All published articles of this journal are available on ScienceDirect.
The Influence of Impression Material on the Accuracy of the Master Cast in Implant Restorations
Abstract
Aim:
The precise framework fit is important for the success of implant restorations. The purpose of the present study was to examine the effect of two different impression materials both of their medium viscosity on the master cast accuracy when parallel and inclined implants were used.
Materials and Methods:
An epoxy master cast with three implants was fabricated. The first two implants were parallel to each other and perpendicular to the horizontal plane and the third implant had a 250 inclination in reference to the other two. A passively fitting metal framework that was fabricated over this master cast was used to measure accuracy of fit. Five closed tray impressions for each medium viscosity material (polyether and polyvinyl-siloxane) tested were taken and the respective ten stone casts with three implant analogs were fabricated. The metal framework in the master cast, was fixed in the new specimens and the micro-gap between this prosthesis and the implant analogs was evaluated. The specimens were observed to an optical microscope and digital photography.
Results and Conclusion:
The data were statistically analysed using a computer software and t-test. Polyether exhibited higher micro-gap mean values (93,4 to 61,8 μm) compared to polyvynil siloxane (30,47 to 14,83μm). The differences were statistically significant only for implant B. The categorical regression analysis (p < 0.01) for all implants showed that the marginal micro-gap was affected by the impression material (94.1%) and significantly by the type of it. The micro-gap values were higher for polyether compared to polyvinyl-siloxane. The torqued implant did not exhibit any statistically significant effect.
1. INTRODUCTION
The use of osseointegrated implants for the restoration of fully or partially edentulous patients has become a widely accepted treatment during the past decades [1-11]. From the technical point of view the goal is the fabrication of prosthetic superstructures that fit passively on the implants [7-9, 12-21] The rigid connection of a Fixed Partial Denture (FPD) to the implants results in a clinical situation where implants, abutments, superstructure and supporting bone act as a single unit [13, 22, 23].
The lack of passive fit combined with the absence of periodontal ligament around the implants, may be the cause of severe problems to the surrounding bone as well as failures to the implants or the prosthetic device [23]. Thus, oral rehabilitation should be initiated with adequate and individualized prosthodontic treatment planning for each clinical situation to provide satisfactory aesthetics and function once the prosthesis is fixed on the implants [23].
Differing from the natural teeth that have a buccal-lingual mobility of 56-108 μm, osseointegrated implants are ankylosed to the bone and have no periodontal ligament to compensate for any inaccuracy, showing a minimal mobility (10 μm) due to the elasticity of bone tissue [2, 9, 11-13, 15, 22, 24, 25]. Consequently, recording the intraoral three-dimensional implant position is critical in the realization of implant-supported prostheses to ensure an accurate relationship on the master cast [4, 7, 8, 12, 16, 17, 20, 23, 26-29].
An inaccurate impression may lead to biological and laboratory problems as a result of the prosthesis’ misfit, or even affect the surrounding tissues [2, 7-9, 12, 17-19, 25-27, 30]. Mechanical complications that might arise from non-passive include screw or abutment loosening, screw-, abutment- or implant fracture and occlusal inaccuracy [2, 6, 7, 9, 12, 16-19, 26, 28, 30-32]. Marginal discrepancy occurring as a result of misfit may also increase plaque accumulation and affect the soft and/or hard tissues around the implant [6, 8, 12, 16, 25, 27, 28, 31].
In the daily clinical practice it is difficult or practically impossible to achieve absolute passive fit and the response of bone tissue around implants supporting ill-fitting prostheses remains controversial. Therefore, the impression accuracy of the implants and the proper construction of the master cast remains an important factor for the clinical life of implants.
Most of the existing studies have described various impression techniques, without a solid conclusion as to which technique is preferable. The construction of an implant restoration with an ideal passive fit is difficult because of the numerous clinical and laboratory stages, but also due to the increased number of materials and components that used during fabrication [5, 7-10, 26, 28, 31-34].
