All published articles of this journal are available on ScienceDirect.
Efficacy of Dental Implants Placements between Lateral and Crestal Sinus Lift Techniques: A Split-Mouth Study
Abstract
Background:
Bone atrophy and pneumatization of the maxillary sinus resulting from tooth loss, associated with low bone density in the region, do not usually allow adequate quantity and quality for the installation of osseointegrated implants.
Objective:
To evaluate the efficacy of crestal and lateral sinus lift techniques which are performed on same patients.
Materials and Methods:
Ten patients who required both crestal and lateral approaches in 20 sinus lifts were selected; 31 endosseous dental implants were placed into these patients, with a reported timeline for each approach. Assessment of the surgical procedures in all patients was done using a Visual Analog Scale (VAS). Clinical and radiographic parameters, including Pocket Probing Depth (PPD), distance between the implant shoulder and the mucosal margin (DIM) and distance between the implant shoulder and first visible bone-implant contact (DIB), were analyzed to compare implant survival for both approaches.
Results:
All implants were successfully osseointegrated. No significant differences were observed between lateral and crestal approaches in PPD, DIM and DIB (p-values = 0.0504, 0.7784 and 0.18170, respectively), and in the total VAS scores (p-value ≥ 0.05). Most of the patients preferred the crestal approach due to the delay in implant placements with the lateral approach.
Conclusion:
Evaluation of the sinus floor elevation is more precise when both techniques are performed on the same patient. Furthermore, although post-operative vertigo is a major concern with the crestal approach; patients preferred this approach over the lateral technique because it is less invasive and required less time for the procedure.
1. INTRODUCTION
An implant-supported dental prosthesis can be a viable treatment option when there is sufficient quantity and quality of bone. The limitations of dental implant placement in the posterior maxilla, due to alveolar ridge resorption and excessive maxillary sinus pneumatization, can be overcome by maxillary sinus floor elevation. Maxillary sinus floor elevation was initially described by Tatum at the Alabama Implant Conference in 1976 and was subsequently published by Boyne in 1980 [1-4]. Since its first description, numerous articles have been published in this field regarding different grafting materials, modifications to the classic technique and comparisons between different techniques [5-8].
Currently, two main approaches to the maxillary sinus floor elevation procedure are widely practiced. The first approach is the classic lateral antrostomy, and the second is the conservative Osteotome Sinus Floor Elevation (OSFE) [9]. Maxillary sinus elevation to facilitate the placement of dental implants (OSFE) has gained widespread acceptance because the technique is less invasive and less time consuming [9]. A residual alveolar ridge of 5 mm is the minimum bone height required to consider the OSFE technique over the lateral approach [10, 11]. Discomfort during the infracture of the sinus floor, intra-operative or post-operative dizziness, tinnitus, disorientation, nausea, vomiting, and vasovagal syncope are the main complications specific to OSFE [12].
Patients requiring both OSFE and lateral antrostomy procedures on either side of the maxilla, as per current practice guidelines, constitute a very rare group. The quality and quantity of the maxillary residual ridge are the key factor in deciding between the two techniques in all patients [13]. Clinical and radiological assessments are utilized to evaluate the quality and quantity of the residual ridge. Both techniques have considerably variable procedural success rates, and patients’ appraisal of the techniques can also vary considerably. Although many studies have compared and contrasted lateral window versus OSFE approaches for sinus lift procedures, a split-mouth study in the same patients has not yet been attempted. A split-mouth study, which is a self-controlled study design, is preferred because it eliminates sources of bias that occur in similar controlled studies [14-16]. Therefore, the aim of this study was to evaluate the efficacy of crestal and lateral sinus lift techniques which are performed on same patients.
2. MATERIALS AND METHODS
2.1. Ethical Approval of the Study Protocol
Approval for the study was granted by the Ethics Committee of the Medical Association for the Military Hospital. The committee met after the completion of the study and approved the study for publication.
All of the patients were informed about the aims and protocol of the study, and provided proper consent. All bilateral sinus lift cases in the center during the period from 2006 to 2012 were considered. Patients were selected according to the inclusion criteria, from a group of sixty patients recruited from the same center [17].
2.2. Inclusion Criteria
- Patients who required a bilateral sinus lift for implant treatment in the posterior maxilla.
