All published articles of this journal are available on ScienceDirect.
Orthodontic Management of a Mandibular Double-tooth Incisor: A Case Report
Abstract
The presence of a double-tooth requires specific complex management due to the need for differential diagnosis and following treatment choices. The aim of this report was to present a rare case of a geminated mandibular lateral incisor, treated with an orthodontic approach.
A Caucasian 10.9-year-old girl presented a lower right double-tooth incisor, with a class 1 molar and a class 2 cuspid tendency on both sides. The upper arch was constricted as shown by bilaterally tendencies to cross-bite, a slightly lower midline deviation was reported and a lack of space for all four permanent cuspids was confirmed also by the panoramic X-ray.
In the lower arch, there was a severe crowding of about 14 mm and a buccally ectopic left canine. Overbite was normal and Overjet minimally increased.
The double-tooth was identified like a geminated tooth, for the presence of one root and one pulp canal of increased size, as shown by the radiographic examinations.
The anomalous tooth was managed with an orthodontic approach associated with a progressive stripping to reshape the crown. A two-phase treatment plan was performed, based on first maxillary expansion and lip bumper and then fixed appliances, in order to achieve a proper occlusion and a better aesthetic.
1. INTRODUCTION
Double-tooth is generally used to define fusion or gemination, two dental developmental abnormalities, which may require treatment for aesthetic, orthodontic, or functional reasons [1, 2]. Fusion is defined as the union between the dentin and/or enamel of two or more separated tooth germs and its prevalence, in the permanent dentition, is about 0.1% [3-5].
The aetiology is uncertain, but trauma, diseases, or genetics may be considered as possible causes [6-12]. According to the tooth development stage at the time of union, dental fusion can be partial or total and it may occur between the teeth of the same dentition or between supernumerary teeth [9, 10, 12].
In most cases, the fused teeth show an anomalous size and shape of the crown and are characterized by separated roots, distinct pulp chambers, and two independent endodontic systems [7]. A particular form of fusion is the concrescence that may occur even before the eruption of teeth involving only the roots of two adjacent teeth with the fusion of the cementum [8].
In the clinical situation, fusion and gemination are represented in different ways. The first appears as a congenitally missing tooth, whereas in gemination, the number of teeth is normal and provided the double-tooth is counted as one unit [9]. Gemination, also named twinning, is defined as an attempt of the tooth bud to divide. In most cases, the division is incomplete and it ends in a single root characterized by only one root canal, but two completely or incompletely separated crowns [7]. The prevalence of geminated teeth is about 0.6% in primary dentition and 0.1% in the permanent one [10, 11].
There are no sex differences, but geminated teeth are usually found in the upper arch, whereas fusions in the lower one [13, 14]. No symptoms related to geminated or fused teeth are found, even if the presence of deep fissures may predispose them to dental caries and periodontal disorders [15-20].
Thus, based on the requirements of the situation, different treatment choices can be implied [5]. The aim of this case report is to show a rare case of a geminated mandibular lateral incisor treated with an orthodontic approach.
2. CASE REPORT
2.1. Diagnosis
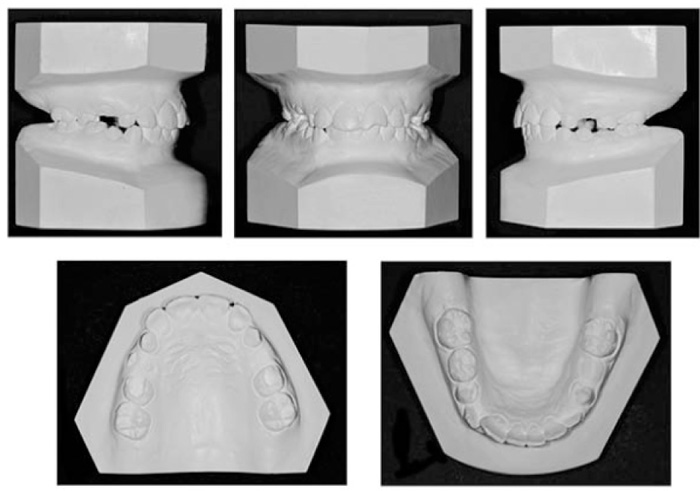
The patient was a 10.9-year-old Caucasian girl in late mixed dentition with the mandibular right lateral incisor showing macrodontic and abnormal crown morphology (Fig. 1). Her mother was really worried and complained of an unpleasant appearance of the lower front teeth.