Most authors consider the passive fit of the prostheses as an advantageous factor for the long-term serviceability of the restorations. As a consequence, the importance of an accurate impression, concerning the technique and the impression material is paramount [7, 8, 10, 14, 26, 27, 29, 31, 34-36]. The impression materials that are widely used for implant restorations are addition type silicones (polyvinyl siloxane) and polyether. The critical question is whether Polyvinyl Siloxane (VPS) or polyether offer increased accuracy in implant impressions.
2. AIM
The purpose of this study was to examine the effect of two different impression materials on the accuracy of the master cast with parallel and inclined implants. The impression materials used were medium viscosity polyvinyl siloxane and polyether with closed tray. The null hypothesis was that there would be no differences in the accuracy of casts produced from impressions made of different impression materials.
3. MATERIALS AND METHODS
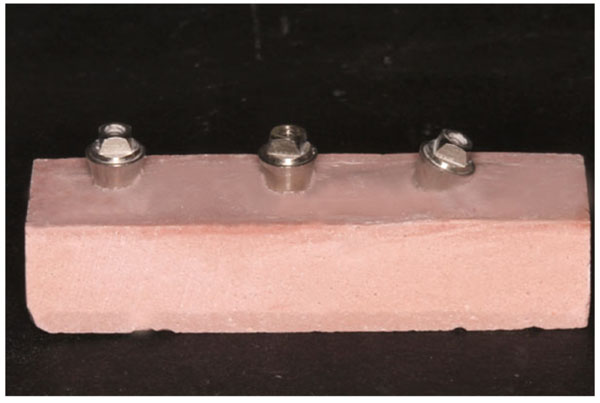
An epoxy resin master cast was fabricated utilizing three 3,4 mm diameter external connection dental implants (Xive TG, Friadent/Dentsply Co, Mannheim Germany). The implants were embedded in the epoxy resin with the use of an electronic paralleling device (Fig. 1). Two implants (implants A, B) were placed perpendicularly to the horizontal plane and parallel to each other (0 degree inclination), while the third implant (implant C) was placed with a 25 degree inclination to the vertical plane. Although a CAD/CAM constructed framework would have been more precise, it was decided to construct and measure a waxed metal framework, in order to be more realistic to everyday dental practice.
A screw-retained metal framework was waxed, sprued and cast from a Co-Cr base metal alloy. After casting, the framework was cut, fit and soldered in order to achieve passive fit over the implants (Fig. 2). The fit of the framework was examined under magnification under a microscope with magnification 40x. This framework was used as reference point for comparisons and as control. The framework was initially screwed on the first implant analog (implant A) with a torque of 20 Ncm. The resulting initial micro-gap was measured at the implant-analog surface for implants B and C with the use of an optical microscope (Leica Microsystems, Wetzlar Germany) and pictures of the fitting surfaces of all the analogs were taken at a standardized magnification of 40X. The framework was later fixed by the retaining screw on the inclined analog (implant C) and the fit was accordingly evaluated on the other two implants (implants A and B). These initial micro-gap values were recorded for each specimen, in order to be used for the calculation of the final micro-gap value.


Five non-parallel orientation grooves (2 mm deep) were created on the sides of the master cast surface using rotary instruments to allow precise orientation of the custom tray. A light-polymerizing resin tray material (Triad, Dentsply Co, Frankfurt Germany) was used for the fabrication of two custom impression trays, one for each impression technique tested.
Closed-tray transfer copings (Xive TG Impression Posts D 3, 4-4, 5 mm, Friadent/Densply Co, Mannheim Germany) were connected to the implants on the epoxy resin cast. Impression material thickness consistency was ensured by injecting exactly 15 ml of bite registration addition silicone material (Exabite™ II NDS, GC America Inc.) around the copings and 35 ml of it inside the trays, creating a consistent 2 mm space.