- Patients who underwent an OSFE procedure without placing grafting material when the RBH was equal to or greater than 5 mm.
- Patients who underwent a lateral sinus lift procedure if the RBS was a minimum of 2 mm and a maximum of 4 mm.
- Patients who required a bilateral sinus lift, with one side indicated for OSFE and the other side for a lateral approach, as per the previous criteria.
- Patients who require at least 1 mm of bone on each side for implant stability.
- Patients free from any systemic or local contraindications for dental implant placement.
2.3. Exclusion Criteria
- Patients who required a bilateral sinus, in whom both the right and left sides were indicated for OSFE per current practice guidelines [9].
- Patients who required a bilateral sinus, in whom both the right and left sides were indicated for sinus lift by the lateral approach per current practice guidelines [10, 11].
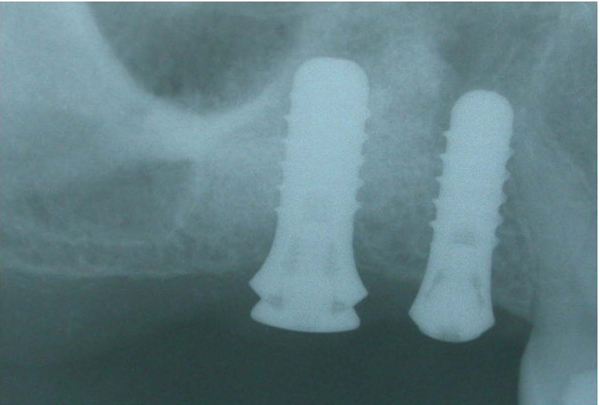
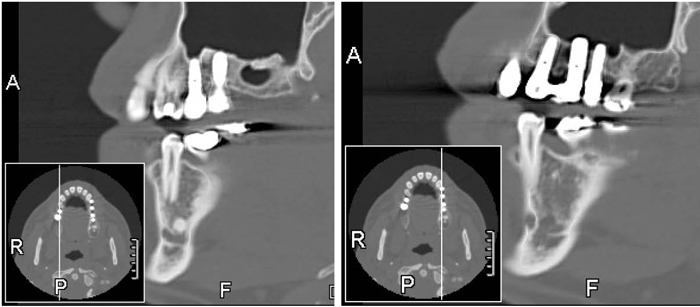
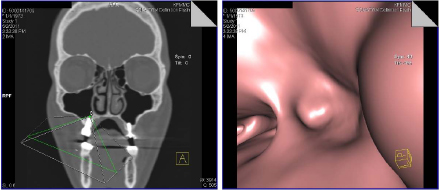
Ten patients were selected out of the sixty patients previously recruited. Thirty-one dental implants were inserted into seven men and three women (Table 1). Their ages ranged between 38 and 68, with a mean age of 53 years old. These patients presented with bilateral edentulous spaces in the posterior maxilla with reduced residual bone height, making standard implant placement impossible. These patients have lost their teeth due to periodontal diseases, caries, trauma or endodontic failures. All of the patients were treated bilaterally via elevation of the sinus floor to place implants in the posterior maxilla, using both techniques chosen on a random basis by two operators. Pre-operative records included orthopantomography (Fig. 1), intraoral photographs and study casts. Computed tomography (CT) scans were obtained using SOMATOM Definition Flash (Siemens, Forchheim, Bavaria, Germany) with Syngo Dental CT software (Syngo Somaris/ 7 version VA 40A_10_P15, 2011). All the patients’ images were obtained with SOMATOM Definition Flash software after the procedures. Local anesthesia was used for all patients. Soft tissue parameters were obtained to compare the peri-implant soft tissue conditions and marginal bone levels between the two approaches. The patients’ appraisals of both techniques were assessed using a Visual Analog Scale (VAS) questionnaire. The survival of the placed implants was evaluated by standard measurements [18].