Clinical examination revealed a class 1 molar with a class 2 cuspid tendency on both sides, the overbite was normal, whereas the overjet was minimally increased, the maxillary arch presented a bilateral tendency to crossbite with a slightly lower midline deviation (Fig. 2).
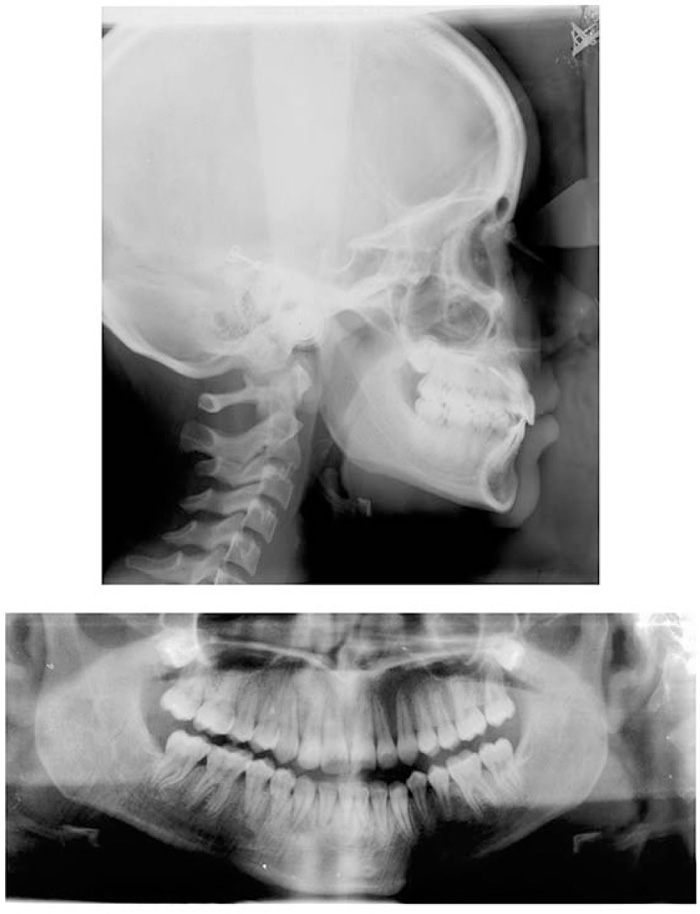
The lateral cephalometric evaluation revealed a skeletal class I (ANB = 4°) with a meso-facial growth pattern (SN-GoMe = 32°), normal inclination of the upper incisors (I/SN = 101°), and proclined mandibular incisors (IMPA = 102°) (Fig. 3A).

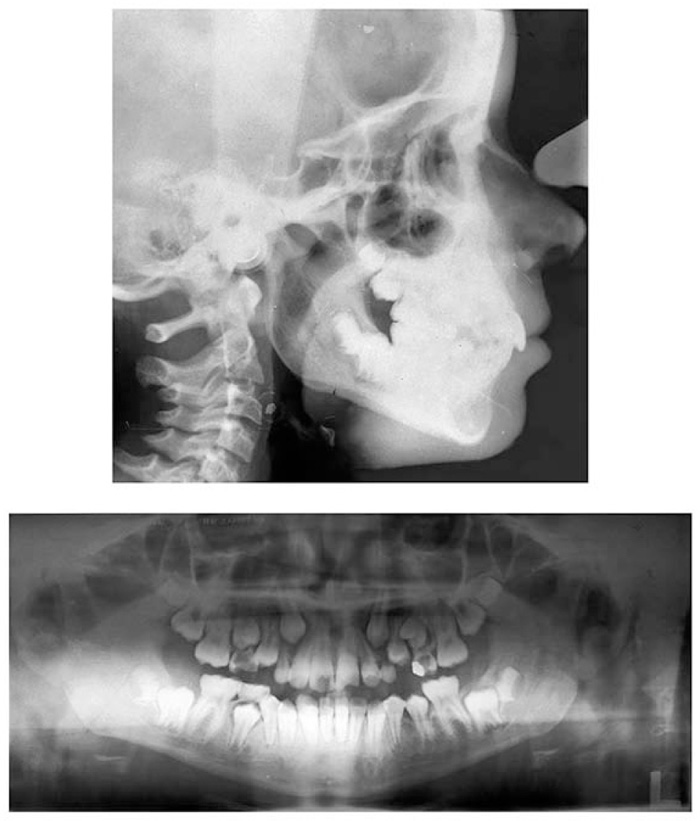
A: Lateral cephalogram and tracing; B: Panoramic radiograph.