A photopolymerizing resin tray material (Triad, Dentsply Co, Frankfurt Germany) was used for the fabrication of two custom impression trays, one for each impression material tested. The tray material was positioned over the copings and the silicone and carefully packed onto the master cast up to complete engagement of the orientation grooves. Light-polymerization was performed in a light curing device (Triad 2000 Visible Light Curing Unit, Dentsply Co, Frankfurt Germany) for 6 minutes. Following polymerization the trays were stored at room temperature (230 ± 10C) and humidity (50 ± 10%) for 24 hours according to manufacturer’s instructions. The same custom tray was used for all the five impressions of each group in order to avoid discrepancies of thickness of the impression materials. The respective tray adhesive material (Polyether Adhesive, 3M/ESPE AG, Seefeld Germany and Silfix, Dentsply GmBH, Konstanz Germany) was applied on the inner surface of each custom tray and allowed to dry for 30 minutes.
For the purposes of this study, a polyether (Impregum Penta™ (3M/ESPE Co) and polyvinylsiloxane impression material (Aquasil Ultra Monophase, Densply Co) both of medium viscosity, were used. Closed tray transfer copings (Xive TG Impression copings, Friadent/Densply Co) were connected to the implants with a 20 Ncm torque, according to the manufacturer’s instructions. The same custom tray was used for all the five impressions of each material. The respective tray adhesive material (Polyether Adhesive, 3M/ESPE AG and Silfix, Dentsply GmBH) was applied on the inner surface of each custom tray and allowed to dry for 30 minutes.
The polyether impression material was mixed in a special automixing device (Pentamix™ 2, 3M/ESPE AG) and syringed around the copings (total volume: 50 ml), while the tray was loaded and positioned in order to engage the orientation grooves. The tray was held with finger pressure until completion of polymerization. The polyvinyl siloxane was mixed with a hand held mixing pistol and syringed around the posts (total volume: 50 ml). The tray was filled with impression material, positioned and held in the same manner.
Ten impressions, five for each tested material, were made (Fig. 3). The impressions were visually inspected for the presence of bubbles or other deficiencies and stored at room temperature (230 ± 10C) and humidity (50 ± 10%) for 24 hours. They were washed with tap water for 10 seconds and dried with an air stream.

The transfer copings were removed from the epoxy resin cast, connected to external hex implant analogs (Xive TG Implant laboratory analogs, Friadent/Densply Co, Mannheim Germany) and the hand tightened coping-analog assembly was repositioned in the retentive features in the impression material. The copings were checked for stability and absence of rotational movement. The new master casts were fabricated using hard dental stone. Type IV die stone material (Silky Stone, WhipMix Co, Louisville, KY, USA) was mixed with water in the ratio suggested by the manufacturer in a vacuum mixing device (Whip Mix Combination Unit, WhipMix Co, Louisville, KY, USA) for 30 seconds. The mixed stone was poured in the impressions and allowed to set for 24 hours. Five specimens (stone casts), each containing three implant analogs, were fabricated for each material tested (1S-5S and 1P-5P) (Fig. 4).
The resulting micro-gaps were evaluated using the passively fitting cast framework that was fabricated on the initial epoxy resin master cast on each implant for every specimen. The framework was initially screwed on the distal perpendicular analog (Implant A) with a torque of 20 Ncm (Fig. 2). The resulting micro-gap was measured at the implant-analog surface with the use of an optical microscope (Leica Microsystems, Wetzlar Germany) and pictures of the fitting surfaces of all the analogs were taken at a standardized magnification of 40X (Figs. 5-7). Six pictures were taken at the contact surfaces of each implant analog, two at each of the mesial, distal and labial analog surfaces. The pictures were analyzed with the use of a software program (Adobe Photoshop CS4, Adobe Systems, California, USA).
