All published articles of this journal are available on ScienceDirect.
Relationship between Helicobacter pylori and Periodontal Diseases: A Meta-Analysis Study and Systematic Review
Abstract
Objective:
The present study aimed at the evaluation of the association between H. pylori and periodontal diseases by systematic review and meta-analysis study.
Materials and Methods:
We searched databases, including PubMed, SID, Magiran, Google Scholar, and Iranmedex using the following keywords in English: H. pylori, tooth decay, oral infection, dental infection, gingival infection and periodontal diseases. Data was analyzed using a meta-analysis and random effect model. Heterogeneity of studies was assessed using the I2 index, and data was finally analyzed with STATA (Version 11.2).
Results:
Among 10 articles reviewed that included 56,334 samples, results showed that association between H. pylori and periodontal diseases was significant with OR (odds ratio) = 1.13 (95% CI: 1.04 to 1.24).
Conclusion:
The results reveal that H. pylori can be one of the main causes of periodontal diseases. Thus, a novel way should be employed for the complete management of H. pylori infections.
1. INTRODUCTION
Helicobacter pylori infections are considered a global challenge today. These bacteria are distributed worldwide. The gastric-oral and/or fecal-oral routes are the most important means by which the organism is spread [1]. Moreover, at least half the world's population is infected by H. pylori, especially in developing countries [2]. In the other direction, periodontal diseases are complicated oral diseases, which are determined by bacterial-induced inflammatory destruction of tooth-supporting tissues [3]. Periodontal diseases have many risk factors, including smoking and diabetes, moreover, several bacteria have been connected to the intensity and progress of periodontitis. Considering the oral cavity as one of the main reservoirs for H. pylori, it can play an important role in pathogenesis, re-infection and transmission of this bacterium [4].
Until now, on the basis of inconsistent findings, the relationship between H. pylori infection and periodontal disease is still controversial [5]. There are a few evidence that show some connection between H. pylori infection and periodontal disease such as dental hygiene, dental caries, gingival index, etc. [6]. On the other hand, recent studies show that H. pylori infected children have an increased risk of dental caries and prudential disease [7]. The contradictory results in recent studies may be due to small assessed populations, sample collection and inadequate detection methods for H. pylori infection. Due to those reasons, we performed a meta-analysis study in which we used cross-sectional and case-control studies to investigate the relationship between H. pylori infection and periodontal disease.
2. METHODS
2.1. Protocol and Registration
The protocol of this research registers at the Ilam University of Medical Sciences, Ilam, Iran, in the Persian language with code 968051/137.
This review was conducted based on PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [8].
2.2. Eligibility Criteria
To identify related studies, a systematic review of cross-sectional and case-control studies about the periodontal disease was performed.
To avoid bias, all steps of the study, including search, selection of studies, quality assessment, and data extraction, were conducted by two researchers independently. Any disagreement was reviewed by a third researcher.
2.3. Information Sources
To obtain related documents in English, scientific databases such as Scopus, PubMed, Science Direct, Web of Science, Springer, and Google Scholar were searched.
English MeSH keywords were used. Helicobacter pylori, tooth decay, oral infection, gingival infection, periodontal disease and also word combination of and/or operators were used as keywords.
2.4. Search
We used the following search terms to search all databases. As mentioned above, keywords including Helicobacter pylori, tooth decay, oral infection, gingival infection and periodontal disease and also word combination of and/or operators were used as keywords.
2.5. Study Selection
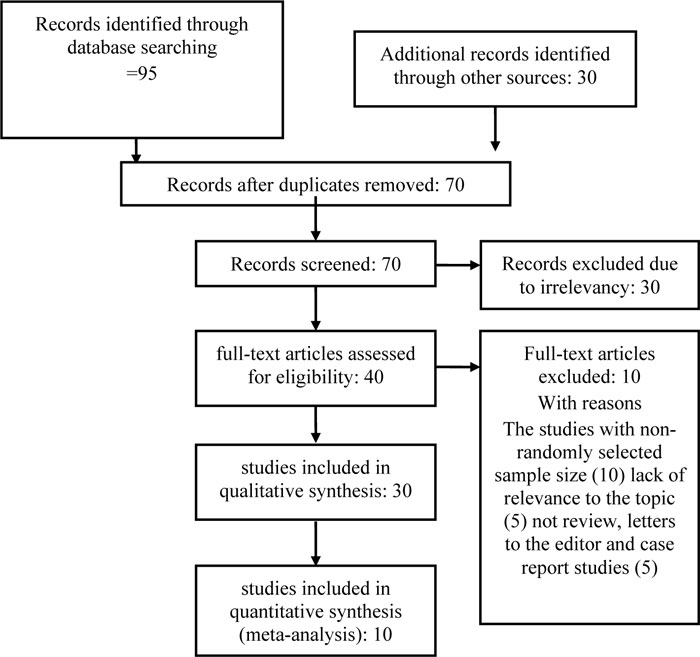
In the initial search, 125 studies probably related to periodontal diseases were selected. Seventy studies were excluded because they were duplicate papers (papers extracted by two researchers with identical titles, authors, and journal). From the remaining 55 studies, 29 cases were excluded after reading the summary and the full text due to non-relevance of the topic, and the lack of criteria and low quality. Of the remaining 26 studies, 16 cases were excluded. Finally, 10 studies were reviewed (Fig. 1).
