All published articles of this journal are available on ScienceDirect.
Modified Orthodontic Bone Stretching for Ankylosed Tooth Repositioning: A Case Report.
Abstract
Background:
Different approaches were proposed in the literature for the treatment of malpositioned ankylosed teeth. The present case report describes a modification of Orthodontic Bone Stretching Technique (OBS) for the repositioning of ankylosed teeth, consisting of dentoalveolar segmental osteotomies performed with piezoelectric instruments followed by orthodontic and orthopedic traction.
Case Report:
A 22-year-old female in good general health was referred by her orthodontist due to an infraoccluded and ankylosed maxillary upper left canine. Attempts of conventional and corticotomy-assisted orthodontic alignment of the tooth were previously performed with no success. After elevating a full-thickness flap, three osteotomies were performed by using piezoelectric inserts (Piezotome Cube, Acteon, Merignac, France). Mesial and distal cuts were full-thickness osteotomies, parallel to the long axis of the tooth, through the buccal and palatal cortical plates. The apical osseous incision was a horizontal corticotomy, involving only the buccal plate, and connecting the vertical osteotomies two millimetres over the apex of the tooth. Heavy orthodontic forces were immediately applied by using both dental and skeletal anchorage. The initial movement of the dentoalveolar segment was observed three weeks after surgery and case finishing has been completed in two months. At a one-year follow-up, the repositioned canine showed good periodontal conditions, no discoloration and positive pulp response to the electric test.
Conclusion:
Modified OBS technique was effective in repositioning an infraoccluded and ankylosed maxillary canine, providing satisfactory function and esthetics with short treatment time.
1. INTRODUCTION
Treatment time reduction is gaining increasing importance for lowering costs and enhancing patient satisfaction. In orthodontics, new approaches including corticotomies, piezocision and the use of Temporary Anchorage Device Systems (TADS) have been proposed with the aim to shorten the duration of therapy [1]. Moreover, the concept of regional acceleratory phenomenon (RAP) [2] and the development of the skeletal anchorage system using mini-screws and plates enabled the application of orthopedic force in addition to conventional orthodontic force [3]. The same techniques have been studied to facilitate dental movement even in ankylosed teeth. However, no robust scientific evidence is available on this topic due to the absence of studies with adequate sample size and long follow-up [4].
Piezoelectric bone surgery has been introduced since the beginning of this century as a promising alternative to conventional rotary instruments in performing osteotomies [5]. The mechanical action of piezoelectric devices consists of bone micronization produced by ultrasonic shock waves conducted by working tips vibrating with a frequency varying from 24 to 36 kHz. The main advantages of piezosurgery are represented by the micrometric cut (leading to thin and precise osteotomies) [6, 7], the selective action on hard tissues [8] and the positive influence on bone healing when compared to conventional rotary instruments [9, 10]. These features paved the way for a wide diffusion of piezoelectric bone surgery in various clinical applications of oral [11, 12] and craniofacial surgery [13, 14] and implantology [15, 16].
The combined action of RAP and piezoelectric surgery was recently exploited to treat ankylosed teeth with Orthodontic Bone Stretching approach (OBS) [17]. OBS is a surgically-assisted orthodontic movement consisting of partial osteotomies, without the mobilization or repositioning of the alveolar segment, combined with the application of orthodontic forces.
The present case report describes a modification of the OBS technique for the repositioning of ankylosed teeth, consisting of piezoelectric osteotomies of variable depth followed by orthodontic traction with dental and skeletal anchorage, with the aim to reduce treatment time without increasing the risk of possible complications or side effects.
2. CASE DESCRIPTION
A 22-year-old female in good general health was referred by her orthodontist due to an infraoccluded and ankylosed maxillary upper left canine. The patient underwent fixed orthodontic treatment and orthognathic surgery to correct severe skeletal Class II discrepancy and vertical hyperdivergent pattern [18]. Attempts of conventional and corticotomy-assisted orthodontic alignment of the upper left canine were previously made with no success.
Clinical examination showed multibracket orthodontic appliance in both upper and lower jaw. The upper left canine was partially erupted and infraoccluded in comparison with the adjacent teeth and with the contralateral one (Fig. 1A). Mesio-distal space between the lateral incisor and first premolar was sufficient to allow canine repositioning. The canine showed no discoloration and responded positively to the electric pulp test.
