All published articles of this journal are available on ScienceDirect.
Chronic Submerged Implant Infection Treated with Immediate Implantation and Guided Bone Regeneration: A Case Report
Abstract
Introduction:
Early implant infection and failure can be addressed by either implant maintenance or immediate replacement and bone regeneration at the defect site.
Methods:
In this study, six patients with chronic sinusitis at the implant site were treated with implant removal and curettage to remove the infected and inflamed soft tissue. A new implant was immediately screwed into the same socket, and a Guided Bone Regeneration (GBR) procedure was performed to regenerate the lost bone at the site. After the patients underwent the second surgery, the sinusitis disappeared, and new bone formed around the implant, achieving good implant stability.
Conclusion:
The implant was loaded, and no complaints were reported during the follow-up period. Chronic implant infection treated with implant removal and immediate replacement plus GBR resulted in stable new implants with new bone formation.
1. INTRODUCTION
The etiology of early implant failure varies from contamination to bone overheating during drilling, poor implant stability, insufficient bone volume, infection, dentist inexperience, abnormal bone remodeling, and compromised patient conditions [1]. Meanwhile, early stage implant infection may be due to surgical site contamination, previous periapical lesion or infection of the extracted tooth, root canal treatment of the extracted tooth, periapical infection of the adjacent tooth or even drilling debris [2]. There is more than one treatment option for implants in the early stage of failure: the implant can either be preserved and disinfected or replaced with a new implant. The decision to keep or replace the compromised implant depends on many factors, such as the amount of hard and soft tissue available, implant stability, cost, time and the medical condition of the patient. Several studies have found that the success rate of the second implant is lower than that of the first implant placed in pristine bone [3]. However, the treatment of implant failure without removal may not lead to a complete cure, and the infection may persist [4]. In this study, we tried to treat implant failure by placing a new implant and performing Guided Bone Regeneration (GBR) to eliminate the infection and regenerate the site.
2. CASE REPORT
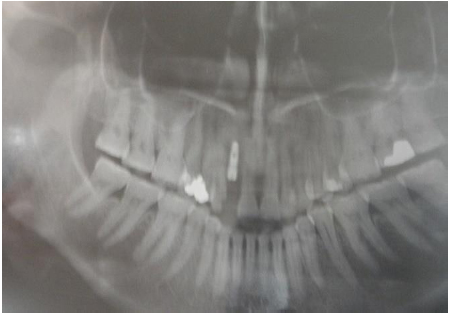
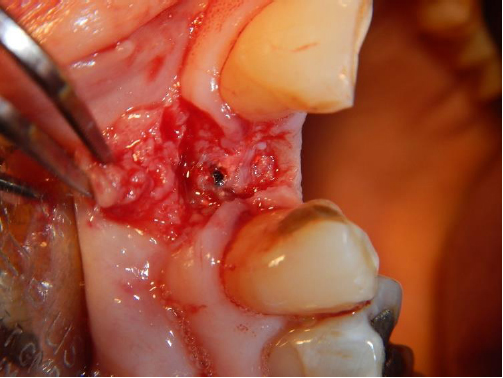
The patient was a 45-year-old woman with no history of any systemic disease, and she was not a smoker. The patient presented to our facility complaining about the sinus tract at the site where an implant was placed 4 months prior at the upper right lateral incisor (Fig. 1). The implant was placed by another dentist, and the sinus showed pus discharge one month after implant placement. The patient was treated with antibiotics every time the sinusitis appeared, which disappeared after antibiotic treatment and reappeared after a period of time. The patient refused to continue treatment with the previous dentist; thus, she was referred to our clinic for further treatment. An orthopantomogram was taken to detect any osseous lesions or sites of bone resorption, and crestal bone resorption was found (Fig. 2). The decision regarding implant removal and replacement along with guided tissue regeneration was discussed with the patient. Written consent was obtained from the patient for the surgery and the publication of her data. Under local anesthesia, a three-sided flap was elevated, and all of the infected granulation tissue around the implant was removed. The implant was removed without bone removal using a ratchet with a forward movement (insertion torque); then, reverse torque was applied to remove the implant from the socket. The implant started to rotate when low torque was applied (15 Ncm), and examination of the implant after removal showed that the implant surface had not attached to the bone (Fig. 3). Through irrigation with normal saline, curettage was performed in the socket (Fig. 4). A new implant with an aggressive design (Dentium, SuperLine) was placed and immediately demonstrated good primary stability (45 Ncm). The implant placement was the same as that immediately after tooth extraction, engaging the palatal bone and the apical area. Several threads of the implant at the crest were exposed buccally (Fig. 5). Decortication and perforation of the labial bone with a burr were performed to identify the bleeding point on the bone. The GBR technique was performed using a resorbable collagen membrane (GENOSS, Gyeonggi-do, South Korea) and a hydroxyapatite-B tricalcium phosphate (HA 70% + β-TCP 30%) bone graft (GENOSS, Gyeonggi-do, South Korea). Periosteum scoring was performed at the base of the flap, and tension-free closure was achieved. The antibiotic treatment consisted of amoxicillin/clavulanate 625 mg and metronidazole 500 mg, and Ibuprofen 400 mg was administered for pain. The sinus tract infection disappeared after one month of healing (Fig. 6). Second-stage surgery was performed after six months; when the flap was raised, new bone was observed to have formed around the implant buccally (Fig. 7). The cover screw was removed, and the healing abutment was placed. After one month, an impression was made with the closed-tray technique and sent to a laboratory for the fabrication of a metal crown fused to porcelain. The crown was placed on a straight abutment (Fig. 8) and cemented with zinc phosphate cement, and the occlusion was checked. Post-implantation radiographs show the proper prosthetic setting and crestal bone level (Fig. 9). The patient was motivated to maintain good oral hygiene.







