All published articles of this journal are available on ScienceDirect.
Analysis of the Correlation between Morphology and Kinematics of Anteriorly Displaced TMJ Discs Using Cine-MRI and ARCUSdigma Systems
Abstract
Background:
Studies of mandibular movement trajectories have provided a good understanding of the motion of the condyle but little information on the geometric relationships of the disc because they have not related the movements to anatomic structures.
Objective:
This study investigated the morphology and kinematic characteristics of the Temporomandibular Joint (TMJ) using Cine-MRI and ARCUSdigma systems.
Methods:
For this study population, preliminary clinical diagnoses were asymptomatic in 15 cases, unilateral anterior disc displacement with reduction (ADDWR) in 17 cases, and unilateral Anterior Disc Displacement Without Reduction (ADDWoR) in 14 cases. Patients were investigated with Cine-MRI and ARCUSdigma systems during physiological opening and closing of the mouth.
Results:
In these groups, there were 13 healthy subjects, 19 patients with unilateral ADDWR and 14 patients with unilateral ADDWoR classified by Cine-MRI. (1) To assess morphology by MRI, disc deformities were evaluated as follows: biplanar, rounded, thickening in the posterior band, lengthened and folded. (2) The opening trajectory for healthy subjects was close to the closing trajectory. Conversely, the incisal and condylar trajectories during opening and closing were obviously bounced, deviated or shortened in the ADDWR and ADDWoR groups. The pathway of the kinematic axis was not parallel, and the condylar trajectory had an inflexion. (3) The mean values of the incisal and condylar paths of the ADDWoR group were significantly different from those in the healthy group (P<0.05), whereas there were no significant differences between the ADDWR and the healthy group (P>0.05).
Conclusion:
This study combined analysis of the condylar pathways and disc-condylar relationship to provide good visualization of morphology and kinematics during jaw movement. This process helps improve our understanding of the complexity of disk-condylar movements in subjects with TMJ internal derangement and may also contribute to our knowledge of the etiology of TMJ internal derangement.
1. INTRODUCTION
Internal derangement of the Temporomandibular Joint (TMJ) is defined as an abnormal relationship of the articular disc to the mandibular condyle, fossa and/or articular eminence. It is a major cause of TMJ disorder and is accompanied by pain, clicking, muscle tenderness and limitations in mouth opening [1]. Jaw movement is regarded as one of the important parameters with which to evaluate the function of the TMJ [2]. Jaw movement has been analyzed using the trajectories of the incisor or condyle during mouth opening. However, analysis of the movement of the condyle is more complex as it is impossible to record its trajectory directly. It is important to mention that condylar trajectories are affected by the shape of the fossa and the disc position. The relation between trajectories of the condyle and disc deformation as a function of movement is not clear. Though anterior disc displacement is the most common disorder, its position and consequences for mandibular movement are still unclear. As jaw movements involve complex rotatory and translational movements, the location of the point chosen for analysis influences the shape of its trajectory.
During the mandible movement, the geometric relationship of the condyle-disc moves through different trajectories with respect to time and position. Mandibular motion is commonly tracked using axiography [3, 4]. With real-time axiography, a precise picture of the movement of the TMJ can be drawn at high spatiotemporal resolution. Unfortunately, this method only allows inferences about the anatomy of the TMJ from the shape of the tracings, which is complex. Furthermore, conventional static Magnetic Resonance Imaging (MRI) fails to visualize the consecutive disc and condylar movement of the TMJ. Pseudo-dynamic MRI analysis investigates the relative contribution of rotation (condylar-disc compartment) and translation (mandibular fossa-disc compartment) along with movement paths during both mouth opening and closing to allow a deeper understanding of normal articular motion [5]. MRI can be used to visualize disc morphology and position and to facilitate the interpretation of topographic changes in muscular, bones, and meniscal and ligamentous structures of the TMJ. Therefore, MRI in the open- and closed-mouth positions is the method of choice for imaging TMJ disorders [6]. It is currently regarded as the best possible diagnostic standard.
Computerized axiography is an alternative noninvasive diagnostic method that enables clinicians to record condylar movements. After localizing, the geometric hinge axis, TMJ kinematic and mandibular movement characteristic can efficiently and accurately be detected by computerized axiography, which allows the recording of jaw movements in three dimensions. This system yields an accurate description of the geometry of TMJ articular surfaces and of the dynamic variation of the intra-articular space. A number of authors have found, as a limitation, that opening the mouth may be associated with a posterior positioning of the condyle [7]. Hence, MRI and jaw tracking were combined to display the motion of the whole disc-condyle structure within the fossa, information combined TMJ anatomy with kinematic data with kinematic data recorded with six degrees of freedom. The aim of the present study was to assess the disk-condyle relationship through MRI and determine its association with the incisal/condylar trajectories in patients with TMJs with disk displacement (with and without reduction).