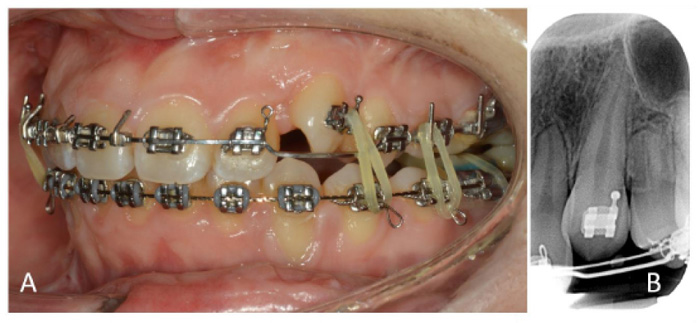
The diagnosis of ankylosis was based on the clinical assessment of mobility and percussion sound, combined with the radiographic examination. Tapping on the upper left canine produced a high percussion sound and PTV (Periotest value; Periotest, Medizintechnik Gulden, Modautal, Germany) was lower than the contralateral canine (1 vs. 9), indicating the substantial absence of mobility. Radiographic examination showed breaks in the continuity of periodontal ligament, suggesting partial tooth ankylosis.
Additionally, a periapical radiograph showed sufficient inter radicular space to perform an osteotomy between the lateral incisor and the canine. Root proximity was present between canine and first premolar, with very limited inter radicular space (approximately 1 mm). Moreover, the root was curved in the distal direction, with the apex in close proximity with the maxillary sinus floor (Fig. 1B).
2.1. Surgical and Orthodontic Procedures
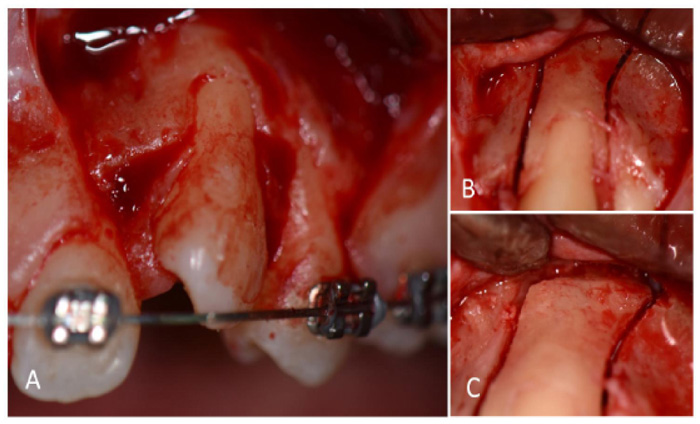
The outpatient surgical procedure was performed under local anesthesia (mepivacaine 2% with adrenaline 1:100.000). A full-thickness trapezoidal flap was elevated only on the buccal side, taking care to preserve mesial and distal papillae (Fig. 2A). Three osteotomies were performed by using piezoelectric inserts (Piezotome Cube, Acteon, Merignac, France): mesial and distal cuts were full-thickness osteotomies, parallel to the long axis of the tooth, through the buccal and the palatal cortical plates. The distal osteotomy was performed following the apical curve of the root in the distal direction (Fig. 2B). The apical osseous incision was a horizontal corticotomy, involving only the buccal plate, and connecting the vertical osteotomies two millimetres over the apex of the tooth (Fig. 2C). A careful luxation of the dentoalveolar segment was then performed with a spatula osteotome inserted in the apical corticotomy.
The buccal flap was sutured to the undetached papillae with synthetic monofilament and a mini-screw was inserted between the first and second left lower premolars. Heavy orthodontic forces were immediately applied using 0.14 Ni-Ti rounded wire (American Orthodontics, Sheboygan, WI, USA) and 1/8” 6 Oz. elastics (Lancer Orthodontics, Vista, CA, USA) between canine and lower mini-screw.
The patient was prescribed with amoxicillin (1 g tablets twice a day for 6 days), ibuprofen (600 mg tablets twice a day for 3 days) and 0.2% chlorhexidine mouth rinse (3 times a day). Sutures were removed after ten days (Fig. 3A).
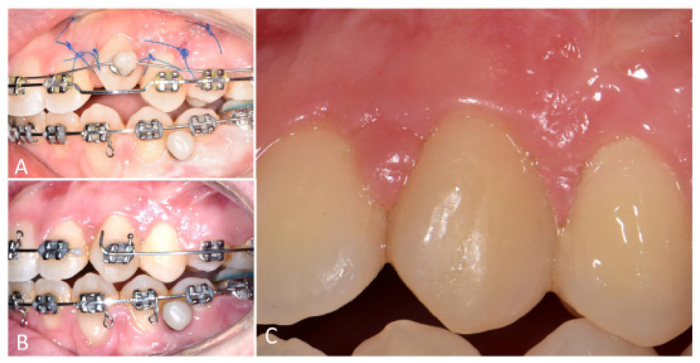
The initial movement of the dentoalveolar segment was observed three weeks after surgery. Finishing has been completed in two months by cutting the wire distal to the lateral incisor and continuing with the elastics as previously described. (Fig. 3B). After debonding, a fixed palatal retainer was applied to stabilize the mobilized dentoalveolar segment and maintain alignment of the entire upper arch.