2.4. Surgical Procedures
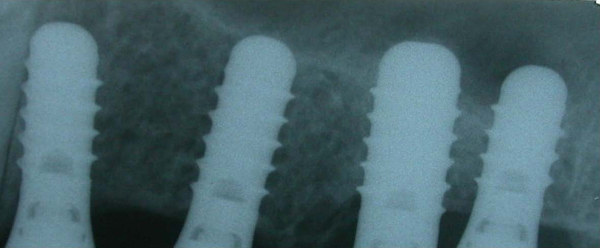
Local anesthesia was administered in the buccal and palatal regions of the surgical area. For the lateral window approach, access to the lateral maxillary wall was achieved via a mucosal crestal incision and anterior and posterior releasing vertical incisions. A bony window was elevated with a round diamond bur on the lateral wall of the maxillary sinus. The window was then carefully removed. After dissection and elevation of the sinus membrane, bovine bone mineral (Bio-Oss; Geistlich) was used to fill the sub-membranous space. Bio-Oss is produced by Osteohealth Co. (Shirley, NY 11967) (Fig. 2). The bony window was replaced and closed with monofilament sutures. The implants were placed after a period of up to 8-9 months to allow for graft maturation (Figs. 3 & 4). A standard OSFE technique was initiated for the other side of the posterior maxilla for the same patients. A mid-crestal incision was performed for flap elevation; vertical and periosteal release incisions were avoided. Cortical bone marking, for site positioning, was performed with 3 round burs of increasing diameters from 1.4 to 3.1 mm. A 2.8 mm-diameter sinus osteotome (Straumann AG, Basel, Switzerland) was performed to push the sinus floor axially. The use of osteotomes, rather than drills, prevented ovalization of the implant bed in the limited residual bone. The sinus floor was then broken by light strokes using a mallet and carefully pushed into the sinus cavity to a maximal height of 3 mm; the Schneiderian membrane was further elevated by implant placement. The osteotomy site was enlarged by the 3.5 to 4.2 mm-diameter sinus osteotome, based on the implant placement in the prepared osteotomy sites. The integrity of the membrane was controlled with an undersized depth gauge of 2.1 mm. No grafting material was used in any of the cases. Implant insertion was performed without tapping. All of the patients underwent open-flap procedures for implant placement. ITI SLA solid screws (Straumann Ch Company of Basel, Switzerland manufacturer), 4.8 or 4.1 mm in diameter, were used for both sides. The flaps were sutured, and all of the implants achieved primary stability. The healing period was lengthy but uneventful. After surgery, the patients were asked to sit up comfortably in the dental chair and to rest for 30 minutes. The patients who were experiencing vertigo were asked to rest and sit up comfortably in the dental chair for an additional 15 to 30 minutes prior to discharge from the clinic to make sure that the patients are not experiencing vertigo after this time. Multiple Valsalva tests were performed in all of the cases to check for patency of the Schneiderian membrane immediately following the procedure. The patients were also instructed not to wear their dentures for 2 weeks post-operatively. Antibiotics (amoxicillin 500 mg every 8 hours) were prescribed for 7 days, analgesics were given as needed, along with an antiseptic rinse with 0.2% chlorhexidine twice daily. The sutures were removed 7-10 days after surgery. Post-operative investigation records included X-rays (Figs. 5 & 6), intraoral photographs, and survival rate chart of all implants for up to 24 months.



| Patient Number | Lateral Window Technique | Osteotome Technique | Total | Preferred Approach | ||
|---|---|---|---|---|---|---|
| No. of Implants | *Operation Time (min.) | No. of Implants | Operation Time (min.) | |||
| Patient # 1 | 2 | 75 | 3 | 45 | 5 | Did not reveal any preference |
| Patient # 2 | 2 | 70 | 1 | 31.5 | 3 | Crestal |
| Patient # 3 | 1 | 68 | 1 | 30.5 | 2 | Crestal |
| Patient # 4 | 2 | 80 | 2 | 33 | 4 | Crestal |
| Patient # 5 | 1 | 63 | 1 | 25.5 | 2 | Crestal |
| Patient # 6 | 2 | 84 | 2 | 34 | 4 | Crestal |
| Patient # 7 | 2 | 78 | 1 | 24 | 3 | Crestal |
| Patient # 8 | 1 | 67 | 1 | 27 | 2 | Crestal |
| Patient # 9 | 2 | 84 | 1 | 26 | 3 | Did not reveal any preference |
| Patient # 10 | 1 | 72 | 2 | 30 | 3 | Crestal |
| Total | 16 | - | 15 | - | 31 | - |
| - | - | Average = 74.1 | - | Average = 30.65 | - | Differences 43.45 min. |
| - | - | SD = 7.294 | - | SD = 6.05 | - | 1.244 |
Impressions were taken after a healing period of 6-9 months after implants insertion. Prosthetic abutments were inserted with 35 Ncm of torque, and restorations were delivered (Figs. 7 & 8). A Computed Tomography (CT) scans were obtained 48 months after loading the last implant.