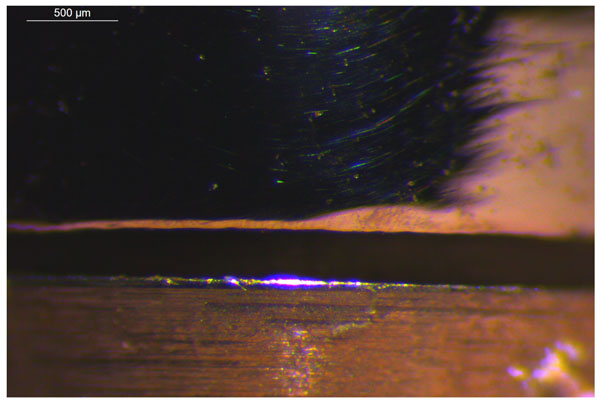
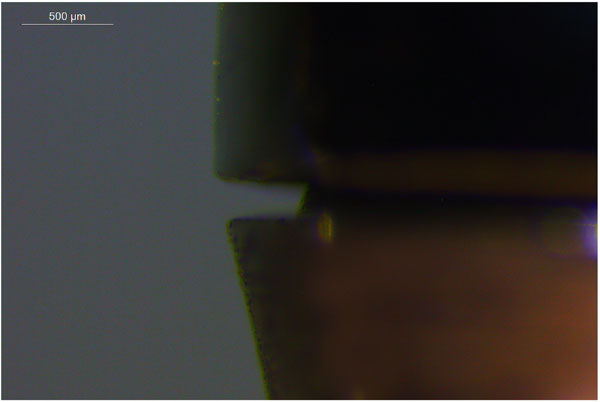
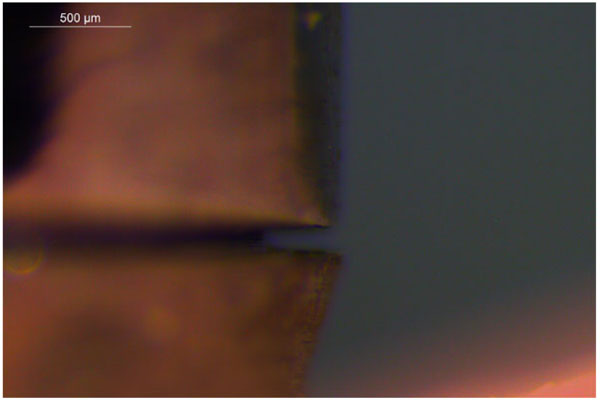
For each picture two points, one at the outermost point of the metal framework and one at the corresponding edge of the analog were selected and the distance between them was measured by means of the reference bar depicted on the screen as the photo was projected by the software program. Three measurements for each picture were performed and their mean value was calculated in μm (Figs. 5-7). The three surfaces of each analog were evaluated and a general mean value (g mean) was calculated for the micro-gap on each implant. Since the fixing of the framework by tightening the screw on the most distal perpendicular implant (Implant A) resulted in the elimination of the micro-gap on this particular implant, only the measurements of the non-screwed implants were used (Implants B and C). The framework was afterwards screwed on the inclined analog (Implant C) and the fit was evaluated in the same way on the other two implants (Implants A and B).
The fit of the preexisting metal framework had already been evaluated accordingly. The framework was fixed by the screw in a similar manner on the epoxy resin cast (reference cast) at 20 Ncm and its fit was also measured. The resulting values of the micro-gap on the epoxy resin cast were considered as a “tare” value and were subtracted from the corresponding values measured on the specimens (casts) made from polyether or silicone impressions.
The data of the micro-gap values were statistically evaluated by ANOVA and Categorical Regression analysis with the use of statistical software programs (SPSS 13.0, Statistica).
4. RESULTS
The overall results from the measurements of the gap (gmean) at the implant-framework interface are presented in Diagram 1. Differences were noted concerning the general mean value of the micro-gaps for the three implants and the two impression materials. Polyether exhibited higher micro-gap general mean values when compared to polyvynil siloxane. For each implant the micro-gap values for polyvynil siloxane and polyether were compared using the t-test. The differences were statistically significant only for Implant B. This might be attributed to the fact that there had been no zero measurements for Implant B, since the framework was torqued either on Implant A or C. As a result, micro-gap values for Implant B were present on all measurements. On the contrary, micro-gap measurements of zero value for Implants A and C were present when the framework was tightened on the corresponding implant, a fact that affected the resulting micro-gap general mean.