2. MATERIAL AND METHODS
2.1. Participants
The selected group comprised 46 subjects (19 men and 27 women; age range 21-35 years; mean age 26.4) divided into the following groups: Group I, asymptomatic TMJs (n=15), Group II, unilateral anterior disc displacement with reduction (ADDWR) (n=17), and Group Ш, unilateral Anterior Disc Displacement Without Reduction (ADDWoR) (n=14). Participants underwent MRI to clinically establish the diagnosis and to assess more fully the internal derangements and/or make a differential diagnosis of other muscle or joint disorders. The participants underwent ARCUSdigma recording on the same day that the Cine-MRI was performed, and the recording was performed at the location indicated by MRI to confirm diagnoses. Each participant was clinically screened by an independent examiner. The examiners were blind to the results of the preceding clinical screening and to the results of the other examiners.
2.2. Clinical Examination
All examinations were performed by the same practitioner and consisted of collecting data on the patient's history of joint dysfunction or pain, observation and measurement of deviations during opening, auscultation and palpation of the joint to detect abnormal clicking or popping, palpation of the muscles of mastication to evaluate tenderness, and mandibular manipulation to detect functional shifts. The participants performed at least 3 maximal opening-closing mandibular movements. Informed consent was obtained from all participants [8].
The inclusion criteria were [8-10] normal occlusion without loss of teeth, except for the third molar, with stable intercuspal relations, Angle Class I jaw relationships, and anterior teeth with vertical and horizontal overlap between 0 and 3 mm. The exclusion criteria were myofascial pain, history of trauma, previous treatment for TMJ, jaw arthritis, tooth mobility of 2 or more, and the presence of systemic diseases affecting joint and/or masticatory muscles, such as fibromyalgia or other rheumatic diseases diagnosed according to the American College of Rheumatology criteria [11]. Controls were totally free from past or present myoarthropathies of the masticatory system [12].
2.3. MRI Protocol
MRI was carried out with a 1.5 Tesla (Philips Co. Ltd) machine with a bilateral circular (8 cm diameter) surface coil for both right and left TMJs. Two positions and three sequences were obtained in static MRI: (1) the closed-mouth position (maximum inter-cuspidation of teeth) using oblique sagittal and coronal Proton density-Weighted Imaging (PdWI) and (2) the maximum opened position of the mandible using oblique sagittal T2-weighted imaging (T2WI). The scanning parameters were as follows: (1) PdWI: TR/TE:1800.0/24.0, FOV: 10 cm × 10 cm, BW: 15.63 kHz, SL/SPACE: 2.0/1.0 mm, MATRIX: 320 × 192 and (2) T2WI: TR/TE: 3775.0/85.0, FOV: 10 cm × 10 cm, BW: 15.63 kHz, SL/SPACE:1.5/0.5 mm, MATRIX: 320 × 192 [7].
Dynamic oblique sagittal images were acquired separately during opening-closing movement by 1-, 2-, 3-, 4-, 5-, and 6-cm thick slices with varying spatial and temporal resolutions. Dynamic fast imaging employing steady-state acquisition MRI was performed at a median oblique sagittal location that was perpendicular to the long axis of the head of the mandibular condyle. The subjects were instructed to move continuously by slowly and freely opening and closing their mouths during this process. The parameters for dynamic, fast imaging employing steady-state acquisition MRI were as follows: SL/SPACE: 5 mm/1 mm, FOV: 18 cm × 18 cm, MATRIX: 256 × 256. Sixty continuous images of the TMJ movement were obtained with the FIESTA MRI system over 90 seconds.
The articular disk was directly identified in sagittal oblique T1-weighted images as an area of hypointensity with a biconcave shape above the condylar structure, and its position was categorized according to available data [13-15]. (1) Superior (normal) disk position: posterior band of the articular disk located above the apex of the condylar head (at the 12 o’clock position) in both the closed-mouth and maximum open-mouth positions. (2) Disk displacement with reduction: posterior band of the disk located anteriorly to the condylar head in the closed-mouth position but a normal disk-condyle relationship established in the maximum open-mouth position. (3) Disk displacement without reduction: posterior band positioned anteriorly to the condyle in both the closed-mouth and maximum open-mouth positions.
