All published articles of this journal are available on ScienceDirect.
Sylc Air Polishing Versus Fluoride Varnish Application in Managing Dentin Hypersensitivity in Non-Carious Cervical Lesions: A Randomized Clinical Trial
Abstract
Objective:
To determine the effectiveness of Sylc (a bioactive glass-based powder) delivered by an air polishing system compared to fluoride varnish application in managing Dentin Hypersensitivity (DH).
Methods:
This study was a double-blinded randomized clinical trial where 50 participants with DH in at least one tooth with a non-carious cervical lesion were included and randomized into two groups (25 participants each) to receive either Sylc air polishing or fluoride varnish application. Baseline and post-intervention measurements of pain were carried out using evaporative, thermal and tactile stimuli using a modified visual analog scale at 3 minutes, 1, 2, 3and 4 weeks, 6 months and 1 year post-intervention. Data for pain intensity was recorded and analyzed for each group.
Results:
For the three stimuli used, Sylc air polishing showed statistically significant reduction of pain intensity (P<0.05) after 3 weeks and up to 1 year post-intervention. Fluoride varnish application showed a statistically significant reduction of pain intensity in evaporative and thermal stimuli at 1 week post-intervention only.
Conclusion:
Sylc air polishing was effective in relieving pain due to DH after 3 weeks and up to 1 year post-intervention, which showed that it can be used as a long-term treatment for DH.
1. INTRODUCTION
Dentin Hypersensitivity (DH) has been defined as brief, sharp, acute pain originating from exposed dentin in response to different stimuli such as thermal, tactile, osmotic, chemical or evaporative stimuli that cannot be attributed to any other dental pathology [1, 2]. The estimated prevalence of dentin hypersensitivity in various populations was observed to range from 1.3% up to 92.1% [3].
The hydrodynamic theory explained the cause of DH as stimuli acting on an exposed surface, causing movement of dentinal fluid, thereby activating nerve endings in the pulp. The stimuli are then conveyed to the central nervous system and felt as pain that lasts only for a short duration [4]. This painful sensation disturbs individuals during daily activities and negatively affects their quality of life. DH could result from certain behavioral factors as acid intake, leading to exposure of dentinal tubules. Other causes of DH could be dental caries, gingival recession, tooth wear, or tooth fractures [5].
Several approaches to DH treatment were proposed to interfere, whether transiently or permanently, with the hydrodynamic theory. These approaches include root coverage and the use of lasers, ions, dentinal sealants, and occluding and nerve depolarization agents, chosen according to the primary cause [6]. There are two major strategies in managing DH; the first is nerve desensitization, and the second is the physical occlusion of the patent tubule. The second approach can be carried out through a wide range of treatment modalities, including the use of proteins, salts or ions to plug the tubules, the use of restorative materials that physically block the patent tubules (dentin sealers) and the use of periodontal soft tissue grafts or lasers [7].
Many remineralizing agents introduced throughout the past years, capable of sealing dentinal tubules, can be used to reduce sensitivity [8]. Of these agents are over-the-counter fluoride-containing products. The Canadian Advisory Board recommended using a desensitizing fluoride toothpaste twice a day, which is considered a non-invasive first line of treatment [9, 10]. A review about at-home and in-office preventive treatment alternatives to reduce DH strongly recommended at-home treatments with fluoride toothpaste and suggested the in-office modalities for further trials. On the other hand, a long-term effect is expected through a material that binds to the dentin both physically and chemically, decreasing the chance of reopening of the dentinal tubules [11].
Novamin, an inorganic, amorphous melt-derived glass compound containing calcium, sodium, phosphate and silica, was introduced into the market in 2003. A bioactive glass with desensitizing capability, Novamin offers immediate and long-lasting pain relief. It is also capable of remineralizing enamel and has antimicrobial and anti-inflammatory properties, making it a promising candidate for the treatment of gingivitis [12]. A new form of the bioactive glass is the airflow-based prophylactic powder (Sylc), the active ingredient of which is also NovaMin. In the salivary environment, the Sylc (NovaMin) releases calcium and phosphate ions. Airflow-applied Sylc forms the biologically stable, acid-resistant Hydroxycarbonate Apatite (HCA), which is very strong and resilient. The continuous release of calcium ions promotes constant protection and long-lasting seal of the tubules [13, 14].
Although there are many therapeutic agents in the market for DH management, there is still no specific treatment that rapidly treats and permanently eradicates DH [15]. More controlled studies are required to differentiate among different desensitizing agents, with the introduction of new methods that might be more beneficial and effective, less time consuming and more convenient than those commonly used. Therefore, the aim of this study was to investigate the effectiveness of air polishing using bioactive glass-based Sylc powder compared to fluoride varnish application in the management of DH in non-carious cervical lesions.