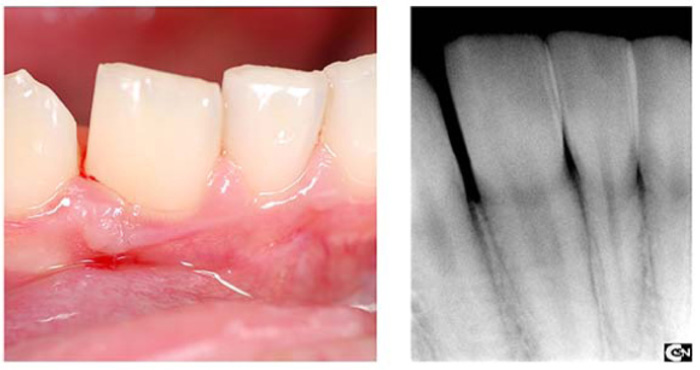
In the upper arch, there was a lack of space for the permanent cuspids confirmed also by the panoramic X-ray (Fig. 3B) while a severe crowding of about 14 mm was observed in the lower arch due to both the double-tooth and the lower incisor proclination. The upper left central incisor was broken, the lower right lateral incisor was a double-tooth, and the lower left canine was buccally ectopic. Clinically, the anomalous tooth showed a macrodontic and abnormal crownmorphology, with a mesiodistal width of 9.5 mm and a buccal and palatal groove dividing the crown into mesial and distal segments. The profile was biprotruded although with a normal value of the nasolabial angle. Oral hygiene was poor. The panoramic X-ray showed that the mandibular right lateral incisor had one root and one pulp canal of increased size, suggesting that the double-tooth was probably a geminated tooth Fig. (3B).The other teeth were in normal size and shape and their number was not reduced, confirming the diagnosis of gemination, although the differential diagnosis of fusion could not be ruled out. No dental anomalies or hereditary diseases were found in her family history.
2.2. Treatment Objectives
The consent to process personal data and photographs was obtained by the patient and her parents. The problem list of this patient included class 2 cuspid tendency correction, overjet improvement, upper arch expansion both to solve the cross-bite tendency and to promote the cuspid eruption, lower midline correction, lower crowding solving, smile and profile improvement. However, the main problem was to decide how to treat the double-tooth.
2.3. Treatment Alternatives
Before starting, the following alternatives were considered:
(1) Treatment in two phases. The first phase was interceptive and included a rapid maxillary expansion in the upper arch and a lip bumper in the lower arch. The second phase was performed with fixed appliances and a transpalatal arch. This option offered several advantages, solving the cross-bite tendency, facilitating the cuspid eruption, correcting the lower midline, improving the lower crowding and the smile. The disadvantages were the greater length of the treatment in two phases, leaving, at least partially, the lower incisor proclination.
(2) Treatment in one phase with the extraction of premolars (e.g. 1.4, 2.4, 3.4, 4.4).
This option solved the class 2 cuspid tendency, improved the overjet, corrected the lower incisor proclination, and improved the facial biprotrusion. The disadvantage was to be a more invasive treatment, that, unlike the first option, could not be interrupted.
(3) Treatment with or without extractions in adult age.
(4) No treatment at all.
2.4. Geminated Tooth Treatment Alternatives
Before starting treatment, the following options for solving the anomalous shape of the mandibular right lower incisor were considered:
(1) Coronoplasty with stripping to remove the excessive amount of enamel.
(2) Endodontic and prosthetic treatment aimed to give a better shape to the tooth with a prosthetic crown. This option could be considered only if a root canal treatment was needed after the reshaping, considering the young age of the patient and the increased size of the pulp chamber.
