prevalence: 81.2% of participants reported that shortage of patients/lack of demand was one of the major barriers, although the specialists agreed less with this statement than did GDPs. This perception was inconsistent with the reported prevalence of various OFP conditions, which affects approximately 10%-26% of the adult population and up to 50% of the elderly [28, 29]. For example, the National Institute of Dental and Craniofacial Research reported that the prevalence of Temporomandibular Joint Disorder (TMJD) was 5%-12% [30]. A systematic review article showed that masticatory myofascial pain disorders, as one of the TMD subgroups, occurred in about 45.3% of TMD patients [31]. Neuropathic OFP is much more heterogeneous and its true prevalence is unknown. The incidence of trigeminal neuralgia varies from 4.3 to 27 cases per 100,000 per year [32, 33] with a 0.3% prevalence [33], whereas glossopharyngeal neuralgia has an incidence of 0.2-0.7 cases per 100,000 persons per year [34, 35]. Additionally, the reported prevalence of continuous neuropathic OFP conditions, such as persistent idiopathic facial pain (formerly known as atypical odontalgia, atypical facial pain, or phantom tooth pain) was 0.03%-1% in the general population [33, 36] and 2.1%-10.6% in a tertiary OFP centre [36]. Generally, the prevalence of burning mouth is between 0.7 to 5% of the population [37, 38]. In Saudi Arabia, the reported prevalence of TMJDs is 21%-34%, with no available data for other OFP disorders [39].
Another consensus response involved the lack of facility, in accordance with the current best evidence. Based on the patient’s chief complaint and individual needs, the diagnosis of OFP conditions may need advanced diagnostic tests, advanced imaging modalities, access to controlled medications, and a multidisciplinary team approach. The accessibility of facilities may require an OFP practice in a hospital setting or tertiary pain centre. This may explain the high agreement on this factor, as most participants were GDPs and most likely work in primary dental clinics, whereas dental specialists agreed less with this statement.
LIMITATIONS
The present study had several limitations. Participants were limited to dentists; however, OFP patients may express other opinions about barriers to good care. Hence future studies should investigate patients’ perceptions during the process of seeking oral care. Additionally, the percentage of senior dentists was low in this study. The years of experience was a key factor that may independently influence the barriers perceived, since senior dentists will have encountered more patients with OFP. However, the distribution by age and years of experience was consistent with the distribution of dentists in the country and the potential subjects were selected randomly in this study. Moreover, there have been few previous studies on this topic, so that the newly constructed questionnaire could not be validated; this needs to be addressed in the future. In addition, study participants were limited to four main provinces in Saudi Arabia. Although Riyadh, Makkah, Asir, and Eastern Province are the largest and most diverse in this country, it will be valuable to survey other provinces and investigate if differences across regions exist, to provide a more inclusive database of dentists for future improvements of national health care. Finally, the recruited participants were not randomly selected from different dental sectors within each province. However, the study sample was equally distributed over academic institutes, governmental sectors, and private practices, to compensate in part for bias.
CONCLUSION
OFP practice is a complex field that is further complicated by multiple barriers. Although OFP education is critical, the current study emphasises that knowledge levels among dentists were not the only barrier that requires addressing; other factors, such as reimbursement, facility, and demand, were also considered barriers. There is a misconception about the prevalence of OFP among dental professionals. OFP courses should be included in dental school curricula to train future dentists. Well-designed educational programs should be planned to target dental specialists and GDPs in Saudi Arabia to ensure the delivery of appropriate patient care at the highest international standards. In addition, there is a critical need to address issues, such as available facilities, to encourage OFP care practice.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the ethical commitee of King Saud University – Faculty of Dentistry (KSU-FD), Riyadh, Saudi Arabia (#IR0164).
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Informed consent was obtained from the participants prior to being enrolled in the study.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available from the corresponding author [E.H] upon request.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The author thanks all study participants. The author is grateful to Dr. Maha Al Hamdan, Dr. Shouq Jurays, and Dr. Hassan Khan for assistance with data collection, and to Mr. Nassr Al-Maflehi for statistical analyses.
APPENDIX 1
|