2. MATERIALS AND METHODS
2.1. Trial Design and Settings
This study was a single-centered, randomized, parallel-arm clinical trial with an equal allocation ratio. The study was reported according to the Consolidated Standards of Reporting Trials (CONSORT) statement and carried out in agreement with the Declaration of Helsinki principles. The study was conducted and approved by the research ethics committee at the Faculty of Dentistry, Cairo University (#17917). The study was registered at ClinicalTrials.gov (NCT03285360).
2.2. Participants Eligibility Criteria
Participants were recruited from the Conservative Dentistry Department Clinic at the Faculty of Dentistry, Cairo University. Participants of both genders aged 18 to 70 years with good oral hygiene, suffering from pain due to DH in at least one tooth with a non-carious cervical lesion and scoring higher than 5 on the Visual Analog Scale (VAS) in response to evaporative stimulus (using air-water syringe for 1-5 seconds), were included in this study. Pregnant women, people with teeth exhibiting mobility (grade 2 or 3) or having deep periodontal pockets (>4 mm), people with orthodontic appliances, and people with allergy to any of the materials used in the study were excluded.
2.3. Interventions
Interventions used in the study were either Sylc® original SR (DENFOTEX Research Ltd., UK) calcium sodium phosopho-silicate based bioactive glass powder to be used in an air-powered tooth polishing system (NSK- ProphyMate neo.) or BiFlourid 10 (Voco, Germany) fluoride-based varnish. Intervention steps were carried out by a single operator.
For the first group; after isolation and cleaning of the tooth surface, the Prophymate Neo handpiece was held at an estimated distance of 3-4 mm from the tooth surface. The nozzle was positioned just above yet not in direct contact with the tooth surface by which the particles came out of the nozzle freely and precipitated on the surface. Free circular movement was used to deliver the Sylc powder particles on the sensitive area(s) for 5-10 seconds while a high-volume suction was directed toward the tooth from the other side.
For the second group; after isolation and cleaning of the tooth surface, a thin coat of BiFlourid 10 varnish was applied using a micro-brush on the sensitive area(s) and left for 10-20 seconds then air-dried. All participants were instructed, after application of the interventions, to avoid eating or drinking for one hour, to avoid brushing or flossing for 4-6 hours and to avoid using any toothpaste containing fluoride until the end of the follow-up period. Measurements were recorded after application of the intervention by 3 minutes, and participants were phoned at 1, 2, 3 and 4 weeks, 6 months and 1 year post-intervention to come to the follow-up visits and record their pain level on the VAS.
2.4. Outcomes
Pain due to hypersensitivity was determined using evaporative, thermal (cold) and tactile stimuli tests. Participants recorded their pain levels after each test on a modified 10 cm VAS with numerical categories expressing severity of pain (0 = No Pain, 1-3 = Mild Pain, 4-6 = Moderate Pain, and 7-10 = Severe Pain) and color-coded facial expressions to facilitate pain expression. Between every 2 tests, there was a rest period of 5 minutes to allow tooth recovery. Measurements were recorded after application of the intervention by 3 minutes, 1, 2, 3 and 4 weeks, 6 months and 1 year. The evaporative test was carried out using an air blast from a conventional dental unit air-water syringe for 5 seconds. The thermal test was carried out using Endo-Frost (Roeko, Germany) refrigerant spray on cotton applied on the tooth surface for a maximum of 5 seconds [16]. The tactile test was carried out using the tip of a sharp explorer (number 3) to gently scratch the exposed cervical surface in an apico-coronal direction with short strokes. All stimuli tests were stopped immediately as soon as the participants reported pain.
2.5. Sample Size Calculation
Sample size calculation was achieved using PS: Power and Sample size calculation software version 3.1.2 (Vanderbilt University, Nashville, Tennessee, USA) based on a previous paper [17]. The expected difference in the VAS score was 7±5. 17 subjects were needed in each group, as calculated using a power of 80% and 5% significance level. The number was raised to 20 in each group to compensate for possible follow-up losses and raised again to 25 to correct for non-parametric distribution.