2.5. Patients’ Perceptions
After the surgical procedures, all of the patients were asked to provide their feedback on the surgical procedures and implant therapy. The patients were asked 14 questions and instructed to evaluate, criticize and compare both surgical approaches to determine subjective perceptions of maxillary sinus lift post-surgery expectations using a VAS scale. The VAS score of “0” indicates ‘total acceptance or no inconvenience’ and “10” indicates ‘total refusal, unpleasant or painful feelings’ [19]. The average VAS score for each question was calculated and analyzed using the paired t-test to provide corresponding p-values. The timeline for each surgical procedure was also recorded (Table 1).
2.6. Clinical Examinations
At the annual clinical examination after functional loading, the survival of the implants and reconstructions were evaluated using the following clinical parameters:
- Pocket Probing Depth (PPD) in millimeters measured at four sites per implant;
- Distance between the implant shoulder and the mucosal margin (DIM), measured at all four sites of implantation (recession scored as a negative value); and
- Distance between the implant shoulder and first visible bone-implant contact (DIB).
All of the soft tissue measurements (made to the nearest millimeter), were performed using a UNC-15 periodontal probe (Hu-Friedy, Chicago, IL, USA).
2.7. Radiographic Examinations
All patients were recalled and programmed after the sinus lift procedure, implantation and prosthetic rehabilitation for orthopantomographic and intraoral radiographs, every 6 months for the first year. The radiographs were utilized to measure DIM and DIB. CT scans were obtained 48 months after loading the last implant.
The analysis of the data was performed using SPSS software, version 20.0. Unpaired t-tests were applied to compare the mean PPD, DIM and DIB between the bilateral sinus lift implant techniques with the p-value ≤ 0.05 was considered significant.
3. RESULTS
All of the patients underwent similar procedures, with successful single attempts for both techniques (Figs. 9 & 10). Note that case number 3: one of the implants at the osteotome side was not included, because it was not in the lifted sinus area). In the lateral window approach, implants were placed during second intervention. Out of 31 ITI solid screw implants 4.1 mm and 4.8 mm in diameter, 15 implants were utilized for OSFE, and 16 implants were used for the lateral approach. The implant lengths used were 10 mm and 12 mm in both techniques. At the time of abutment connection, all of the implants were stable. The mean follow-up period was 36 months after permanent prosthetic insertion. During follow-up period, all implants and prostheses were stable and functional, no pain or swelling were noted in any of the cases before or after prosthetic loading.
3.1. Survival Failure Rates
There were no complications associated with the surgical procedure; such as infection of the maxillary sinus, loss of bone particles through the nose, wound dehiscence, and/or loss of the implants’ initial stability. One sinus membrane perforation was noted during the lateral window approach but was not considered a complication related to the surgical procedures as it was a minimal perforation noted at the initial bur hole region. The perforation was managed by leaving the membrane folded over itself while lifting the sinus membrane, thus obviating the need for repair. All of the implants presented had radiologically proven osseointegration and thus received single crowns or fixed prostheses. All of the implants successfully fulfilled the Buser et al. criteria [18].
3.2. Radiographic Assessments
Linear measurements were obtained to evaluate the marginal bone levels. The DIB was measured. None of the periapical radiographs revealed any peri-implant radiolucency during the follow-up period. However, minimal crestal bone loss was noticed six to nine months after loading. There were no significant differences in the marginal bone levels between the lateral window and the OSFE implants. Radiographically, the apical elevation of the sinus floor for both approaches was observed. There was predictable radiography bones/graft established around the implant apex in cases completed with the lateral approach. There were no obvious confirmations seen of bone formation between the lifted sinus membrane and the implant apex.