(3) Surgical sectioning off a segment of enamel, followed by its extraction. This option, also, could require an endodontic treatment after the extraction.
(4) Extraction of the geminated tooth to solve the severe anterior crowding, partially due to the lower incisor proclination, accepting the presence of only three lower incisors with a lower midline deviation.
(5) Extraction of the geminated tooth and its replacement with an implant.
(6) No treatment if required by the patient's parents.
2.5. Treatment Progress
The first option of treatment was chosen. The treatment started with an interceptive first phase, including an expander in the upper arch [16-18] and a lip bumper in the lower arch to gain some space. After one year of treatment, the cross-bite tendency was solved and the panoramic radiograph showed the recovery of the space for the upper cuspid eruptions (Fig. 4).
Then a challenging solution to solve geminated tooth shape, including the aesthetic expectations was performed with the stripping (Fig. 5). Moreover, the lower third molars were removed, before starting fixed appliances. After the first year of the interceptive phase, the maxillary expander was removed and the upper and lower arches were fully bonded. So, the second phase of treatment started with a fixed appliance and a trans-palatal arch.

At the end of the active treatment, the brackets were removed, and an upper Begg’s appliance and a lower canine-to-canine bonded retainer were used. The fixed phase lasted 20 months, the patient was motivated and cooperative throughout the entire treatment.
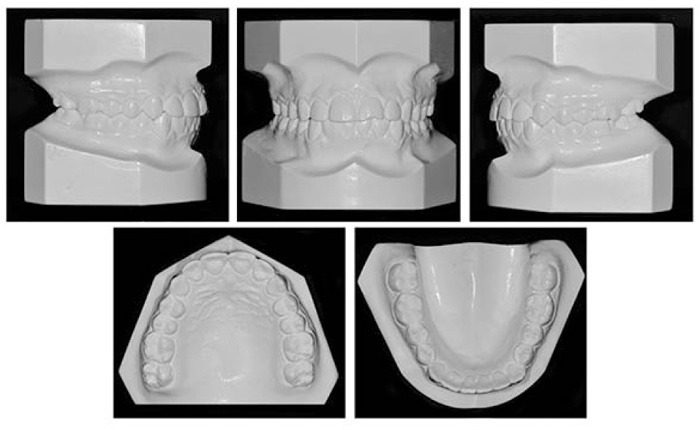
2.6. Treatment Results
The treatment objectives were achieved. The geminated tooth was left in its position showing good shape. The original color was preserved and the pulp vitality test continued to be positive. The occlusion showed a well-aligned dentition with a class 1 molar and cuspid relationship and a good tooth interdigitation, as demonstrated by the posttreatment casts. The crowding was completely solved in both arches, the bilateral cross-bite tendency and lower midline deviation were corrected, a normal overjet was achieved whereas the overbite was maintained (Figs. 6 and 7).
The posttreatment panoramic X-ray showed a proper root inclination of all teeth (Figs. 8A and 8B).

| Parameters | Initial | Final |
|---|---|---|
| SNA | 82° | 82° |
| SNB | 78° | 79 |
| ANB | 4° | 3 |
| Wits | -2 mm | -1 mm |
| SN-Go-Me | 32° | 32° |
| FMA | 21° | 21° |
| Se-N | 72 mm | 72 mm |
| PNS-A | 50 mm | 51 mm |
| Go-Pg | 78 mm | 80 mm |
| 1/SN | 101° | 103° |
| 1/Go-Me | 102° | 104° |
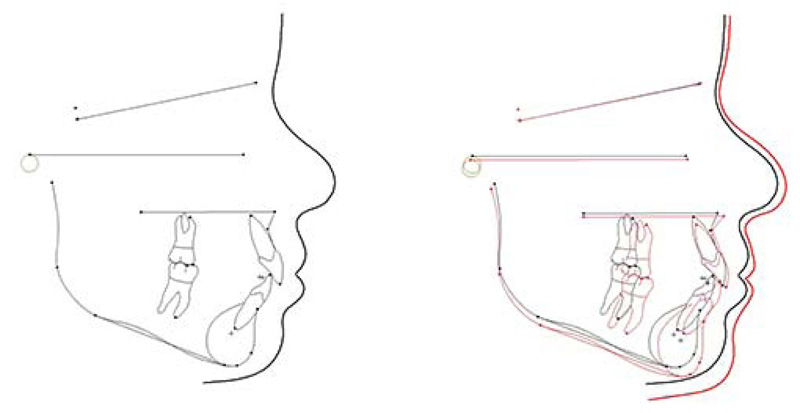
Superimposition revealed a good sagittal and vertical control (ANB = 3°, SN-GoMe = 32°) (Fig. 9); (Table 1). The treatment lasted 2 years and 6 months and the patient was motivated and cooperative throughout. An improved smile with a consonant smile arch was achieved, although the upper left central incisor still needed a restorative treatment. No signs or symptoms of temporomandibular joint disorder were present at the end of treatment. Oral hygiene was improved.
