All published articles of this journal are available on ScienceDirect.
Dentists and Dental Intern’s Preferences of Root Canal Treatment with Restoration Versus Extraction then Implant-Supported Crown Treatment Plan
Abstract
Objectives:
The intent of this study was to evaluate and compare the preferences and treatment choices between dentists and dental interns with regard to the following different treatment modalities: Root Canal Treatment (RCT) with restoration versus extraction with Implant-Supported Crown (ISC) or surgical treatment in relation to the given case scenarios.
Methods:
The questionnaire was presented as an online survey with a case scenario. The total number of the respondents were 165. The four clinical case scenarios included an anterior and posterior tooth having apical periodontitis, with and without previous RCT. The treatment options were as follows: RCT with restoration, extraction then implant, and surgical treatment.
Results:
A total of 165 dentists and dental interns were included in this study. A hundred and three 62.4% respondents were dentists, 60; 36.3% were males and 105; 63.7% were females. Most of the respondents graduated from the College of Dentistry, Jazan University (93.9%). The highest percentages and numbers for Anterior Teeth (AT) were selected in related to the RCT and restorations in the four scenarios among gender, dentists, and interns, with no considerable differences. A high percentage of RCT and restoration option was recorded for Posterior Teeth (PT) with no previous restoration and around 50% for the same treatment modality to posterior teeth with previous restorations. For Future Planning Postgraduate Studies (FPPS), it was obvious that most of the selected specialties agreed with the RCT and restorations choice.
Conclusion:
All dentists and interns in both genders preferred RCT with restorations over extraction, and then ISC in the AT with and without previous RCTs. In the PT with no previous RCT, the participants agreed that RCT with restorations is superior to other choices. Among the FPPS, the respondents demonstrated an absolute agreement to RCT and restorations as a treatment of choice for different scenarios.
Clinical Significance:
Dentists should preserve the natural teeth by RCT with restoration as the first treatment choice followed by other choices. The nonsurgical approach should always be adopted as a routine measure in PA lesions of endodontic origin. Conservative orthograde endodontic therapy demonstrates favorable outcomes with a regular periodic review and assessment of the healing process of PA lesions.
1. INTRODUCTION
Teeth without periapical lesions prior to Root Canal Treatment (RCT) have higher success rates than those with lesions [1]. Usually, RCT with final restoration is less costly than an Implant Supported Crown (ISC) prosthesis [2]. Considering the number of procedures that accompany either mentioned treatments can be a determining factor in what a patient can afford and therefore becomes part of the decision as to which treatment is provided [1-3]. Fixed Partial Dentures (FPD) is an option once a tooth is extracted and it has lower survival rates than single RCT plus restoration or ISCs, which have high survival rates [3, 4].
Many factors, such as cost, number of adjunctive procedures, esthetic and biologic considerations, compromised ability to restore a tooth, anatomic factors, tooth color and tooth thickness, patient preference, and other systemic factors, affect the choice of treatment [2-4]. RCT is an appropriate and cost-effective intervention to extend the life of a tooth with a diseased pulp. The RCT procedures always involves cavity preparation followed by disinfection of endodontic space [5], as well as a proper root canal filling technique [6]. Orthograde re-treatment is also cost-effective; however, unless clinically indicated, the benefits of additional apical surgery do not justify the additional cost [4, 7]. Based on an American Dental Association survey in the United States, initial (not lifetime) costs were compared for a simple extraction, extraction then an Implant Supported Crown (ISC), and extraction followed by a three-unit Fixed Partial Dentures (FPD) with a high noble FPD restoration. They concluded that a slight difference in the cost but a time factor is different [2, 8].
The ISC studies frequently reported outcome rates exceeding 95%. Meta-analyses found success rates of 96.7% to 97.5% for single-unit restorations and 92.5% to 93.6% for FPD restorations over six to seven years [8, 9]. Others shows that both ISC and RCT have superior long-term survival compared with FPD [10-12].
Dentists are regularly confronted with difficult choices. Should a tooth that has not healed through nonsurgical RCT through endodontic microsurgery be replaced using an ISC [13]. Modern dentistry should follow an evidence-based approach; however, the question of retention or extraction of a tooth has not been satisfactorily answered at a high level of evidence [14]. Investigating the decision-making process between tooth retention and extraction is difficult. A tooth may be functioning; however, multi-factorial risks may lead to extraction upon endodontic or restorative treatment attempts [15, 16]. This phenomenon is complicated by countless natural or pathological variations, different treatment planning options, clinician’s background and/or skillfulness, and patient preferences [17].
