All published articles of this journal are available on ScienceDirect.
Post-Operative Evaluation of the Intra-Oral Buccal Fat Pad Removal Technique: A Prospective Study
Abstract
Background:
In recent years, the number of procedures for buccal fat pad removal has increased. In cases of thinning of the face, bite injuries or bruxism, partial removal of the corpuscle is performed, always taking into account facial harmonization.
Objective:
The aim of the present study was to demonstrate the post-operative procedure of the removal of the BFP by pain parameters, mouth opening and presence of edema. This longitudinal cohort study was registered in clinical trials and all participants had access to the informed consent form.
Methods:
Forty BFP removal surgeries were performed with the technique of intraoral access. After the bichectomy procedure, the individuals were followed for 4, 7, 10, 15, 30, and 90 days. Visual pain scale, mouth opening measurements and clinical visual assessment were performed at all times.
Results:
We observed that the presence of edema and limited mouth opening for about 15 days were the changes most commonly found in surgeries performed. The results showed a significant decrease in painful symptoms after 15 days, regarding mouth opening, the results showed a return to normal levels after 30 days (p <0.05), the presence of edema ceased after 15 days.
Conclusion:
We conclude that the BFP removal, when performed following a precise indication, properly and with the recommendations of post-operative care, followed correctly, promotes limitation in mouth opening and painful symptoms by 15 days.
The procedure is becoming a new area for the dental surgeon, who can perform the procedure safely, reliably and with aesthetic and therapeutic results.
1. INTRODUCTION
In 1727, Heister described the buccal fat pad (BFP) as an anatomical structure independent of the face. In 1801, Marie François Xavier Bichat, a French anatomist, described an encapsulated mass of fat in the face on the outside of the buccinator muscle reporting its histological etiology of a central body and 4 extensions: buccal, pterygoid, pterygomaxillary and temporal. The body is centrally positioned and located above the parotid duct behind the zygomatic arch and is divided into 3 lobes: anterior, intermediate and posterior, in accordance with the structure of bones, ligaments and blood vessels [1].
BFP is a structure with adipose tissue, and this membrane is thin in adults, but is a prominent mass in children. The posterior lobe is located in the chewing spaces and extends to the lower orbital fissure, surrounds the temporal muscle, and extends downward to the upper edge of the mandible body. The function of BFP is to protect the sensitive anatomical structures around it, such as trauma vessels and nerves and to play a role in chewing and sucking functions, especially in children, preventing cheeks from collapsing during breastfeeding [2].
The use of a BFP-containing flap in the treatment to cover intraoral defects was first described by Egyedi in 1977, and was the first to announce the use of the buccal fat in oral reconstruction for the closure of sinus-buccal and nasal-buccal communications [3]. During the last 3 decades, it has been used as a standard procedure in the closing sinus or buccal fistulas and is a well-established tool in oral and maxillofacial surgery [4, 5].
In recent years, the number of procedures for the removal of BFP for aesthetic purposes has grown, and can be performed by both the plastic surgeon and the dentist. A patient who is a candidate for this type of surgery usually has an excessive facial circumference, and in some cases, tears the jugal mucosa tissue due to constant bites at the same site [6-8].
The anatomical position of the predominant BFP in the lower middle facial third allows manipulation to modify facial contour in aesthetic surgical procedures. Thus, there are several publications that refer to the removal and access to the oral fat pad to achieve facial balance in cases where the volume rises to a dominant position on the face [8, 9]. Although BFP removal can be performed in isolation, a variety of associated procedures were found in this systematic review, including facial lifting, submental lipoplasty, rhinoplasty, malar and mental implants, lip augmentation, masseter detachment, and botulinum toxin injection [10, 11].
Intraoral resection is performed on most of them. Although both malar atrophy and hypertrophied buccal fat may appear independently, there are patients who show both clinical signs. In these cases, the facial contour loses its oval contour and the lower thickness of the middle face dominates the malar area, resulting in a poorly defined face. The procedure is relatively safe and can be performed under local anesthesia in the office. Imaging such as ultrasound can be used to check the size of the BFP [11, 12]. The patient should always be informed of the risks and have access to the consent form, where all risks and care should be thoroughly explained. Applying postoperative care accurately, symptomatology resembles the extraction of a third molar, analgesics and anti-inflammatory drugs and sometimes antibiotics are prescribed in the first days [1].