In Diagram 2 the tests of between subjects (implants and impression materials) effects on the marginal micro-gap between the implant analog and the metal framework are presented. A statistically significant difference concerning only the factor “impression material” was found (p < 0.01). The factor “torqued implant” did not exhibit any statistically significant effect on the impression accuracy.
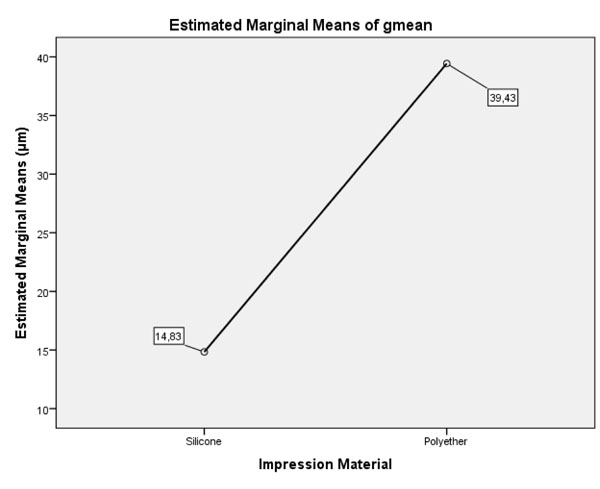
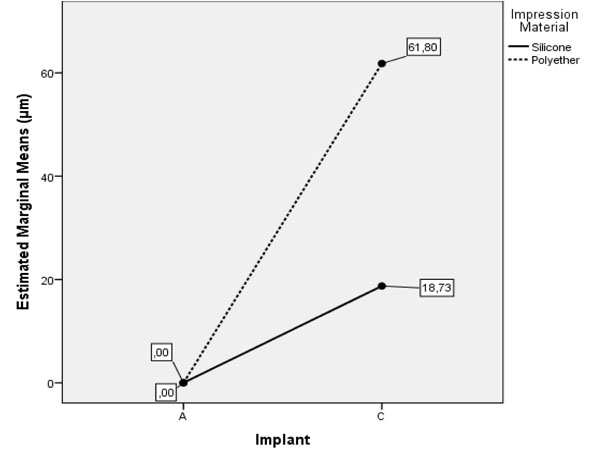
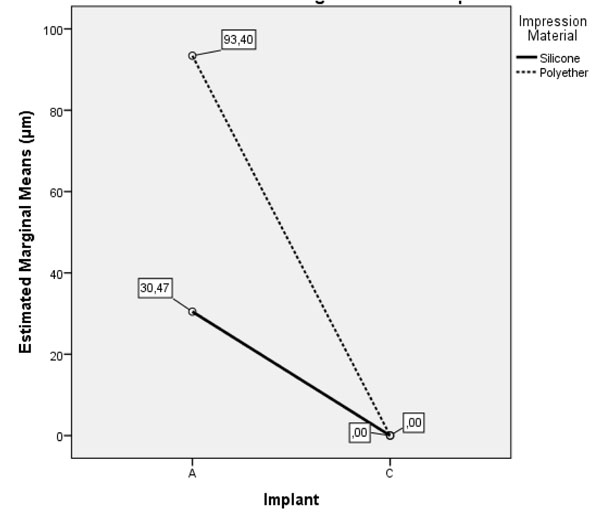
Diagram 3 depicts the general mean values of the micro-gap at the framework-analog interface for all implants. For silicone impressions the micro-gap between the prosthesis and the analogs was 14,83 μm and when polyether was used, the micro-gap between the above surfaces was 39,43 μm, no matter which implant was torqued. Diagram 1 depicts the mean value of the micro-gap on implant C when the framework was tightened on implant A. As expected, the micro-gap in Implant A was zero for both impression materials. The mean values for silicone was 18.73 μm and for polyether 61.8 μm (F = 5.079), (p < 0.05). In Diagram 4 the mean value of the micro-gap on implant A is presented, when the framework was tightened on implant C. As expected, the micro-gap in Implant C was zero for both impression materials. The mean values for silicone was 30.47 μm and for polyether 93.4 μm (F = 5.30), (p < 0.05).