Some researcher’s concluded that the majority of dentists preferred RCT with restoration than extraction, then ISC for teeth with apical periodontitis [16, 18]. Patients, as well as dentists, preferred preserving their teeth by RCT with restorations than other choices even in the presence of Periapical Pathosis (AP) [19, 20].
Three local studies were conducted in Saudi Arabia. The first one assessed the importance of preserving natural teeth with RCT versus ISC and concluded that the majority of cases needed referral system because treated cases were performed with less experienced general practitioner dentist [21]. The others suggest that their respondents preferred RCT with proper restoration represented a practical and economical choice over extraction, followed by ISC in both AT as well as PT [22, 23]. Hence, the main purpose of the current study was to evaluate the dentist and the dental intern preferences and treatment choices with regard to the following different treatment options: Root Canal Treatment (RCT) and restoration versus extraction, then Implant-Supported Crown (ISC) or surgical treatment. Comparisions were done between gender, dentists, dental interns and their Future Planning Postgraduate Studies (FPPSs) in relation to the different treatment scenarios.
2. MATERIALS AND METHODS
2.1. Study Design and Sampling
This current study used a cross-sectional study design to evaluate the preferences among dentists (graduated students with minimum of 3 year’s experiences), dental interns (graduated students in a one year internship program), and the Future Planning Postgraduate Studies (FPPS) (group of general practitioners, those willing to go for postgraduate studies in different dental specialties), from different university, and College of Dentistry. This study was based on a four-point questionnaire.
2.2. Questionnaire
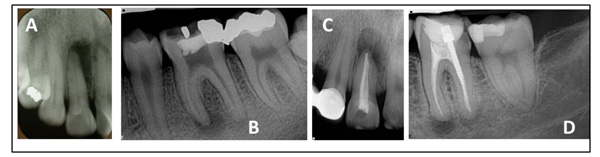
A self-administrated survey was utilized and distributed among the target population. The questions on the clinical domain comprised of four case scenarios as mentioned by Wenteler et al., Azarpazhooh et al., Azarpazhooh et al., and Mashyakhy MH [7, 18, 20, 22], with some modifications. The case scenario included AT and PT with apical periodontitis with and without previous RCT. Along with the description, a radiographic image was provided with each clinical scenario (Fig. 1). Participants were asked to choose the best treatment plan for each clinical scenario based on their knowledge and understanding. The questionnaire was presented as an online survey with the following case scenarios.
2.3. Case Scenarios
A 50-years-old male patient presented with a permanent tooth with apical periodontitis. The medical history was noncontributory, and the periapical X-ray showed apical radiolucency associated with the tooth. The tooth is restorable, and the overall prognosis (periodontics, endodontics, restorative, and prosthodontics) is favorable. Presented below are the four clinical scenarios with radiographs for anterior and posterior teeth with and without previous RCT (Fig. 1). Please select the treatment plan for each scenario. The four clinical scenarios were as follows:
- An anterior tooth with no previous RCT and presence of PA periodontitis.
- A posterior tooth with no previous RCT and presence of PA periodontitis.
- An anterior tooth with previous RCT and presence of PA periodontitis.
- A posterior tooth with previous RCT and presence of PA periodontitis.
The treatment options were as follows: RCT with restoration, extraction then ISC, and surgical treatment.
2.4. Data Collection and Analysis
This cross-sectional study was conducted in full accordance with the World Medical Association Declaration of Helsinki. The Ethics Committee of the Director of Health Affairs in the related region approved the study proposal. Data from the online-based questionnaire were pooled for analysis. IBM Statistical Package for the Social Sciences V 20.1 (SPSS IBM, Inc., Chicago, Illinois, USA) was used for statistical analysis. Descriptive analysis was conducted for all the scenarios. In addition, responses of respondents for each gender group, category (dentist or intern), and FPPSs were compared by respondent Chi-Square test and Fisher’s Exact test. Statistical significance was set to a p-value of ˃ 0.05.