Like every surgical procedure, there is a risk of possible complications, including bruising, partial necrosis, infection or injury to the facial nerve that results in paralysis or paraesthesia, local embolism, edema and local erythema. The aim of the present study was to report the post-operative period of 40 buccal fat pad removal surgeries performed on patients who sought care due to injuries caused by biting the jugal mucosa or aesthetic facial discontent.
2. MATERIALS AND METHODS
Forty patients who came to the UNISA Dental Clinic for the BFP removal procedure were included in this longitudinal study. All females, aged between 20 and 40 years and presenting good general health, were included. All patients received information and had access to the informed consent form that after the necessary explanations was duly completed and signed. The study was approved by the Research Ethics Committee and was registered with Clinicaltrials.gov ID: NCT03974373
Clinical parameters such as periodontal indices (probing depth, plaque index and gingival index), characteristics of the jugal mucosa, the maximum opening of the mouth and the amount of fat removed were evaluated. After detailed anamnesis and verifying the need to remove the fat ball by constant bite in the jugal mucosa or for aesthetic facial thinning, the patients were instructed to perform blood tests, fasting blood glucose and complete blood count. With the exams presenting normal levels compatible with health status, the patients were scheduled to perform the proposed therapy. At all evaluation times, pain intensity, mouth opening (in mm) and the presence of local edema were verified. For pain intensity, we used the visual analog scale (VAS) for pain (Visual Analogue Scale - VAS). In line with the numbered ends 0-10. At one end of the line, “no pain” is marked and at the other “worst pain imaginable”, so that the patient assesses and marks the pain present at that time. The measurement of mandibular movement limits was obtained with the aid of a millimeter ruler, and determined as follows: voluntary maximum opening (MVA): measurement obtained by asking the patient to open the mouth the maximum as possible.
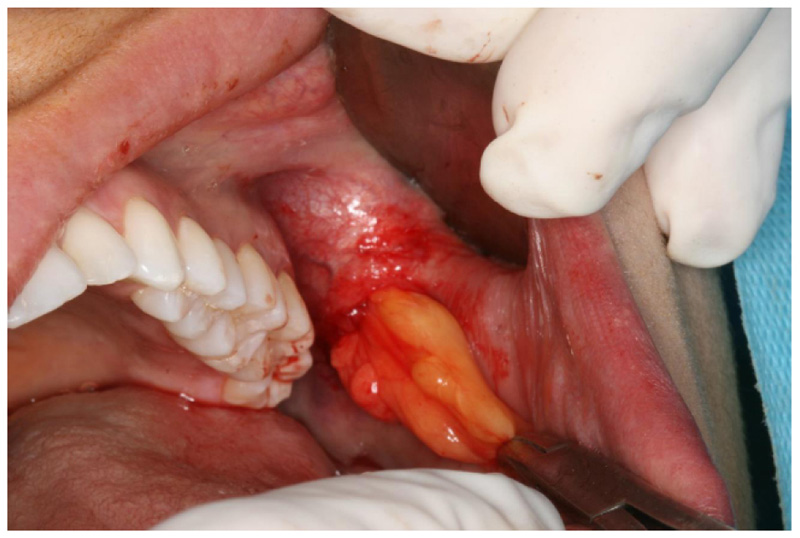
The surgical procedure was performed using the technique with intraoral access, already established in the literature [13]. The access to the Bichat fat ball was made through a small incision of no more than 3 mm (Fig. 1) in the soft tissue situated in the lower aspect of the zygomatic buttress, being careful to visualize and protect with the retractor hole Stensen's conduit. With the aid of blunt or hemostatic scissors (Fig. 2), dissection was performed, taking care to preserve the membrane surrounding the fat ball (Fig. 3). After removal of one side, the pressure was removed to remove air and the procedure was started on the opposite side, after removal of both sides, a simple suture with silk thread was performed. There were no formal indications for sending samples for anatomic and / or histological examination.
The patients were properly medicated with analgesics and anti-inflammatory and antibiotics for 5 days. Kinesio therapy tapes were applied and placed in the direction of origin for insertion of the muscles involved in the region, and changed after 4, 7 and 10 days. Intense bilateral cryotherapy in the extra-oral surgery zones for 24 to 48 hours was performed. The first return was at 4 days after the procedure and the following at 7, 10, 15, 30, and ninety days, where physical, clinical examinations, standardized photos and mouth opening measurements were performed.