Their data could be extracted and studies whose data could not be extracted (for various reasons such as they were duplicate papers (papers extracted by two researchers with identical titles, authors, and journal), some cases were excluded after reading the summary and the full text due to non-relevance of the topic, and the lack of criteria and low quality, etc.) were removed from the study.
2.6. Data Collection Process
In this study, a checklist of available studies was prepared. One author extracted the data from included studies and the second author checked the extracted data. The disagreement between them was solved by the third author and the final decision was the third author.
The review author agreed on the results of data extraction. The strategy used for study selection is displayed in Fig. (1). Ten studies published were eligible for meta-analysis (Table 1).
2.7. Data Items
All final papers imported to the study process were extracted by a pre-prepared checklist. The checklist includes the author's name, year of study, place of study, P-value, age, and Odds ratio and other data (Table 1).
2.8. Risk of Bias in Individual Studies
Researchers using a STROBE standard checklist [9] include 22 items. The selected studies were appraised in all aspects of methodology, including sampling methods, measurement parameters, statistical analysis and objectives of the study. The minimum and maximum scores in this checklist were 16 and 44, respectively. The papers that reached at least the minimum score were selected for the meta-analysis stage.
2.9. Summary Measures
The results of studies were combined based on the sample size, OR and its standard deviation.
2.10. Synthesis of Results
To assess the heterogeneity of the studies, the Cochran test and the I2 (heterogeneity index) were used. Due to the significant heterogeneity in the studies, random effects model was used.
2.11. Risk of Bias Across Studies
The findings are described in forest plots (the point estimations and their 95% CI). To examine publication bias, the Begg plot and regressions method were used.
2.12. Additional Analyses
P-value less than 5% was considered as a significant heterogeneity test. Sensitivity analyses were pre-specified. Statistical analyses were performed using STATA version 11.
| ID | Author | Years | Country | Age | Sample | No .of Sample | OR | CLOW | CLUPER | Study Type | P Value | Ref. |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | sonyang | 2014 | China | 46.2 | DC | 54036 | 1.05 | 1.01 | 1.09 | CS | 0.120 | 17 |
| 1-2 | sonyang | 2014 | China | 46.2 | LT | 54036 | 1.22 | 1.03 | 1.22 | CS | 0.007 | 17 |
| 2 | Gülse | 2016 | Turkey | 35.1 | PPD | 81 | 0.50 | 0.12 | 2.11 | CS | 0.442 | 18 |
| 2-2 | Gülse | 2016 | Turkey | 35.1 | PI | 81 | 1.10 | 0.17 | 7.28 | CS | 0.892 | 18 |
| 2-3 | Gülse | 2016 | Turkey | 35.1 | GI | 81 | 1.00 | 0.06 | 15.41 | CS | 0.981 | 18 |
| 3 | Yang | 2016 | China | 57.3 | PD | 212 | 2.82 | 0.57 | 13.90 | CC | - | 19 |
| 4 | Pataro | 2016 | Brazil | 37.5 | PD | 154 | 1.10 | 0.39 | 3.13 | CS | 0.076 | 20 |
| 4-2 | Pataro | 2016 | Brazil | 37.5 | CAL | 154 | 0.97 | 0.42 | 2.22 | CS | 0.210 | 20 |
| 5 | Nisha | 2014 | India | 43.6 | PD | 500 | 2.07 | 0.93 | 4.61 | CS | 0.214 | 21 |
| 6 | Rajendra | 2006 | India | 39.5 | OSF | 150 | 1.13 | 0.49 | 2.61 | CC | 0.725 | 22 |
| 7 | Lucrecia MEDINA | 2017 | Argentine | 49.0 | PD | 61 | 2.06 | 0.14 | 30.01 | CS | 0.188 | 23 |
| 8 | D.bicak | 2017 | Turkey | 10.2 | DP | 70 | 1.50 | 0.17 | 13.38 | CC | 0.500 | 24 |
| 8-2 | D.bicak | 2017 | Turkey | 10.2 | H | 70 | 1.28 | 0.86 | 1.91 | CC | 0.114 | 24 |
| 9 | Yi-Jian | 2015 | China | 44.5 | PD | 1050 | 1.47 | 0.85 | 2.56 | CS | 0.037 | 25 |
| 10 | Dayama | 2011 | India | 46.5 | OC | 20 | 1.00 | 0.03 | 30.87 | CC | - | 26 |
| 10-2 | Dayama | 2011 | India | 46.5 | OC | 20 | 0.30 | 0.06 | 1.62 | CC | - | 26 |
3. RESULTS
3.1. Study Selection
In the initial search, 125 studies probably related to periodontal diseases were selected. Some studies were excluded because they were duplicate papers. From the remaining studies, some cases were excluded after reading the summary and the full text due to non-relevance of the topic, and the lack of criteria and low quality. Finally, 10 studies were reviewed (Fig. 1).