2.4. ARCUSdigma System Recordings
Each study participant underwent mandibular kinesiography with a commercially available device (ARCUSdigma, KaVo) [16]. Each participant was seated on a high-backed chair with their head upright and looking ahead. The kinesiographic recordings were made with the use of a magnet temporarily applied on the subject’s buccal mucosa under the lower arch of the central incisors to monitor the location of the mandible relative to a sensor array suspended in front of the face from a lightweight frame suspended on the bridge of the nose and connected behind the head by straps. All tasks were performed 3 times at 10-minute intervals, and the average value of the 3 attempts was recorded.
2.5. Statistical Analysis
Data were statistically analyzed using SPSS 11.5 (SPSS Inc.; Chicago, USA). Count data were compared using Chi-square tests, and p < 0.05 was considered statistically significant. Measurement data were expressed as the mean plus or minus the standard deviation (x ± s). Data were compared among multiple groups using analysis of variance, and data were analyzed between two groups using t-tests. A p < 0.05 was considered statistically significant.
3. RESULTS
Thirteen of 15 subjects with asymptomatic TMJs were evaluated as normal using MRI. Two of the 15 subjects with asymptomatic TMJs had unilateral ADDWR on the basis of MRI. Fourteen cases of unilateral ADDWoR were seen in Group Ш using MRI (Table 1).
| – | MRI Findings | ARCUSdigma Findings | |||
|---|---|---|---|---|---|
| Diagnosis | Symptomatic Joints (Subjects) | Asymptomatic Joints (Subjects) | Sign of Condylar Trace | Symptomatic Joints (Subjects) | Asymptomatic Joints (Subjects) |
| Normal TMJ | 0 (0) | 13 (15*) | Smooth and reproducible | 0 (0) | 13 (15*) |
| ADDWR | 17 (17) | 2 (2) | Bounce and deviate in a typical “figure eight” | 17 (17) | 2 (2) |
| ADDWoR | 14 (14) | 0(0) | Short and curved shape | 14 (14) | 0(0) |
| Total | 31 | 15 | Total | 31 | 15 |
3.1. Cine-MRI of Normal TMJs
MRI clearly identified discs, condylar position and morphology, articular surfaces, and correct disc-condyle relationships. Normal discs were directly identified in sagittal, oblique T1-weighted images as an area of hypointensity with a biconcave shape above the condylar structure, and its posterior band was located above the apex of the condylar head (at the 12 o’clock position) in both closed-mouth and maximum open-mouth positions.
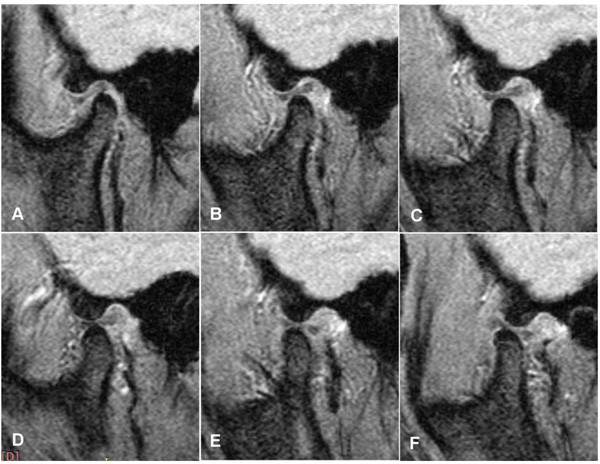
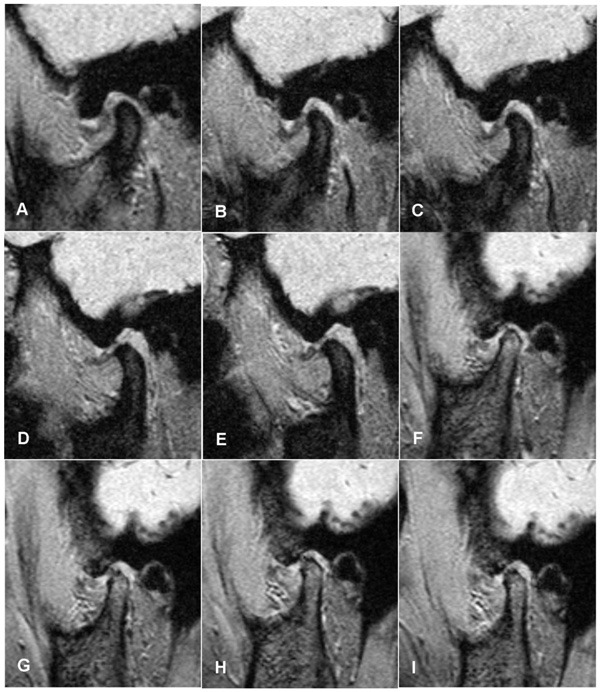
The Cine-mode recordings of the subjects with normal TMJs showed a rotational condyle distance within 2.0 cm during the early phase of mouth opening. Over the distance between 2.0 cm and 4.0 cm, condylar movement showed a continuous translation under the apex of the articular eminence. When keeping the mouth open at 5.0 cm, there was the onset of condylar rotation and loss of condylar, and the condyle was then located in a slightly pre-tubercular position (Fig. 1).