The normality of distribution was verified with the Shapiro-Wilk test. The pain values, verified by the VAS scale, and the maximum mouth opening were compared with the nonparametric Wilcoxon test (p≤0.05).


3. RESULTS
Of the 40 patients operated on, all (100%) presented in the first 4 days limitation of mouth opening, painful symptoms after medication effect and bilateral edema. On the tenth day, these variables decreased in 37 patients, who continued with Kinesio® tapes for further 4 days.
Due to non-compliance with rest and food care recommendations, 3 patients (7.5%) had increased edema and unilateral swelling. In two patients (5%), it was observed that it was caused by the exaggerated physical effort; they were not obeyed as recommendations passed after BFP removal surgery and patients should follow the recommendations for rest and physical activity until the return of at least 7 days. In one patient (2.5%) due to invasion of alimentary foreign body, a popcorn grain while chewing managed to penetrate the BFP space and intervention was required to remove the invading agent. The presence of swelling, edema, flushing and pain were observed in these patients.
| Pre operative | 4 days | 7 days | 15 days | 30 days | 60 days | 90 days | |
| Mouth opening (mm) | 53.1 (±3.3) | 27.1 (± 5) |
30.4 (±3.5) |
37.5 (±2.2) | 52.8 (±3.3) | 53.2 (±3.1) | 53.2 (±3.1) |
| p value | p<0.0001 p=0.0009 p<0.0001 p<0.0001 p=0.630 p=1 | ||||||
| Visual pain scale | 0 | 5.22 (±1.4) | 4.52 (±0.84) | 2.02 (±0.15) | 0.8 (±0.1) | 0 | 0 |
| p value | p<0.0001 p=0.0073 p<0.0001 p<0.0001 p=1 p=1 | ||||||
Regarding mouth opening, we observed a larger mouth opening as the post-operative time increased, from the first evaluation (fourth day) to the fourth evaluation (30 days) there were significant increases in the opening, returning to normal after the thirtieth day (Table 1). The initial opening of the mean age was 53.1mm to 27.1mm on the fourth day, a reduction of almost 50%, 7 days after the surgery, it was 30.4mm and with no difference when compared to the time of 4 days. Significant statistical difference was observed when comparing 7 days with 15 days and 15 days with 30 days, after 30 days we can observe a return from the initial opening. The results obtained when applying the pain scale (VAS) showed pain and discomfort in the region on the fourth day with a decrease in symptoms on the seventh day and on the fifteenth day, from the thirtieth day, all patients no longer had pain or discomfort. As expected, on the fourth day, there was a significant increase in pain and discomfort, when compared to the fourth day with the seventh day, no statistical difference was observed. Differences were observed between comparisons of 7 days with 15 days and 15 days with 30 days, patients with 30 days returned to the rates observed before the BFP procedure. In the periods of 60 and 90 days, the observed data were of the absence of pain and symptoms.
4. DISCUSSION
The purpose of buccal fat pad removal is functional and aesthetic: to decrease the size of the thickness of the jugal mucosa avoiding frequent bite of the region and promote thinning in the portion below the zygomatic bone. However, this surgery is controversial for some surgeons, as this region of the face often loses fat over age and the removal of these fat bags can lead to an older appearance. Importantly, after years, the face begins to suffer a loss of fat and collagen naturally [14]. Due to this, people who undergo the procedure may need to be filled in later to regain a more youthful appearance. The literature is scarce in buccal fat pad removal procedures, although it has been performed by plastic surgeons for over 40 years, research has not been performed and studies are limited to case reports or literature reviews.
It is essential to perform a thorough clinical evaluation by the professional who will perform the surgery so that the diagnosis is accurate. Explaining to the patient, the real benefit of the procedure is mandatory. Anatomical knowledge is essential, and the use of ultrasound imaging can give evidence of the size of the buccal fat pad [12]. However, we should be careful about the use of ultrasound examination because most of the time, the fat ball is difficult to see and does not allow to determine its size and volume.
The complication rate observed in our study is similar to the few reported studies, Thomas et al., [14], observed 16% of complications and Epstein et al., [15], about 18% of these complications. Regarding the presence of trismus, hemorrhages and facial asymmetry, unlike these studies, we observed foreign body penetration and excessive physical activity in the first days after surgery.