3.2. Study Characteristics
Inclusion criteria including related papers about periodontal diseases in the English language were considered as inclusion criteria. Exclusion criteria including studies with non-randomly selected sample size, lack of relevance to the topic, letters to the editor, and case report studies were excluded.
3.3. Risk of Bias within Studies
The selected studies were appraised in all aspects of methodology, including sampling methods, measurement parameters, statistical analysis and objectives of the study. The papers that reached at least the minimum score were selected for the meta-analysis stage (This item is described in methods).
3.4. Results of Studies
In a systematic review of studies, 10 case-control and cross-sectional studies with 56,334 individuals fulfilled the inclusion criteria for the meta-analysis (Fig. 1). Oral and dental problems include patients with periodontitis diseases, dental calculus, loose tooth, recurrent aphthous stomatitis, etc.
In this regard, various studies were used, taking into account various parameters of oral diseases, the information of which could also be extracted.
Various parameters include: Dental calculus, Loose tooth, periodontal pocket depth, plaque index, gingival index, periodontal diseases, clinical attachment loss, oral sub mucous fibrosis, S: silivea, Dental biofilm Dental biofilm, Halitosis, Oral cancer
Note: Studies were conducted in which the information could be extracted.
3.5. Synthesis of Results
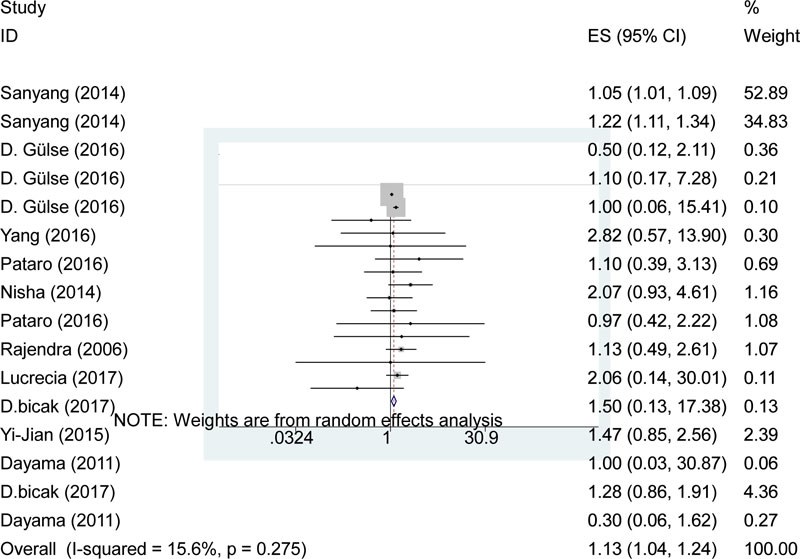
In the present study, a statistically significant difference was found between H. pylori and periodontal diseases; 1.13 (95% CI: 1.04 to 1.24). In other words, on analyzing the results of the present study, a strong association was found between the H. pylori and periodontal diseases (Fig. 2).