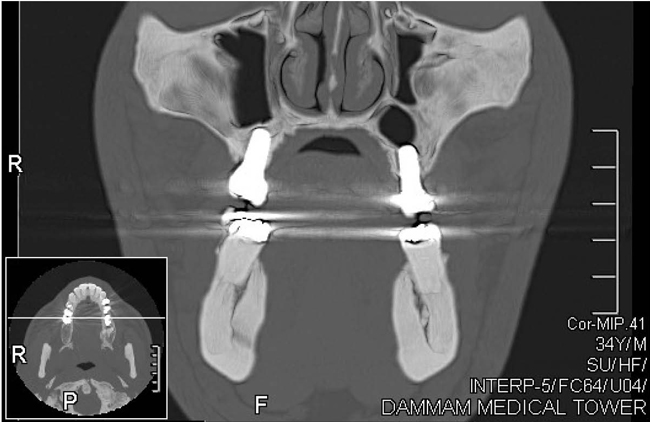
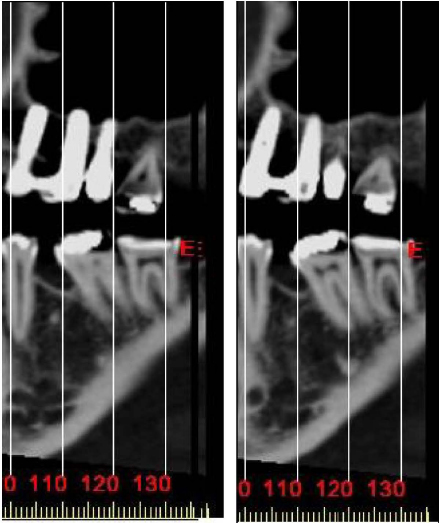
CT scans showed the amount of bone gained bilaterally by both techniques, as shown on right and left sagittal CT films (Fig. 11) and coronal CT scans (Fig. 12). The reformatted fly-through image of the maxillary sinus floor (Figs. 13 & 14) showed an intact Schneiderian membrane over the projection of the apical border of the implant at both sides. After two years of prosthetic loading, periapical radiographs showed a stable clinical situation in the area around the apices of the implants on both sides. A dome-shaped structure was apparent at the sites of the first and second molars on the left side (Fig. 15). Selected magnified images from CT scans showed the apical borders for these implants, the surrounding bone, and the new sinus floor 2 years after surgery using the staged OSFE technique on the left side (Fig. 16). No peri-implant radiolucency was distinguished in any of the cases.




3.3. Peri-Implant Soft Tissue Condition
Using 2-tailed independent samples t-tests, there were no significant differences between the two approaches (lateral and osteotome) in the averages of 3 indices (PPD, DIM and DIB). The p-values of the tests for PPD, DIM and DIB were 0.0504, 0.7784 and 0.1817, respectively. The proximities of these averages in the 3 indices comparing the two approaches to the boundaries are shown in Table 2. The mean and standard deviation for the marginal bone level of the lateral window implants was 2.67 ± 0.95 mm, compared with 2.75 ± 0.95 mm for the OSFE implants. The mean and standard deviation of PPD for the implants with the lateral window approach was 3.83 ± 0.348 mm, compared with 3.55 ± 0.406 mm for implants using the crestal approach. The mean and standard deviation for DIM for implants with the lateral window approach was 0.356 ± 0.784 mm, compared with 0.447 ± 0.613 mm for implants with the crestal approach. The mean and standard deviation for DIB for implants with the lateral window approach was 2.85 ± 0.465 mm, compared with 2.64 ± 0.397 mm for implants with the crestal approach (Table 2).
Statistically, there was no significant difference in the mean mesial and distal PPD between the lateral and osteotome bilateral sinus lift implant techniques. Additionally, there was no significant difference in the mean DIM for the buccal, lingual, mesial or distal aspects between the two sinus lift implant techniques (p > 0.05) and the mean mesial and distal DIB between the lateral and osteotome bilateral sinus lift implants (p > 0.05). Finally, there were no significant differences in the average PPD, DIM, and DIB between the lateral and crestal approaches (Table 2 and Fig. 17).