3. DISCUSSION
This case can be considered very rare for different reasons.
First of all, the prevalence of double-teeth in permanent dentition ranges from 0.1% to 0.2% [19], consequently, it is even more frequent to find this dental anomaly in primary dentition than in permanent. Moreover, in our case, the patient was a girl and, according to the literature, there is no sex predilection and gemination could be seen in both sexes with equal frequency [14, 19, 20]. As regards the position, our geminated tooth was observed in the mandible whereas they are commonly found in the maxilla, while cases of fusion are more habitually detected in the mandible as usually described [11, 14].
In addition, our tooth was a lateral incisor that rarely shows gemination. Conversely, gemination, generally, affected more maxillary central incisors as often reported [11, 19].
Furthermore, the case was particular also from an etiological point of view. The etiology of gemination is still unknown and unclear, although there are numerous hypotheses; Grover & Lorton claimed that local metabolic obstacles, which occurred during morpho-differentiation of the tooth germ, might be the cause, so they proposed that there could be a connection amongst gemination, twinning, and odontoma [8]. In particular, according to Shokri A. et al [19], the developmental irregularity of both the mesoderm and the ectoderm caused the gemination so it might be associated with the local metabolic interferences appearing during morpho-differentiation of the tooth germ.
In our case, the number of teeth was not reduced, as usually happens in cases of gemination, in fact, as reported by James EP et al, in the clinical situation, cases of fusion appear as congenitally missing tooth while in gemination, the number of teeth is normal, provided the double-tooth is considered as one unit [9].
The treatment of this dental anomaly is critical, especially in the anterior region, as in our case, because it can produce an unlikable aesthetic appearance due to uneven morphology [9-22].
Numerous treatment approaches have been designated with respect to different forms and morphological variations of geminated teeth, including endodontic restoration, periodontal therapy, orthodontic treatment, and surgical options with extraction and replacement of the tooth with an implant.
Though the agreement on the surgical approach is not always completed since, according to Braun et al, it implies not only the extraction of the whole tooth but also the remaining edentulous region after surgery that needs an expensive substitution with a prosthesis or an implant at the end of the growth.
In the meantime, the wearing of a partial denture can promote the loss of alveolar bone in the anterior maxilla [3]. Moreover, a long time is needed to preserve the space and implants are not necessarily a complication-free long-term solution, thus conservative treatment might be more appropriate [21-23]. However, the patient and her parents opted for coronoplasty with stripping followed by an orthodontic treatment because it was less invasive, simpler, shorter, and cheaper. The desired results were achieved. The aesthetic outcome of the crown shape was pleasing, even if the patient did not complete the restorative treatment of the broken upper left central incisor. The key points determining the resolution of this treatment option were a differential diagnosis and the patient’s motivation.
CONCLUSION
Differential diagnosis is one of the most difficult challenges for an orthodontist, due to similar
features between fusion and gemination. In dental practice, it is pretty rare to find these shape anomalies, but the dentist should be able to recognize immediately the nature of the problem and treat it appropriately. Early diagnosis and treatment are needed for a successful orthodontic solution as suggested by the aesthetic and functional outcome of this clinical case.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
The consent to process personal data and photographs was obtained by the patient and her parents.
STANDARD FOR REPORTING
Care guidelines and methodology were followed to conduct the study.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