CONCLUSION
In our study, a significant difference was observed regarding mouth opening in the first 30 days, with an increase of 2.7 opening on the fourth day, returning to normal from the thirtieth day. Patients who had to undergo foreign body removal and air drainage had a greater limitation of mouth opening and after care had a similar post-operative follow-up. Communication between the dentist and the patient is paramount so that complications such as these can be resolved quickly and satisfactorily. When applying the pain scale (VAS), we observed a significant decrease in the scale values in the first 30 days, and after this period, the patients reported no discomfort. In our study, on the fourth day, we observed an average of 5.2, such difference can be attributed to the fact that less tissue manipulation during the hydrosection technique.
The volume of GMP seems to be constant in adults, volumetric evaluations show that GMP grows between childhood and adulthood, increasing from 4,000 mm3 to 8,000 mm3 and between 20 and 50 year declines to 7,000 mm3 [11]. We observed in the operated cases that BFP is not always symmetrical, and the use of syringes to verify similar withdrawal on both sides may not mean that the patient will have facial symmetry. In the 40 cases performed, no pre-operative examinations were performed to verify the BFP. Ideally, for future studies, pre-operative imaging evaluation should be performed to define the real need for these exams. The post-operative conditions observed were not interfered by the lack of pre-operative images.
Intraoral access allows access to the fat ball without the need to move away from anatomical structures, unlike the extraoral access that presents the fat ball below muscles, arteries, nerves and veins. But even with the ease of intraoral access, there are several complications observed, including bruising, swelling, edema, partial necrosis, infection or injury to the facial nerve, exaggerated incisions may leave tissue without adequate blood supply leading to necrosis [13]. Preservation of the fascia overlying the adipose corpusum improves prognosis and shortens operative time, rupture would require suction and curettage of the area [14] and would probably lead to post-operative pain with longer symptomatology.
The lack of attention and commitment to the recommendations given for a safe and quiet post-operative period meant that 3 cases did not have the desired post-operative period. The 3 patients were immediately treated after communication and had fast resolution of the pain with corticosteroid medication and elimination of local etiological factors in one of the patients (foreign body). Patients who were affected due to physical effort had suture removed and after compression in the area and removal of air that invaded the site, a new suture was performed. Seven days after the reopening of the site, the 3 patients presented normal post-operative and oral and facial conditions compatible with patients without complications.
Among the post-operative care, we used intense cryotherapy for 48 hours, performed by the patient himself at home with the aid of thermal bags. Oral corticosteroids for 3 days to avoid excessive edema and analgesics for 5 days were prescribed. The placement of the placed Kinesio tapes assisted in the local muscle recovery. The tapes were changed 3 times on the fourth, seventh and tenth post-operative days. Post-operative care, if properly followed, leads the patient to normal feeding conditions within 15 days, we observed a clinically considerable increase in mouth opening from the tenth day, and patients should be warned about this.
The intraoral approach to BFP removal, in our opinion, is the best option when there are no associated surgical procedures; however, when a facelift procedure is indicated because the signs of aging are present, the rhytidoplasty approach may be a better alternative to the results that will be achieved. It is important to highlight the differences between the intraoral approach and the facelift procedure. In addition to the anesthesia regimen, surgical anatomy is completely different. Most complications are related to the approach chosen and not to the removal of BFP itself. Facial lifting presented major complications such as involvement of the buccal and zygomatic branches, these complications occurred due to damage to the structures involved in the facial approach [2]. Undoubtedly, if we perform both procedures simultaneously during a facelift, the final aesthetic result is much better [12]
The most important structure related to the intraoral approach is the parotid duct [2, 11]. As reported, to avoid damage to this structure, the incision is recommended about 2mm posterior to the exit of the parotid duct at the bite level or the occlusal of the upper molars [15]. Although it is a relatively old procedure, there is still a need for medium and long term studies to obtain more clinical evidence on satisfactory results. The local condition after a long time still needs clarification, BFP removal without rhytidectomy may not bring results as expected by patients causing discontent.
When the bichectomy is performed without association with any other procedure, surgery is intraoral, which is the most indicated, because the oral mucosa has better healing and leave no apparent mark. The present study, when compared with the results of other research described in the literature, shows the same complication rate. In patients with precise indication, the results contribute to a great improvement in orofacial aesthetics.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Research Ethics Committee of University Santo Amaro, Brazil and was registered with Clinicaltrials.gov ID: NCT03974373.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All patients received information and had access to the informed consent form that after the necessary explanations was duly completed and signed.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