A categorical regression statistical analysis was performed in order to further investigate the effect between the two predicting factors (predictors), the impression material (polyvinyl siloxane or polyether) and the torqued implant (A or C). This analysis indicated the impact of each factor on the examined dependent variable (micro-gap) (Tables 1-4). It may be observed that the impression accuracy was mostly affected by the impression material (94.1%) and significantly less by the torqued implant (5.9%).
| Tests of Between-Subjects Effects | |||||
|---|---|---|---|---|---|
| Source | Type III Sum of Squares | df | Mean Square | F | Sig. |
| Corrected Model | 3565,240a | 3 | 1188,413 | 4,439 | ,019 |
| Intercept | 14724,356 | 1 | 14724,356 | 55,005 | ,000 |
| impr_mater | 3025,800 | 1 | 3025,800 | 11,303 | ,004 |
| implant | 341,689 | 1 | 341,689 | 1,276 | ,275 |
| impr_mater * implant | 197,751 | 1 | 197,751 | ,739 | ,403 |
| Error | 4283,072 | 16 | 267,692 | - | - |
| Total | 22572,667 | 20 | - | - | - |
| Corrected Total | 7848,311 | 19 | - | - | - |
| ANOVA | |||||
|---|---|---|---|---|---|
| - | Sum of Squares | df | Mean Square | F | Sig. |
| Regression | 6,476 | 2 | 3,238 | 4,070 | ,036 |
| Residual | 13,524 | 17 | ,796 | - | - |
| Total | 20,000 | 19 | - | - | - |
| Coefficients | |||||
|---|---|---|---|---|---|
| - | Standardized Coefficients | df | F | Sig. | |
| Beta | Bootstrap (1000) Estimate of Std. Error | ||||
| Impression Material | ,552 | ,150 | 1 | 13,578 | ,002 |
| Implant | ,138 | ,132 | 1 | 1,085 | ,312 |
| Correlations and Tolerance | ||||||
|---|---|---|---|---|---|---|
| - | Correlations | Importance | Tolerance | |||
| Zero-Order | Partial | Part | After Transformation | Before Transformation | ||
| Impression Material | ,552 | ,557 | ,552 | ,941 | 1,000 | 1,000 |
| Implant | ,138 | ,166 | ,138 | ,059 | 1,000 | 1,000 |
5. DISCUSSION
The purpose of this study was to examine the effect of two different medium viscosity impression materials on the accuracy of the master cast with parallel and inclined implants using the closed tray impression technique. The null hypothesis was that neither type of impression material (polyether and polyvinyl siloxane) would affect the framework fit. On the basis of the recorded data and the evaluation of the results, the null hypothesis was rejected. Both materials had a significant effect on the accuracy of the experimental casts, both for parallel and inclined implants.
A standard amount of medium viscosity polyether and polyvinyl siloxane impression materials were used with the closed tray technique. The innovations in this study were the use of an optical microscope and a software to measure the micro-gap between a restoration and the implant analogs and the use of medium viscosity impression materials.
Baig et al., [37] in an extended literature review covering a 20 year period, showed that silicones and polyether were the preferred materials for implant impressions. 59 studies were selected in total for evaluation and 15 studies compared polyvinyl siloxane and polyether. Among them 11 studies found no differences between the two materials in terms of impression accuracy, in contrast to our study, where differences existed. 30 studies analyzed the splint effect, 13 found splinting of the impression post resulting in greater accuracy and 13 others elicited no differences between splinting and non-splinting of the posts. In 12 studies the implant inclination was examined as a factor influencing the impression accuracy and found significant differences in accuracy for inclinations reaching 200-250 and this finding is in accordance with the results of the present study. Finally, among the 25 studies examining pick-up (open- tray) and transfer (closed tray) impression techniques, 12 favored open tray over closed- tray impression, especially with increased numbers of implants. In the present study only the closed- tray technique was examined.