| Variables |
Lateral (n = 16) |
Osteotome (n = 15) |
P-Value |
|---|---|---|---|
| Pocket Probing Depth | |||
| • Buccal | 3.78 ± 0.329 | 3.55 ± 0.421 | 0.099 |
| • Lingual | 3.78 ± 0.368 | 3.41 ± 0.531 | 0.031 |
| • Mesial | 3.92 ± 0.415 | 3.64 ± 0.511 | 0.103 |
| • Distal | 3.81 ± 0.398 | 3.59 ± 0.398 | 0.130 |
| • Average | 3.83 ± 0.348 | 3.55 ± 0.406 | 0.0504 |
| Distance between implant mucosal margins | |||
| • Buccal | -0.356 ± 0.666 | -0.447 ± 0.596 | 0.694 |
| • Lingual | -0.381 ± 0.779 | -0.360 ± 0.722 | 0.938 |
| • Mesial | -0.356 ± 0.784 | -0.447 ± 0.613 | 0.724 |
| • Distal | -0.356 ± 0.764 | -0.467 ± 0.595 | 0.658 |
| • Average | -0.363 ± 0.722 | -0.431 ± 0.594 | 0.777 |
| Distance between the implant shoulder and first visible bone-implant contact | |||
| • Mesial | 2.88 ±0.536 | 2.56± 0.484 | 0.084 |
| • Distal | 2.81 ±0.444 | 2.71± 0.456 | 0.552 |
| • Average | 2.85 ±0.465 | 2.64± 0.397 | 0.184 |

3.4. Patient-Centered Outcomes
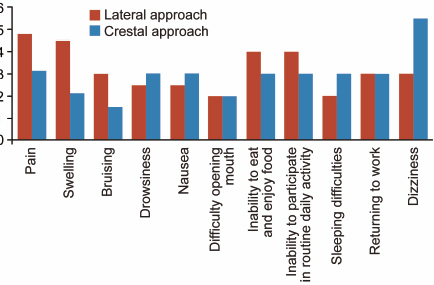
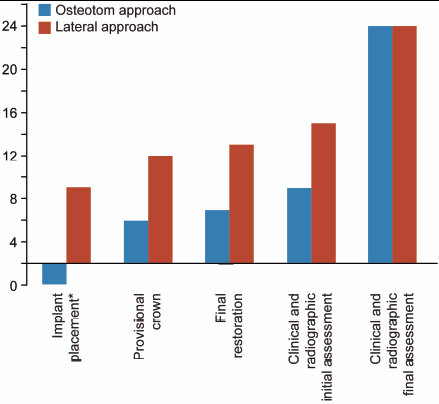
All 10 patients actively participated in evaluating, criticizing and comparing both surgical procedures which included general satisfaction, nausea, vertigo, pain and discomfort after the surgical procedures. Using the VAS scale, with “0” to indicate ‘total acceptance or no inconvenience’ and “10” to indicate ‘total refusal or unpleasant or painful feelings.' Concerning general satisfaction, the questionnaire consisted of 14 questions concerning the two approaches. All of the patients had receptive attitudes toward the questionnaire, and all ten patients answered all of the questions about both approaches. The provided mean and standard deviation for the VAS score for all of the questions related to the lateral approach was 2.92 ± 1.050, compared to 3.2 ± 0.9751 for the crestal approach (P ≥ 0.05). The analysis demonstrated no statistically significant difference in the total VAS scores between the lateral and crestal approaches (Table 3 and Fig. 18). The timeline of the study for both crestal and lateral approaches within 36 months was shown in (Fig. 19), which demonstrated the implant placement for lateral approach 8-9 months after sinus floor elevation with a Bio-Oss graft. None of our patients required any medications for such complaints. In the overall assessment, eight of the ten patients preferred the OSFE over the lateral approach with the remaining patients not revealing any preference (Table 1).