2.6. Allocation Sequence Generation and Concealment
Fifty eligible participants were randomly assigned to one of the interventions using a computer-generated random numbers list (random.org) with 1:1 allocation ratio. Allocation sequence concealment was achieved by using opaque sealed sequentially numbered envelops. After signing the informed consent, each participant chose an envelope, which was signed by both the participant and the supervisor to ensure the irreversible assignment of each intervention. Blinding of the participants was ensured by using the same air-powered polishing system in the fluoride varnish group but with no powder. Outcome assessors were blinded to the type of intervention received by the participants (double-blinding). To increase the chances of the participants following through with the trial, their personal data and contact information as well as the contact information of two reachable relatives or friends were thoroughly recorded. Additionally, as a reward, the participants got treatment for their other dental needs between the visits. Also, those who took a day off from work or came from rural areas to attend the follow-up visits were financially reimbursed.
2.7. Statistical Methods
Data were statistically described in terms of mean and standard deviation (SD) or median and range when appropriate. Comparison between the study groups was done using Mann Whitney U test for independent samples whereas comparison within the same group was done using Wilcoxon signed rank test for paired (matched) samples. Two-sided p values less than 0.05 were considered statistically significant. All statistical calculations were done using SPSS® (Statistical Package for the Social Science; IBM® Corp, Armonk, NY, USA) for Microsoft Windows.
3. RESULTS
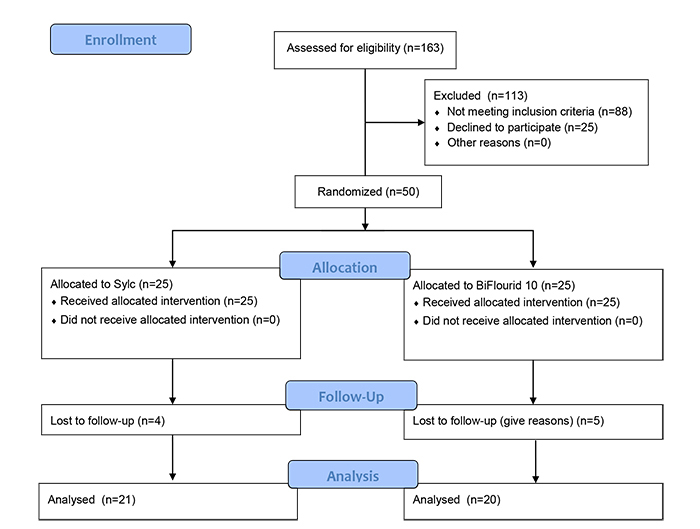
Fifty participants were randomized into two groups of 25 each. A total of nine participants were lost to follow-up, 4 in the Sylc group and 5 in the BiFlourid 10 group. Participants’ flow through the trial is presented in a CONSORT flow diagram (Fig. 1).The age range of the participants in the Sylc group was 18-52 years and in the BiFlourid 10 group was 21-62 years.
3.1. Evaporative Test
Median and range values of pain intensity for different interventions and follow-up intervals are presented in Table 1. Regarding the baseline records of pain, there was no statistically significant difference between the two groups (P=0.125). There was a significant decrease in pain intensity in each group during successive follow-up intervals (P<0.001) (Table 1).
3.2. Thermal Test
Median and range values of pain intensity for different interventions and follow-up intervals are presented in Table 2. Regarding the baseline records of pain, there was no statistically significant difference between the two groups (P=0.432). There was a significant decrease in pain intensity in each group during successive follow-up intervals (P<0.001) (Table 2).
| Follow-up Intervals | Intervention [Median(Range)] | P-value | |
|---|---|---|---|
| Sylc powder | BiFlourid 10 | ||
| Baseline | 8.00 (4.00) | 9.00 (3.00) | 0.125ns |
| 3 minutes | 7.00 (4.00) | 7.00 (3.00) | 0.295ns |
| 1 week | 6.00 (4.00) | 5.00 (7.00) | 0.005* |
| 2 weeks | 3.50 (6.00) | 3.00 (7.00) | 0.512ns |
| 3 weeks | 1.50 (4.00) | 4.00 (8.00) | <0.001* |
| 4 weeks | 0 (5.00) | 4.00 (8.00) | <0.001* |
| 6 months | 0 (5.00) | 3.00 (7.00) | <0.001* |
| 12 months | 0 (3.00) | 3.00 (10.00) | <0.001* |
| Follow-up Intervals | Intervention [Median (Range)] |
P-value | |
|---|---|---|---|
| Sylc powder |
BiFlourid 10 |
||
| Baseline | 8.00 (4.00) | 8.00 (4.00) | 0.432ns |
| 3 minutes | 7.00 (5.00) | 7.00 (4.00) | 0.856ns |
| 1 week | 6.00 (5.00) | 4.00 (7.00) | 0.009* |
| 2 weeks | 3.00 (6.00) | 3.00 (7.00) | 0.539ns |
| 3 weeks | 1.00 (5.00) | 4.00 (7.00) | <0.001* |
| 4 weeks | 0 (6.00) | 4.00 (9.00) | <0.001* |
| 6 months | 0 (5.00) | 4.00 (9.00) | <0.001* |
| 12 months | 0 (3.00) | 3.00 (10.00) | <0.001* |
3.2. Tactile Test
Median and range values of pain intensity for different interventions and follow-up intervals are presented in Table 3. Regarding the baseline records of pain, there was no statistically significant difference between the two groups (P=0.847). There was a significant decrease in pain intensity in each group during successive follow-up intervals (P<0.001) (Table 3).