At one-year follow-up, the repositioned canine showed good periodontal conditions, no discoloration and positive pulp response to the electric test. Treatment outcome totally fulfilled the patient’s aesthetic and functional expectations (Fig. 3C).
The present case report was presented accordingly to CARE statement (http://www.care-statement.org). The patient signed a consent form authorizing publication of clinical images and all data have been treated according to the principles of the Declaration of Helsinki as revised in Fortaleza (2013).
3. DISCUSSION
Tooth ankylosis consists of the anatomic fusion of root surface (either cementum or dentin) with the surrounding alveolar bone. This phenomenon has a multifactorial etiology (e.g. genetic factors, dental trauma), with the majority of cases occurring in deciduous molars (incidence ranging 1.5 to 9.9%) [19]. Ankylosis is quite uncommon in permanent teeth, with an incidence reported to be ten times less frequent than in deciduous [19]. Tooth ankylosis has also been reported as secondary to pre-orthodontic surgical uncovering of impacted teeth [20]. Possible explanations are related to mechanical or chemical damage (leakage of etching agents towards the cementoenamel junction during bonding of attachments) [21]. In rare cases of primary failure of eruption, ankylosis could also be the result of the application of inadequate orthodontic forces on infraoccluded teeth [22].
When ankylosis occurs during facial growth, the tooth may fail to erupt properly, remaining impacted or apical to the occlusal plane. Possible treatment options for infraoccluded ankylotic teeth in adults include, in order of increasing invasivity: i) surgical luxation [19, 21] ii) corticotomies [23] iii) orthodontic bone stretching (OBS) [17] iv) segmental osteotomies [24, 25] and v) tooth extraction. In the present case, after considering the previous failure of a corticotomy-assisted approach, we applied a modified version of OBS. OBS consists of mesial, distal and apical osteotomies involving only buccal cortical and cancellous bone preserving the palatal plate, followed by orthodontic traction [17]. We modified the original OBS protocol by performing mesial and distal full-thickness osteotomies, through the buccal and palatal cortical plates, followed by miniscrew-anchored orthodontic traction [26]. This approach derives from the previously described implant relocation technique [27-29], in which segmental osteotomies were performed to move malpositioned osseointegrated implants to a more favourable position. The use of piezoelectric bone surgery presents significant advantages in this particular application. The micrometric cut leads to improved surgical control, allowing thin and precise osteotomies in the reduced space between adjacent roots [6, 7]. The selective action on mineralized tissues of ultrasonic inserts permits to perform palatal cortical osteotomy without damaging the underlying periosteum of the undetached palatal flap, in order to preserve vascular support deriving from this side [4]. Moreover, recent studies highlighted enhanced bone healing after ultrasonic bone surgery in comparison with rotary instruments [9, 10, 30-32].
The proposed modification of OBS protocol could facilitate the mobilization of dentoalveolar segments in comparison with the original OBS technique, in which the integrity of the palatal plate is maintained when performing mesial and distal osteotomies [17]. Moreover, modified OBS preserves the apical vascular supply of the dentoalveolar segment, minimizing the risks of possible side effects inherent to the segmental osteotomies, such as loss of pulp vitality, avascular necrosis of the repositioned bone-tooth segment, marginal bone resorption and gingival recession [33].
Mesial and distal osteotomies improve the efficacy of orthodontic forces, which are applied immediately and continuously. After some days of traction, the stretching of the palatal plate allows the movement of the entire dento-alveolar segment, following Frost’s mechanostat hypothesis [34]. In addition, both surgical trauma and orthodontic traction support the onset of the regional acceleratory phenomenon, characterized by the acceleration of normal cellular activities [2]. Piezoelectric surgery, in particular, greatly increases spongious bone turnover and demineralization-remineralization dynamics, facilitating the movement of the osseous segment [35-37].
However, the positive functional and esthetic outcomes reported in the present case report should be considered with caution: the efficacy of different treatment options for ankylosed permanent front teeth is still not supported in the literature by high-level evidence studies [38]. Further, well designed randomized clinical trials are necessary to draw conclusions and suggest guidelines for the management of these challenging clinical situations.
CONCLUSION
The proposed modification of OBS could facilitate ankylosed tooth repositioning in comparison with the original technique, where the palatal plate is not interrupted by mesial and distal osteotomies. Modified OBS preserves the apical vascular supply of the dentoalveolar segment, minimizing the risks of possible complications such as loss of pulp vitality, avascular necrosis of the repositioned bone-tooth segment, marginal bone resorption and gingival recession.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for the publication of this case report, including accompanying images.
STANDARD FOR REPORTING
CARE guidelines and methodology were followed to conduct the study.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