|
Average VAS Scale for each Question Lateral Approach |
Average VAS Scale for each Question Crestal Approach |
Questionnaire for each Symptom Score from 0 to 10 | - |
|---|---|---|---|
| 4.8 | 3.1 | Pain | 1 |
| 4.5 | 2.1 | Swelling | 2 |
| 3 | 1.5 | Bruising | 3 |
| Negligible (0) | Negligible (0) | Nasal bleeding | 4 |
| 2.5 | 3 | Drowsiness | 5 |
| 2.5 | 3 | Nausea | 6 |
| 2 (highest level on 1st day) | 2 (highest level on 1st day) | Difficulty with mouth opening | 7 |
| 4 (highest level on 1st to 3rd days) | 3 (highest level on 1st to 3rd days) | Inability to eat and enjoy food | 8 |
| 4 (highest level on 1st to 3rd days) | 3 (highest level on 1st to 3rd days) | Inability to participate in routine daily activity | 9 |
| 2 | 2 | Sleeping difficulties | 10 |
| 3 (sick leave for 3 days) | 3 (sick leave for 3 days) | Returning to work | 11 |
| 3 | 5.5. immediately after surgery, lasted a maximum of 30 min. | Dizziness (vertigo) | 12 |
| Negligible (0) | Negligible (0) | Difficulty in nasal airflow at the sinus lift area | 13 |
| Negligible (0) | Negligible (0) | Breathing, swallowing, and speech difficulties | 14 |
| Average = 3.2 | Average = 2.92 | - | - |
| SD = 0.9751 | SD = 1.050 | P-value = 2.22 | - |
4. DISCUSSION
This article is the full version of a previous short communication published earlier [20]. Being this was a split-mouth study, the comparison of both techniques in the same patients proved that the symptoms seen only in the OSFE group may be specific to the technique. The crossover effect of learned memory in the split-mouth design is one of the limitations of this study [14]. Checchi et al. conducted a randomized clinical trial with a split-mouth design to compare the Summers and Cosci techniques in crestally augmented sinuses with particulate cancellous human allografts [17]. To reduce the crossover effect, all of the patients were educated regarding the procedural steps, and they provided informed consent for both techniques prior to the first procedure. The crossover effect might have been further reduced in this study because six of the ten cases had crestal approaches followed by OSFE, whereas remaining four patients had OSFE procedures before the crestal approach. Patients who experienced OSFE-associated symptoms during and after the OSFE did not experience any of these symptoms with the lateral approach. However, all of the patients recovered from these symptoms after 30 to 60 minutes. It was interesting to note that based on their responses, none of the patients were concerned about this transient discomfort.
Average difference in operation time between the two techniques: 43.45, SD: 8.254. *Operation time for the lateral approach is the total time for two stages (1st stage: sinus lift with Bio-Oss graft and 2nd stage: surgical implant placement).
The symptoms of vertigo can require pharmacological management to reduce the spinning sensations and/or to reduce the accompanying nausea. The most commonly used drugs are anxiolytics, sedatives, and/or muscle relaxants, along with antihistamines. Antihistamines appear to have suppressive effects on the central emetic center, relieving nausea and vomiting associated with motion sickness [21]. None of our patients required such medications. To prevent this complication, a gentle hammering should be performed, and a careful approach should be taken during the osteotome technique. Patients should be informed regarding the possibility of post-operative vestibular symptoms, because these symptoms can be very unpleasant and may cause considerable stress if the patient was not previously informed of this problem. Although not indicated in this study, if the symptoms are incapacitating, immediate referral to an otorhinolaryngologist is recommended [22-26].
There was no significant difference in the total VAS scale between the crestal and lateral approaches; P = 2.22.
The time required for implant placement after the lateral approach was mentioned negatively in the responses of all of the patients to the questionnaire. This finding might have been influenced by the current expectations of patients in this era of immediate loading implants. Although a delay in implant placement was the main reason for preferring OSFE over the lateral approach, the lateral approach was the choice of patients who feared the development of such symptoms and of patients who could not tolerate the discomfort of hammering. This finding also emphasizes the importance of disclosing all vestibular symptoms when presenting the OSFE procedure to the patient.
Different techniques have attempted to reduce the force exerted during the fracture of the nasal floor in OSFE. Romanos described a technique for window preparation for the sinus lift procedure [27]. A round bur was used to prepare the osteotomy under continuous saline solution irrigation. Various techniques are now being used to reduce the membrane perforation, including the use of piezosurgery, hydrostatic force, laser surgery, various modifications of hammer osteotomes, and more precise radiological evaluation during surgery. All of these techniques could also reduce the perforation rate in OSFE [28-37].
Radiological evaluation revealed sufficient lifting of the sinus floor by both techniques. Radiological evidence of the presence of bone over the implant apex was proved by CT scans for all of the patients. Radiological evidence of bone formation at the apex of the implant on periapical radiographs was not always confirmed in the OSFE cases, whereas with the lateral technique, sufficient bone could be observed above the implant apex. Nevertheless, there has been no inconclusive clinical evidence to prove any advantage of bone over the implant apex directly affecting implant survival in any of the sinus lifting procedures [38, 39].