3.2. ARCUSdigma Recordings of Normal TMJs
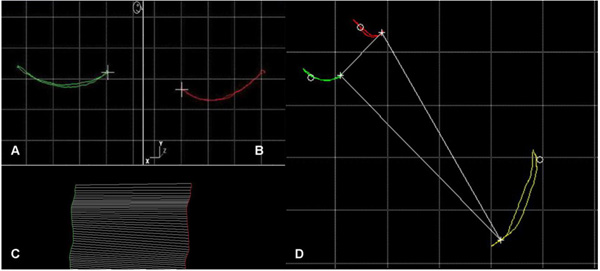
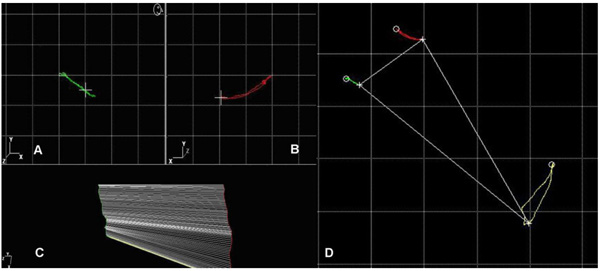
The condylar trace of normal TMJ was smooth and reproducible, with no deflections. No clicking sounds were recorded. Fig. (2) is a typical example of the kinematic center of condylar movement traces of a normal TMJ. Sagittal condylar traces (green: left, red: right) are harmonic, with reproducible cycles for opening and closing jaw movements. The deviation of the excursive from the incursive line (yellow) was slight (< 5 mm). The intercondylar axis remained parallel and clustered at the end of the recording of the opening/closing cycle (lower left in Fig. (2)).
3.3. Cine-MR Imaging of ADDWR TMJ
Subjects with early ADDWR showed an abrupt change in the disc-condyle relationship during mandibular rotation. The rapid changes in spacing between subsequent condylar positions show the sudden accelerations and decelerations experienced during recovery of the normal disc-condylar relationship. The dislocated disc was reduced initially or intermediately during mouth opening. The range of mandibular motion was usually not limited. Joint clicking was found at different stages of mouth opening. Dynamic image simulation of the entire opening-closing movement was performed, and the more backward and upward shift in condylar position in the glenoid fossa, and the rotation period were reset to the beginning of the period between the start and end of the opening-closing movement simulation (Fig. 3).
3.4. ARCUSdigma Recordings of TMJs with ADDWR
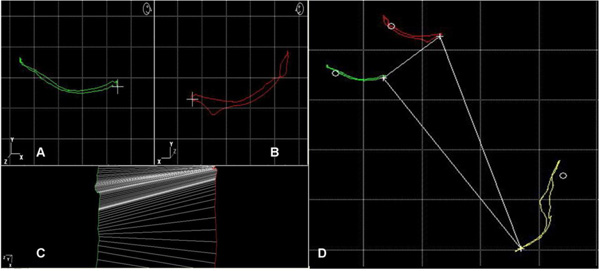
Condylar and incisal point trajectories with unilateral ADDWR appeared to bounce and deviate, forming a typical “figure eight”. The deviation of the excursive from the incursive line was significantly increased (>5 mm). The intercondylar axis became non-parallel for the ipsilateral condyle with ADDWR. However, the condylar trajectory of the unaffected side showed smooth and reproducible movements with no deflections (Fig. 4). The deflections coincided with the occurrence of the clicks.