3. DISCUSSION
The definition of early implant failure is failure occurring before or at the time of abutment, such as an inability to establish close bone to implant contact [5].
It is crucial to differentiate between failed and compromised implants, as the former need to be removed, while the latter can be preserved and treated. The main difference between the two conditions is that implant mobility can be found at any stage during implant failure.
Because the first implant was not placed by our group, the cause of the infection was difficult to determine. As our patient had no medical problems and did not smoke or drink alcohol, the cause of the infection was most likely local.
Infection of the sinus tract at this stage has many causes (Table 1), such as the entrapment of soft tissue between the implant shoulder and the cover screw during cover screw placement.
Another cause of infection is the placement of an implant at the site of a previous root canal or periapical infection or lesion. Most of these lesions are found in the periapical area of the implant, where the bacteria reside [6, 7]. Most likely, the etiology of the infection in our case was overheating during drilling, which leads to not only sinus discharge but also a lack of osteointegration and soft tissue formation around the implant [1].
In the current case, we used a second implant with the same diameter as the failed implant but with a different design (aggressive), and we placed the implant more palatally using the same technique as used for the immediate implant (Table 2).
In contrast, in another study [8], the failed implant was immediately replaced with a wider and longer implant. In our case, we chose to remove the implant because it was not yet loaded, and there was no prosthesis to lose. In addition, the implant was not very stable and thus had a high chance of losing stability after loading. The implant was removed by applying torque to the implant with a ratchet in the insertion direction and then applying reverse torque, which is a very safe procedure for removing a failing implant while maintaining the surrounding bone (Table 2).
The survival rate of implants placed at the site of a previous implant failure varies depending on the time and number of failures. A review performed by Gomes et al. [3], reported a low survival rate of implants placed at the site of late implant failure and for implants placed after a second and third implant failure. However, the survival rate of implants placed at the site of early implant failure or a first implant failure was more than 90% [3].
A study performed by Grossmann and Levin [9] showed that the success rate of a second implant was low compared to that of the first implant placed; in that study, no bone grafting was performed, and a short implant was used [9].
In the current study, the second implant was placed in the infected site with bone resorption; however, the bone was still able to integrate with the new implant. In addition, new bone formed closely around the second implant and the dehiscence through the GBR procedure.
Other treatment modalities require removal of the infected tissue and sterilization of the implant surface followed by GBR without implant removal. There are some considerations involved in maintaining an infected implant in place, such as implant stability, the amount of bone around the implant, the medical condition of the patient and prosthetic temporization.
Nevertheless, several studies have failed to regenerate bone around an implant with peri-implantitis, especially when a mechanical debridement method was not used [4, 10]. A study performed by Persson et al. [4], showed only thick capsule formation around the implant and bone formation only when pristine cover screws were used. In our case, the GBR procedure was still considered successful upon the formation of new bone, despite the chronic infection found at the site of the previous implant.
| No. | Causes |
|---|---|
| 1- 2- 3- 4- 5- |
Overheating of the drill during osteotomy Soft tissue entrapment during cover screw placement Contamination during implant placement surgery Foreign body lifted at the site of the implant Implant placed at the site of a previously infected tooth (periapical or periodontal) |
| No. | Advantages |
|---|---|
| 1- 2- 3- 4- 5- 6- 7- |
Conservative implant removal allows immediate implantation. No bone removal minimizes the amount of bone needed for GBR. Conservative implant removal provides the opportunity for implant osseointegration. The source of infection is completely removed. The process is time consuming. Engaging the palatal bone during implant placement provides better stability and allows new bone to surround the implant. Using a second implant with an aggressive design achieves better primary stability. |
CONCLUSION
In the current case, immediately replacing the infected implant followed by GBR did not affect the prognosis of the implant or new bone regeneration.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the CARE guideline.
CONSENT FOR PUBLICATION
The participant provided written informed consent to be involved in the study.
AVAILABILITY OF DATA AND MATERIALS
The data sets analyzed during the current study are available from the corresponding author on request.
FUNDING
The funding support is by: Riyadh Dental Hospital-King Saud Medical City.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