Lee et al., [31], in a systematic review investigated the accuracy of impression techniques and materials for implants. Of the 41 articles that were included, 14 compared the accuracy of closed and open tray impression techniques. Of the 14 studies, 5 showed more accurate impressions with the non-splinted open-tray technique, 2 with the closed-tray technique and 7 showed no difference between them.
In the closed-tray technique the impression copings remain fixed on the implants after the removal of the impression. The transfer of the impression copings from the mouth to the implant analogs and their repositioning to the impression material on the tray may induce inaccuracy, because they may not be exactly seated to the original position. This is believed to be the primary source of error of this technique, especially when more than 4 implants were examined [38]. In the present study 3 implants were used in order to minimize the risk of false positioning of the impression copings and the resulting inaccuracy of the master cast.
Eleven of the studies reviewed by Lee et al. [31], compared the accuracy of polyether and polyvinyl-silicone impression materials. In ten of them no difference between the 2 materials was reported and only 1 showed greater accuracy of the impressions with polyvinyl siloxane. This result was probably related to the impression materials and their accuracy, concerning the implant position. Lee et al., [28], in an experimental in-vitro study investigated the effect of impression material on the accuracy of the cast. Open tray impressions were made on a stone master model that was fabricated with 5 implant analogs embedded parallel to each other and placed in different depths below the model’s surface. Medium-body polyether or a combination of putty and light-body polyvinyl siloxane was used as impression materials. Horizontal and vertical distances were measured with a microscope and it was concluded that polyvinylsiloxane was more accurate [28].
6. LIMITATIONS
A possible limitation concerning the design of the present study was the fact that a not so precise waxed metal framework (comparing to a CAD/CAM framework) was used for the measurements, in order to be more realistic concerning what happens to everyday dental practices. Another important limitation was that the evaluated micro-gaps between the prosthesis and the implant analog were not depicted 3-dimensionally (3D), but in 2 dimensions.
Assessment of the distortion occurring in working casts produced by different impression has been investigated using a variety of methods [39] These include stereophotogrammetry, reflex microscopy, laser interferometry, scanning electron microscopy, microtomography, confocal microscopy and mechanical digitisers. For dental applications, surface measurement sensitive to changes at the microns (μm) level is necessary and current methods involving the use of three-dimensional co-ordinate measuring machines are designed to meet these specifications [17, 22, 26, 35, 39, 40].
In the present study the microgap between the metal framework and the implant analogs was evaluated. The specimens were observed in an optical microscope from which photos were taken and analyzed using a computer software. Before that stage, impressions were prepared with medium-viscosity polyether and with Medium-Viscosity Silicone (VPS), contrary to all previous studies that used putty and light-body Polyvinyl-Silicones (VPS). That process imitates the common procedure in the dental practitioner’s everyday clinical life.
CONCLUSION
Within the limitations of this in-vitro study the following can be concluded:
○ Both impression materials significantly affected the accuracy of the casts, both for parallel and for inclined implants.
○ Polyether impressions exhibited significantly higher marginal gap values compared to polyvinyl-siloxane.
○ The marginal gap between implants and framework was affected mainly by the impression material and secondarily by the implant inclination or their interaction.
○ For inclined implants the casts resulting from polyvinyl-siloxane impressions were more accurate compared to the polyether impressions.
○ For both impression materials the micro-gap values of the inclined implants were significantly higher compared to the parallel implants. Implant inclination of 25 degrees may affect the accuracy of the resulting final cast.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Not applicable
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors thank Professor George Heliades, Director of the Biomaterials Department at the National and Kapodistrian University of Athens Dental School for his thorough help and support.