| Follow-up Intervals | Intervention [Median(Range)] | P-value | |
|---|---|---|---|
| Sylc powder | BiFlourid 10 | ||
| Baseline | 7.00 (3.00) | 7.00 (3.00) | 0.847ns |
| 3 minutes | 6.00 (6.00) | 6.00 (4.00) | 0.339ns |
| 1 week | 4.00 (5.00) | 4.00 (8.00) | 0.226ns |
| 2 weeks | 2.00 (4.00) | 2.00 (6.00) | 0.266ns |
| 3 weeks | 0 (4.00) | 4.00 (6.00) | <0.001* |
| 4 weeks | 0 (5.00) | 3.00 (9.00) | <0.001* |
| 6 months | 0 (3.00) | 3.00 (8.00) | <0.001* |
| 12 months | 0 (2.00) | 2.00 (8.00) | <0.001* |
4. DISCUSSION
The most successful treatment of DH is to mimic the natural process of occluding open dentinal tubules. Naturally, saliva plays a role in providing calcium and phosphorus ions that aid in gradual occlusion, forming a superficial layer of calcium, phosphates and salivary glycoprotein aggregates [18]. However, the natural pathway does not cause rapid occlusion and elimination of pain; therefore, extra amount of calcium and phosphates must be available in the oral environment in order to speed up the process. Different compositions containing amorphous calcium phosphate and biomaterials as calcium phosphosilicate mixtures present in the bioactive glass particles are used to help in the rapid occlusion of dentinal tubules [19]. Sylc is a bioactive glass material that reacts with saliva to deposit HCA, which is chemically similar to natural tooth minerals [20]. Sylc bioactive glass showed remarkable occlusion of the dentinal tubules when used in air polishing procedures and when applied with rubber cups as prophy-paste [21]. Air polishing using Sylc powder provides a bifunctional advantage of polishing the tooth surface and occluding the dentinal tubules.
In this clinical trial, all steps were performed according to the guidelines for the design and conduct of clinical trials on DH [22]. DH was assessed by three different stimuli (evaporative, thermal and tactile) to simulate the different situations in which DH arises. Though the Numerical Rating Scale (NRS) and Verbal Rating Scale (VRS) are generally used for pain assessment, they are limited in scope and less recommended in the assessment of DH. In this study, the Visual Analog Scale (VAS) was used as it is counseled by the guidelines of conducting clinical trials on DH [22]. Using the VAS, the participant marks the pain intensity on a graduated 10 cm straight line (0 = no pain, 10 = extreme pain). In the current study, an illustration of facial expressions with color codes was added below the 10 cm line Visual Analog Scale in an attempt to make the scale easily understood by participants who might have a low level of education. In fact, the addition of the facial expressions resulted in more participant cooperation than that resulting from using a plain 10 cm line alone [23]. Trial assessment periods were sufficient to allow the expression of maximum efficacy of the intervention used. In this clinical trial, the assessment intervals were at the baseline and 3 minutes, 1, 2, 3 and 4 weeks, 6 months and 1 year post-intervention.With long-term follow-up periods (1 year), it was a challenge to make the participants show up to all their follow-up visits. Therefore, measures to improve their compliance were applied.
The pain responses differed according to the type of stimulus used. The tactile stimulus evoked the least pain response in comparison to the other two stimuli. The evaporative and thermal stimuli elicited nearly the same responses at all assessment periods, as the space between the odontoblastic process and the tubule wall (the peri-odontoblastic space) is thought to be occupied by dentinal fluid [24]. When dentin is exposed to external stimuli, a fluid shift occurs across the dentinal tubules to create a neurovascular response (pain sensation). The tactile stimulation showed the least pain response as it has the least influence on the movement of the peri-odontoblastic fluid. The evaporative and the thermal stimuli elicited more pain as they directly stimulate the fluid movements [25-29].