3. RESULTS
Out of the 200 questionnaires distributed, only 165 dentists and interns answered the questionnaires during the study period. The survey response rate was 82.5%, the others did not answered the questionnaires because of the lack of time or refusal to participated in the study. Table 1 summarizes the demographic data of the subjects, of which 103; 62.4% respondents were dentists and 62; 37.6% were interns, males were 60; 36.3% and 105; 63.7% were females. The mean age was 24.18 years, and the standard deviation was 0.817. The frequency and percentage of the graduate dentists from the College of Dentistry of Jazan University were 155; 93.9%. Four groups were recorded according to the year of graduations; 2012-year; 0.6%, 2013-year; 50.3%, 2014-year; 46.7%, and 2015-year; 2.4%. A total of 10 subgroups of FPPSs were recorded, the highest percentages subjects had selected Endodontists (ENDO) with 22.4%, followed by Orthodontics (ORTHO), Prosthodontics (PROS), and Oral and Maxillofacial Surgery (OMS) 13.9%, 12.7%, and 11.5%, respectively. A total of 12.1% decided to stay as General Practitioners (GP) dentists (Table 1).
Regarding the choices of the categories in the different clinical and radiographical scenarios, Graph 1 shows that the percentages in the RCT with restoration choices were 83.5% and between 14.5-16.5% in the extraction then ISC in the AT with no previous RCT. Only 4.8% among interns were registered in the surgical treatment choice. For the PT with no previous RCT, over 95% were registered in terms of RCT with restoration. However, it was only 1.9% among dentists in the surgical treatment choice. In the AT with previous RCT, between 66%-77.4% in RCT with restoration options were selected by the categories, while it was between 16.1%-17.5% and 6.5%-16.5% in the extraction then ISC and surgical treatment choices for interns and dentists, respectively. In the PT with previous RCT, the percentages were close to each other and in the middle and ranged from 40.8%-48.4% & 21.0%-35.9%, and 30.6-23.3% for RCT with restoration, extraction then ISC, and the surgical treatment choices, respectively (Graph 1). No significant differences were detected among categories with P-values more than 0.05 for the different clinical scenarios.
| Parameter | Number | % | |
|---|---|---|---|
| Category | Dentists | 103 | 62.4 |
| Interns | 62 | 37.6 | |
| Gender | Male | 60 | 36.3 |
| Female | 105 | 63.7 | |
| University | Jazan | 155 | 93.9 |
| Others | 10 | 6.1 | |
| Year of graduation | 2012 | 1 | .6 |
| 2013 | 83 | 50.3 | |
| 2014 | 77 | 46.7 | |
| 2015 | 4 | 2.4 | |
| Future Planning Postgraduate Studies (FPPS) |
Endodontic | 37 | 22.4 |
| Restorative | 8 | 4.8 | |
| Orthodontics | 23 | 13.9 | |
| Prosthodontics | 21 | 12.7 | |
| Oral & maxillofacial surgery | 19 | 11.5 | |
| Public health | 11 | 6.7 | |
| Periodontics | 12 | 7.3 | |
| Periodontics | 13 | 7.9 | |
| Oral medicine | 1 | .6 | |
| No specialty | 20 | 12.1 | |

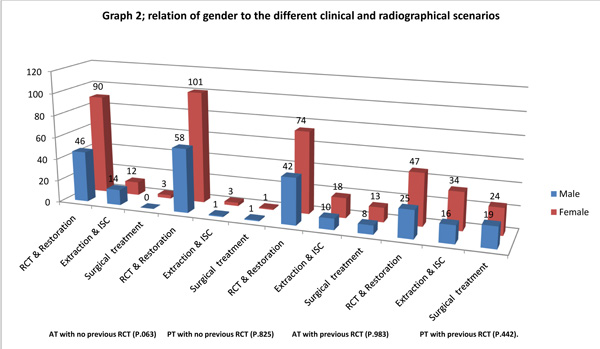
The relationship between gender and the four clinical and radiographical scenarios are presented in Graph 2. In the AT with no previous RCT, the percentages were similar in both genders in terms of RCT with restoration and extraction then ISC, which were 76.7% & 23.2% for males; and 85.7% & 11.4% for females, respectively, while it was relatively low in the surgery treatment choice. In the PT with no previous RCT, a high percentage was registered in terms of RCT with restoration of 96% and extremely low percentages were recorded for extraction then ISC, (1%-2.9%) in both genders. In the AT with previous RCT, 70% selected the treatment by RCT with restoration and approximately 17% in extraction then ISC, while it was only around 13% in the surgical treatment choice for both genders. Finally, 41.7% & 26.7% for males and 44.8% & 32.4% for females were recorded for the choices of RCT with restoration and extraction then ISC, respectively, and between (22.9%-31.7%) for the females and males in the surgical treatment choice in the PT with previous RCT (Graph 2). No significant correlations were observed among all factors and P-values were .063, .825, .983, .442, for the different clinical scenarios, respectively.