3.5. Cine-MR Imaging of TMJs with ADDWoR
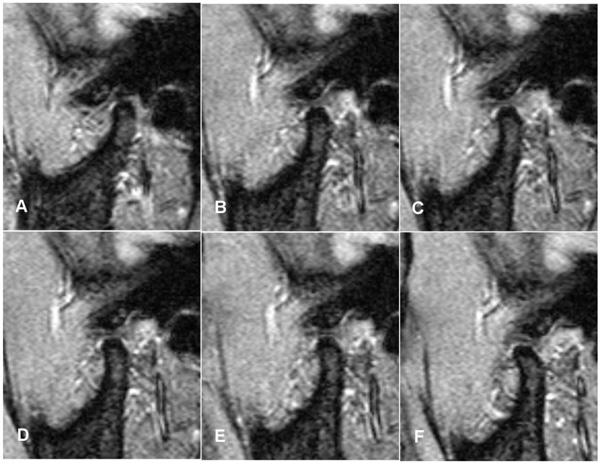
Disc morphology displayed a biplanar, even thickness, and the disc was folded. The more severe the degree of anterior disc displacement, the worse the backward and upward shift of the condylar position in the glenoid fossa. The disc was completely in front of the condyle, and the anteriorly located disc was pushed further forward during condylar excursions. Changes in disc position and morphology were seen by MRI during translational movement of the condyle, which compressed the anteriorly dislocated disc (Fig. 5).
3.6. ARCUSdigma Recordings of TMJs with ADDWoR
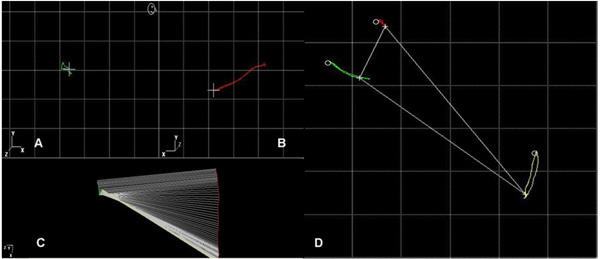
The condylar movement of the TMJs with ADDWoR was limited, and the trajectory showed a significantly shorter range of TMJ movement that was observed in the contralateral TMJ. In the chronic phase (over 6 months), the range of TMJ motion was not significantly limited (Fig. 6). In the acute phase (within 6 months), mandibular movements were painful, and mouth opening was limited with deviation to the affected side (Fig. 7).
3.7. Occlusal Index
The mean occlusal indices of normal, ADDWR and ADDWoR groups (range of incisal and condylar trajectories during opening movements) are shown in Table 2. Student’s t-tests were conducted at a level of significance of p<0.05. A significant difference between individuals with ADDWoR and normal TMJs was found for the lengths of condylar and incisal trajectories during opening-closing movements p<0.01. A significant difference between individuals with ADDWoR and ADDWR was found for the lengths of the condylar and incisal trajectories during opening-closing movement (p<0.01) (Table 3).
| - | Condylar Trajectory Range |
Incisal Trajectory Range |
|---|---|---|
| Normal (n=13) | 13.2±3.1 | 41.1±3.8 |
| ADDWR (n=19) | 13.9±5.1 | 38.7±6.1 |
| ADDWoR (n=14) | 5.7±3.5 | 24.1±5.4 |
| - | Condylar Trajectory Range | Incisal Trajectory Range | ||
|---|---|---|---|---|
| - | t | p | T | p |
| ADDWoR*Normal | 10.109 | <. 001 | 6.324 | <.001 |
| ADDWoR*ADDWR | 6.792 | <.001 | 5.081 | <.001 |
4. DISCUSSION
Normal TMJ discs are double-concave, and the shape of the discs with anterior displacement can change. In this study, two subjects with asymptomatic TMJs had unilateral ADDWR identified using MRI. The small degree of deformation of the disc included thickening and swelling. However, this small degree of deformation of asymptomatic ADDWR still affected condylar tracing during opening-closing movements. ARCUSdigma is a sensitive instrument that can be used to record the condylar traces of asymptomatic TMJs with ADDWR. The results of this study show that healthy and symptom-free subjects with ADDWR have similar incisal trajectories. Other studies have reported that deviation of the incisal trajectory in symptom-free subjects with ADDWR is only 0.2-3.8 mm during opening-closing movements and the deviation angle is approximately 6 degrees. Hence, it is difficult to detect this deviation in clinical examination [17, 18]. These results suggest that the former minimally displaced discs did not cause a significant change in the incisal trajectory during opening-closing movements [19].