| Number | Author | Country |
Age Group (years) |
Publication Years | Sample | Quality Score |
|---|---|---|---|---|---|---|
| 1 | Yansong et al. | China | 46 | 2014 | 54036 | 80 |
| 2 | Gülse et al. | Turkey | 35 | 2014 | 81 | 90 |
| 3 | Yang et al. | China | 57 | 2016 | 212 | 80 |
| 4 | Pataro et al. | Brazil | 37 | 2016 | 154 | 90 |
| 5 | Nisha et al. | India | 43 | 2014 | 500 | 90 |
| 6 | Rajendra et al. | India | 39 | 2006 | 150 | 90 |
| 7 | Lucrecia MEDINA et al. | Argentine | 49 | 2017 | 61 | 80 |
| 8 | Bicak et al. | Turkey | 10 | 2017 | 70 | 80 |
| 9 | Yi-Jian et al. | China | 44 | 2015 | 1050 | 90 |
| 10 | Dayama et al. | India | 46 | 2011 | 20 | 100 |
| - | - | - | - | - | No. total: 56,334 | - |
3.6. Risk of Bias Across Studies
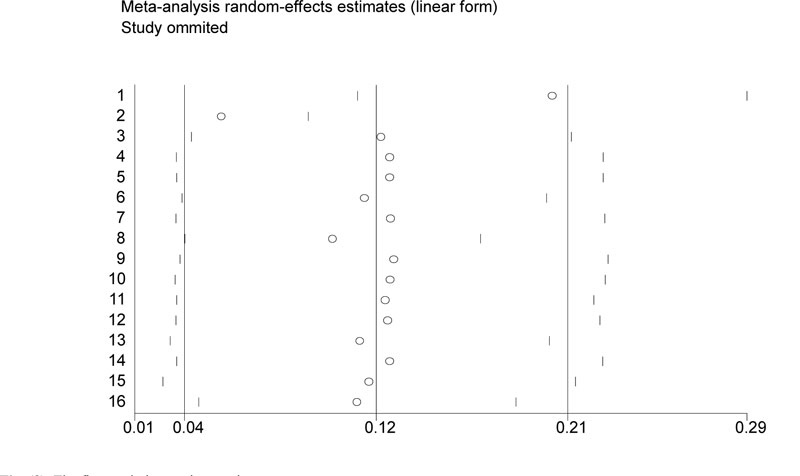
According to publication linear form figure, in this diagram, the impact of the first study on other studies will be examined. In this study, by deleting the first study, its impressive impact will be on the overall results (Fig. 3).
In this study, we used different periodontal parameters such as Periodontal Pocket Depth (PPD), the Plaque Index (PI), the Gingival Index (GI), and Clinical Attachment Loss (CAL). In other words, we have various periodontal parameters extracted from a study and we consider them as one parameter as periodontal disease parameters. Eventually, we extracted a variety of data from one study, each of which was related to one of the periodontal diseases, but all of them considered as periodontal diseases (Table 1).
3.7. Additional Result
In this study, quality assessment was also performed. Quality scores were performed for every ten studies (Table 2).
4. DISCUSSION
4.1. Summary of Evidence
It is widely accepted that one of the causes of periodontal diseases is polymicrobial in nature [10]. Periodontal disease comprises a group of inflammatory diseases of the supporting structures of teeth that occur in a susceptible group of individuals. However, the beginning and the progress of periodontal diseases are impressed by the interaction of myriad genetics, environmental, host, and microbial factors [11]. Accordingly, there are many factors as a risk factor for the host that can create an infection or oral and tooth problems for the host, such as: socioeconomic status, race and geographic region. Therefore, it has been suggested that microbial testing is used to diagnose and optimize periodontal therapy and assess its outcome [12].
Although bacteria can also arguably be an important factor and also responsible for a wide range of systemic infections as well as local infection [13].
5. LIMITATIONS
In foretime studies, the role of the oral cavity in H. pylori infection is highly controversial and confusing, due to some of them, the role of the oral cavity in H. pylori infections is significant and in some others, this condition is rejected. Although the H. pylori colonization in gastric mucosa can be one of the risk factors to develop gastric cancer, in the present study, our aims were to measure the effect of the presence of H. pylori in the oral cavity and periodontal disease.
There is a high prevalence rate of H. pylori infection in India, as a developing country, compared to developed countries (i.e., 80% by 20 years of age). In many studies, H. pylorus has been evaluated as a risk factor for many diseases, for example, Run-Tian Wang et al. found that H. pylori infection might increase the risk of stomach cancer [14]. In another study, Jing Yang et al. analyzed the association between H. pylori and periodontal disease (PD); their results showed that PD might be associated with H. pylori infection in adults; H. pylori infection may be a significant and independent risk factor for periodontal disease [15]. Damla Aksit Bıcak in 2017 showed that H. pylori can occur in the oral cavity aside and independently from the stomach; however, the high prevalence of bacteria in the oral cavities of children with gastric, an association between the presence of H. pylori and halitosis, DMFS, and pH were found [16-26].
CONCLUSION
In this study, the relationship between H. pylori infection and oral and dental problems was investigated. In summary, analyzing the results of this study, an association was found between the presence of Helicobacter pylori and oral and dental problems.
Furthermore, the results of this study indicated that H. pylori may be one of the risk factors responsible for periodontitis. This result suggests that further research is necessary to investigate their pathogenicity.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
The grant was awarded by the Ilam University of Medical Sciences, Ilam, Iran ( Grant no. 968051/137).
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