Graph 3 represents the respondent’s choices regarding FPPSs selected and the different clinical and radiographical scenarios in the presences of PA periodontitis. In the AT with no previous RCT, the percentages were high in ENDOs (94.6%), followed by OMS (84.2%), then Periodontics (PERIO) 76.9%, and PROSs 76.2, but it was low in the Restorative (RESTO) specialty (12.5%) for the treatment choice of RCT with restoration, but it was 5.4%, 15.8%, 11.5, 23.8% for extraction then ISC in the same selected specialties. In the PT with no previous RCT, a high percentage reaching 100% has been registered in all selected specialties except in restorative (75%) and GPs (80%) subgroups, in the restorative for the RCT with restoration treatment modality. The results were extremely very low and registered (0.00%) mostly in all specialties; except for 4 cases, 20% for the GPs and 2 cases of 25% in the RESTO subgroups selected for extraction, then ISC and surgical treatment choices. In the AT with previous RCT, the percentages were high being 84.6%, 81.8%, 78.3%, and 70.3% in PERIO, public health (PH), ORTHO and ENDO subgroup, respectively, in terms of the treatment choice of RCT with restoration, while the percentages were in middle among other specialties. But it was ranged from 8.3% to 36.8% in peidodontics (PEIDO) and OMSs in extraction then ISC in the same specialty, respectively. In the PT with previous RCT, 69.6% was registered in ORTHO, 61.5% in PERIO, 59.5% in ENDO, and 50% in the RESTO, but it was 9.5% in PROS subgroup for the RCT with restoration treatment. The percentages were in different ranges for the same specialty in extraction, followed by ISC and surgical treatment choices. The results were significantly different with p-value less than 0.05 in the different treatments choices, but it was not significant in the treatment of AT with no previous treatment in which the P-value was 0.097.
4. DISCUSSION
In the current cross-sectional study, the questionnaire was designed to determine the dentists and dental interns preferable for three different treatment modalities: RCT and restoration, extraction then ISC prosthesis, and surgical treatment in AT and PT with and without apical periodontitis. The radiographic interpretations were constantly subjected to inter- and intra-observer variations [24]. One of the most difficult aspects of any healthcare profession is decision making. The education of a dentist can play an important role in decision making and may also result in different treatment choices [16, 25].
From Graph 1, the dentists and dental interns preferred RCT with restoration over extraction then ISC prosthesis for AT with or without previous restorations. The percentages of the treatment modality (RCT with restoration) in the AT with no previous RCT were relatively high and ranged from 70%-83%, while that for AT with previous RCT and restoration reached 66%-70%. This is in agree with Azarpazhooh et al., Azarpazhooh et al., Azarpazhooh et al., and Mashyakhy MH [16, 18, 19, 22]. The other treatment choice extraction then ISC was only around 15%-17%, while the surgical treatments were the least selected scenarios in the same treatment choices. These results were contrary to a similar survey conducted by Azarpazhooh et al., Aldawsari and Alamir, and Mashyakhy MH [20-22]. Many previous systemic reviews concluded that no differences exist in the survival outcome of the two treatment modalities [8], which they prefer to maintain the natural teeth with RCT with restoration before extraction followed by ISC treatment [3, 14, 23, 26].