For the ADDWR group, Cine-MRI showed that internal derangement had a crucial influence on condyle movement during early rotation but not during translation. Cine-MRI is particularly useful for observing abrupt changes in the disc-condyle relationship during early rotation in individuals with ADDWR. The rapid changes in spacing between subsequent condylar positions show the sudden accelerations and decelerations experienced during the recovery of a normal disc-condylar relationship. ARCUSdigma also showed a typical “figure eight” pattern for condylar tracing when the disc returned back to the normal disc-to-condyle relationship. Additionally, sudden-onset variations in speed coincided with the occurrence of a typical “figure eight” pattern and clicking. In the unilateral ADDWR group, Cine-MRI showed three different condylar positions in the maximal opening position. First, the disc-condyle position was directly below the apex of the eminence. Second, the disc was directly below the apex of the eminence, but the condyle moved slightly before the apex of the eminence. Third, the disc-condyle position was obviously located before the apex of the eminence, which is referred to as hypermobility. In the third case, the clicking sounds occurred at the end of the opening and/or at the beginning of closing, and jerky lateral mandibular movements were observed. The interference may be due to a condylar dislocation before the crest of the eminence. In this study, there were 2 cases of condylar hypermobility in subjects with ADDWR, and the pterygoid muscle on the lower portion of the head of the condyle showed pathological changes. The large elastic fibers in the upper part of the pterygoid muscles and the upper plate of the articular disc act as a pair of balancing devices that maintain a normal relationship between the condyle and disc during exercise [20, 21]. With condylar hypermobility, the elastic fibers of the double-plate area are stretched harder to maintain the relative stability of the disc-condyle position. In TMJ hypermobility, the condylar ridge thrusts to the crest of the eminence and elongates the elastic fiber of the disc [22-24]. ARCUSdigma showed a typical “down polyline” in the condylar tracing. With condylar hypermobility and the repeated over-stretching of the disc, the pterygoid muscle is always under tense contraction. When the pterygoid muscle shows pathological changes, becomes out of balance, which causes the TMJ capsule to loosen and open too wide.
According to clinical diagnoses, ADDWoR can be divided into acute and chronic phases, which are within six months (acute) and over six months (chronic), respectively [25]. In this study, we found two different condylar movements patterns in the two ADDWoR phases. One involved significantly limited condylar movement. During the opening movement, the displaced disc was pushed further forward by the condyle. Then, the deformation of the articular disc increased. These patients were in significant pain and had limited movement during opening (20-25 mm). Due to the bilaminar zone being rich in blood vessels and nerves, there were clinical symptoms of joint pain during opening and an abnormal squeezing feeling, causing the patient to limit mouth opening.
The other range of condylar movement in the other pattern was near normal. The formerly displaced disc hindered the condyle from continuing forward, and the condyle then made a compensatory rotation. Because of this compensatory rotation in the affected joint, the affected trace bent down at the end of mouth opening. These patients did not have obvious pain and had limited movement in mouth opening, and the course of ADDWoR lasted more than a year. We speculated that the double-plate area and the joint capsule began to relax when the symptom of ADDWoR transferred from the acute to the chronic phase. This change would explain why this patient type has an increased opening index. Hence, the increased opening does not present as pathology of the deformed disc because displacement has been reduced, and the condylar movement has returned to normal. The effectiveness of using the distance of mouth opening as a clinical indicator to assess the degree of displacement should be questioned [26]. However, in some subjects, the anteriorly dislocated disc mechanically prevented the condyle from moving through its full forward excursion. In this closed-lock derangement, the subject was not able to fully open their mouth.
CONCLUSION
This study assessed the correlation between TMJ disc and condyle position, as depicted by Cine-MRI, and features of mandibular movement. The accuracy of the ARCUSdigma parameters in predicting condylar tracing is acceptable. Data from this study can be used as a good predictor for functional signs of internal derangement of the TMJ.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by Ethics Committee of Affiliated Hospital of Stomatology, Sun Yat-Sen University.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2008.
CONSENT FOR PUBLICATION
Written and informed consent was obtained from all participants before the study started.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
This work was supported by the National Natural Science Foundation of China (Project Numbers: 81201201 and 81472928), the Medical Science Foundation of Jiangsu Provincial Health Department (Project Number: H201641), the Jiangsu Provincial Medical Youth Talent (Project Number: QNRC2016850), and the Southeast University-Nanjing Medical University Cooperative Research Project (2242017K3DN14).