Although various biomaterials are currently being used to augment beneath the lifted sinus membrane in both the OSFE and lateral techniques, biomaterials were not utilized after OSFE in this study. Piero et al. assessed the clinical outcomes of sinus membrane elevation in combination with implant placement without any biomaterials [40]. Although the regeneration of bone was not uniform, the height of the membrane lift did not correlate with the amount of regenerated bone, and the success rate was not affected. However, with the lateral approach without simultaneous implant placement, grafting material is often necessary to support the sinus membrane [41-44]. Membrane perforations were easily visualized with the lateral approach compared to the OSFE, whereas with OSFE, other clinical parameters, including the Valsalva test, were utilized to confirm membrane integrity. Some authors believe that tearing of the Schneiderian membrane was a factor that diminished implant survival rate [45]. Hernandez-Alfaro et al. observed an implant survival rate that was inversely proportional to the size of the perforation [46]. However, some authors did not report tearing of the membrane to be a negative factor in the survival rates of implants [47]. Schwartz-Arad et al. reported that tearing of the membrane influenced the occurrence of post-surgical complications but did not influence the survival rate of the implants [48]. Membrane integrity has considerable significance in the lateral approach, because it limits the amount of sinus graft material inserted into the zone, improving implant survival and reducing complications. Ardekian et al. did not find significant differences in implant survival rates between implants inserted in a grafted sinus with a perforated membrane and in a sinus with an intact membrane [47]. The criteria used to select the lateral technique over OSFE were the residual bone height and the predicted initial stability, rather than avoidance of membrane perforation by direct visualization [49, 50]. One of the ten cases in this study had a membrane perforation during the lateral approach. However symptoms such as nasal bleeding, graft escape or nasal congestion were not reported in this case.
Radiological data were used to assess implant success. The Periotest apparatus has been shown to be successful in assessing the stability of implants. However, it often fails to detect cases with saucerization of the bone. Radiographs can show the bone levels of implants. It was found that, although an implant was stable, it might have suffered significant horizontal bone loss [51, 52]. The quality and quantity of the bone covering the implant apex might prevent the effects of tangential forces applied on loaded implants, which could eventually initiate crestal bone loss. In OSFE, because there is no marked bone formation around the implant apex, these tangential forces can apply more rotational force, with a fulcrum situated toward the crestal bone, compared to an implant inserted using the lateral approach, in which a bone graft is used [38, 39]. The distinguishing of the bone created when replacing the bone graft with the lateral approach was different from the bone created around the implant with the OSFE approach. However, such a comparison was beyond the scope of the study. Nevertheless, there were no significant differences noted in the measurements of PPD, DIB or DIM between the two techniques. No implants were lost, and no significant differences were detected among the studied variables, and no or reduced crestal bone resorption was seen in one-year post-operative radiographs; therefore, the procedures were considered to have attained implant success, per Buser et al.’s criteria [19]. This was a split-mouth study that challenged a meticulous and direct assessment of both techniques for maxillary sinus lift. A split-mouth design with a larger sample size, directly comparing OSFE to the lateral approach with immediate implantation, could be considered in future studies.
CONCLUSION
Maxillary sinus floor elevation with both the crestal and OSFE techniques could be evaluated precisely when both techniques were performed in the same patient. Although the small sample size for a split-mouth study was a limitation, the specific advantages, disadvantages and indications for each technique could be distinguished. No significant differences were observed in PPD, DIM, and DIB when assessing implant survival using clinical and radiological assessments. Approximately 33.3% of the patients experienced vestibular discomfort during the OSFE procedures; however, no significant differences were noted in implant success between the two approaches. Approximately 80% of the patients preferred the OSFE approach over the lateral approach due to the delay in implant placement with the lateral approach.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Ethics Committee of the Medical Association for the Military Hospital, Saudi Arabia approved the study for publication. (Research Ethics Committee REC Number: kfmmc-dd18/05/2011)
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All research procedures on humans were followed in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013. (http://ethics.iit.edu/eco des/node/3931)
CONSENT FOR PUBLICATION
The participants provided written informed consent.
AVAILABILITY OF DATA AND MATERIAL
The authors confirm that the data supporting the findings of this study are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