Dentists and dental interns absolutely agreed that the RCT with restoration was the treatment choice for the PT with no previous RCT, and reaching over 95% in both treatment modalities. This finding is in contrast with the finding of Mashyakhy MH [22] who recorded a percentage lesser than 50% in their survey. This can be explained by the level of education for the selected subjects (fourth-year students); by contrast, our respondents were graduates/or with a few years of experience. Long-term survival of posterior RCT with restoration was superior to FPD and ISC [4]. The contrast was found in the percentage with the scenario of the PT with the previous RCT, which did not reach 50% among dentists compared with 40.8% of dental interns (Graph 1). This finding can be explained by the apprehension of the respondents regarding the healing of the periapical lesion and the additional appointments needed [21, 26]. The treatment option of extraction and ISC reached between 21%-35.9% in the PT with previous RCT scenarios in terms of categories (dentist or dental intern). This result is well supported bystudies [8, 10, 13-15], those concluded that ISC had a higher survival rate at four to six years than teeth treated with endodontic microsurgery. Qualitatively different success criteria precluded the valid comparison of success rates. Some systematic reviews have also mentioned that the survival rates of ISC and RCT with restoration are similar [17, 27].
In relation to the percentages for the male and female recorded, the findings were in complete agreement with the results obtained by Mashyakhy MH [22]. Despite this variability, radiographs are known to play a crucial role in decision making regarding various dental treatments. The respondents had three available treatment options for the four case scenarios presented, and a general consensus was obtained among the participants (Graph 2).
A nonsurgical approach should always be adopted as a routine measure in PA lesions or periodontitis origin.Conservative orthograde RCT demonstrates outcomes. Regular periodic review and assessment of the healing process of periapical lesions are essential. The progression of this lesion results in local inflammation, resorption of hard tissues, and destruction of other periapical tissues [28]. In the current study, the AT or PT with or with no previous RCT with apical periodontitis, the results from Graphs 1 and 2, dentists, interns and both gender were nearly significant with P-values .077 and .063, respectively, which means that most of the respondents preferred RCT for a single or multiple rooted teeth even in the presence of PA periodontitis. This was obvious in other findings [18, 19, 26]. A number of studies have reported a success rate of up to 85 percent after non-surgical RCT of teeth with periapical lesions [28-30].
In the current study, in relation to the FPPSs, the respondents who selected ENDO, PROS, and PERIO totally agreed that RCT with restoration is the choice of treatment for the AT teeth with no previous RCT scenario, and their percentages were 94.6%, 76.2%, and 76.9%, respectively. This coincided with the previous results mentioned by Baba et al., Torabinejad et al. [3, 8], and Azarpazhooh et al., 2013a [19], who's recorded that most of their GPs, PROS, PERIO, OMS had selected the ISC over the RCT and restorations, when compared to ENDOs group. This does not coincided with our findings which may explained by their dentists' preferences associated with their professional registration. Also, we are not in agree with the results concluded by Wenteler et al. [7], those examined GPs and specialists variously RCT strategies according to the type of coronal restoration and their treatment choices were preferred extraction and replacement with an implant.
The percentage was slightly less in the AT with previous RCT for the FPPS, ranging between 50% to 81.8% for RESTO Conservative orthograde RCT demonstrates favorable oand 84.6% for PERIO. However, it had the same percentages for PT with previous RCT. In addition, the percentage was so high and reaches almost 100% in the treatment of PT with no previous RCT in terms of the RCT with restoration option among most FPPSs (Graph 3). Multiple studies indicating that RCT teeth with restored reaming cusps have better survival than those restored with crown restorations are available [3, 27].
Long-term studies with a broad range of carefully defined outcome criteria are needed. Owing to the limitations of the included study, the tentative conclusions of the authors are appropriate and likely to be reliable. Further studies are recommended to compare the different scenarios of RCT and other choices between different graduated students from different schools, general practitioners with different years of experiences and post-graduate students from different specialties.
CONCLUSION
The current survey scopes that dentists and dental interns from both genders preferred RCT with restorations over extraction then implants in the AT with and without previous RCTs. In the PT with no previous RCT, all the respondents agreed that RCT and restoration were preferable than extraction then ISCs, while equal percentages were recorded for the treatment choices for PT with previous RCTs. Among the FPPSs selected (ENDO, PROS, PERIO and RESTO), the respondents had an absolute agreement for RCT and restoration as a chosen treatment for the four scenarios. All options should be viewed as complementing and not competing factors. They should serve as an overall goal in treatment, which includes long-term health benefits for the patient’s function, comfort, and aesthetics. To achieve these goals, dentists and interns must be fully aware of the actual long-term outcomes of RCT and restorations versus extraction then ISC.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Ethics Committee of the Director of Health Affairs in the related region approved the study proposal.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from the patient prior to being enrolled in the study.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