At the baseline and after 3 minutes, both interventions showed similar results, possibly attributed to insufficient time for both interventions to work. After 1 week, the fluoride varnish application showed a more statistically significant reduction of pain intensity than did the air polishing with Sylc powder. A possible explanation is that most of the fluoride particles were incorporated into the tooth within the first two weeks through the regular action of the fluoride varnish. The solvents of the varnish evaporate when applied, leaving a thin layer of material covering the exposed dentinal tubules. This effect might partially decrease dentin permeability, diminishing the hypersensitivity.
After two weeks, both interventions had the same effect on pain intensity with no statistically significant difference. This result could be attributed to continuous dentinal tubules occlusion either by CaF from fluoride varnish or by bioactive glass from Sylc powder. After 3 weeks and up to 1 year post-intervention, Sylc powder showed a more statistically significant reduction in pain intensity than did the fluoride varnish application. This result could be due to the effect of bioactive glass powder, which obliterates most of the dentinal tubules mechanically and chemically. Another reason could be the failure of maintenance of occlusion of the dentinal tubules by the formed CaF and fluorapatite compounds due to abrasion caused by tooth brushing or acidic challenges by erosive drinks throughout the follow-up periods. Regardless of the exact cause, topical fluoride applications are considered of enormous value in managing DH but not a long-lasting treatment. On the other hand, the Sylc powder air polishing application showed significantly lower median values at all follow-up periods, indicating successful management of DH. Sylc powder application by air polishing showed higher pain intensities than did fluoride varnish in the 1st week. These resultant values may be due to the slow chemical action of the bioactive glass, causing only partial dentinal tubules obliteration without completely treating DH. Surprisingly, after 3 and 4 weeks, 6 months and 1 year, the median values of Sylc powder were zero, indicating a complete and long-lasting treatment of DH. The dentinal tubule occluding effect of bioactive glass has been attributed to the formation of an HCA layer on the surfaces besides their mechanical occlusion of dentinal tubules.
Using the air polishing delivery system provided a huge number of calcium and phosphate particles presented in the Sylc at the exposed surface of the tooth. Moreover, the air pressure aided in pushing these particles inside the dentinal tubules to a considerable depth. The small size of the Sylc particles helped in infiltrating into the dentinal tubules to a depth of about 100 nm, leading to better effectiveness and durability. Furthermore, the elevation of local pH arising from the application of bioactive glass could also provide the essential alkaline environment that facilitates the precipitation of calcium and phosphate from the particles and from saliva to form a calcium phosphate (Ca-P) layer on tooth surfaces. As the reactions and the deposition of Ca-P complexes continue, this layer crystallizes into HCA, which is chemically and structurally similar to biological apatite [30-33]. The combination of the residual calcium sodium phosphosilicate particles and the HCA layer results in the physical occlusion of dentinal tubules with a longer-lasting effect. Furthermore, the chemical reactions initiated by calcium sodium phosphosilicate particles to promote the formation of an HCA layer for the treatment of DH may also be useful in treating demineralized tooth structure and/or preventing further demineralization [34].
Within the conditions of this study, participant compliance, regarding the 1-year follow-up period, was challenging and was overcome by explaining the problem of DH to the participant. DH is relieved by the formation of reparative dentin and by the proper treatment of the etiology, possibly decreasing the painful sensation, leading to discontinuation of the participant from the trial. This difficulty in achieving good participant compliance was overcome by explaining to the participants the problem associated with DH, the etiological factors, and the importance of changing the overall lifestyle according to the etiological factor diagnosed.
CONCLUSION
Sylc application using air polishing showed a significant reduction in pain caused by DH compared to fluoride varnish application in all test stimuli after 3 weeks and up to 1 year post-intervention. This could indicate the use of Sylc air polishing as a long-term treatment for DH in non-carious cervical lesions. Remineralizing glass powder administration through air polishing was preferred by the participants, as it has more than one resultant benefit with the same application. It manages to diminish the hypersensitivity while leaving the tooth surface clean and shiny. Conduction of further randomized clinical trials is suggested to investigate the effectiveness of Sylc air polishing on DH and to obtain recommendations and consensus for population and clinicians.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the research ethics committee at the Faculty of Dentistry, Cairo University , Egypt with approval No.(#17917), and the study protocol was registered at Clinical Trials.gov (NCT03285360).
HUMAN AND ANIMAL RIGHTS
No animals were used in this study. The study was carried out in agreement with the Declaration of Helsinki principles.
CONSENT FOR PUBLICATION
Written informed consents were signed by all participants before starting the study.
AVAILABILITY OF DATA AND MATERIALS
The data sets analyzed during the current study are available from the corresponding author [D.M] upon request.
FUNDING
None.
CONFLICT OF INTERESTS
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


